Waking up to itchy red welts after a seemingly relaxing shower can be confusing—and distressing. For some, water itself becomes a trigger. Hives after showering are more common than many realize, and while they may seem harmless at first, recurring episodes can signal an underlying sensitivity or condition. Understanding the root causes, recognizing the types, and knowing how to respond can make all the difference in restoring comfort and confidence in daily routines.
What Triggers Hives After Showering?
Hives—also known as urticaria—are raised, red, itchy welts that appear when the body releases histamine in response to a perceived threat. While allergens like food or pollen are well-known triggers, physical stimuli such as heat, pressure, or even water can provoke reactions. In the context of showering, several factors may activate the immune system:
- Water temperature: Hot water dilates blood vessels and increases skin permeability, potentially worsening irritation or triggering histamine release.
- Chemical exposure: Shampoos, soaps, body washes, and even laundry detergents used on towels can contain irritants like sulfates, fragrances, or preservatives.
- Cholinergic urticaria: A form of hives triggered by body heat and sweating, often activated during or after warm showers.
- Aquagenic urticaria: A rare condition where hives develop within minutes of water contact, regardless of temperature.
- Hard water minerals: High levels of calcium and magnesium in tap water may disrupt the skin barrier, especially in those with sensitive or compromised skin.
Identifying which factor is responsible requires careful observation and sometimes medical evaluation. For many, the issue isn’t the water itself but what’s in it or how it affects the body.
Types of Hives Linked to Showering
Not all post-shower hives are the same. The specific type influences duration, appearance, and treatment approach. Below are the most common forms associated with bathing:
| Type | Trigger | Symptoms | Duration |
|---|---|---|---|
| Cholinergic Urticaria | Rise in body temperature from hot water or steam | Small, pinpoint hives; intense itching; possible flushing | 30–90 minutes |
| Aquagenic Urticaria | Contact with any form of water (rare) | Itchy bumps within 1–5 minutes of water exposure | 30–60 minutes after drying off |
| Contact Dermatitis (Irritant or Allergic) | Reaction to soaps, fragrances, or preservatives | Red, burning rash; may blister or peel | Hours to days, depending on exposure |
| Heat-Induced Physical Urticaria | Physical stimulus of warmth on skin | Large welts along areas exposed to heat | Less than 2 hours |
Distinguishing between these types helps determine whether the problem is environmental, immunological, or physical in nature. Cholinergic hives, for example, are more likely in younger adults and often linked to exercise or emotional stress—not just showers.
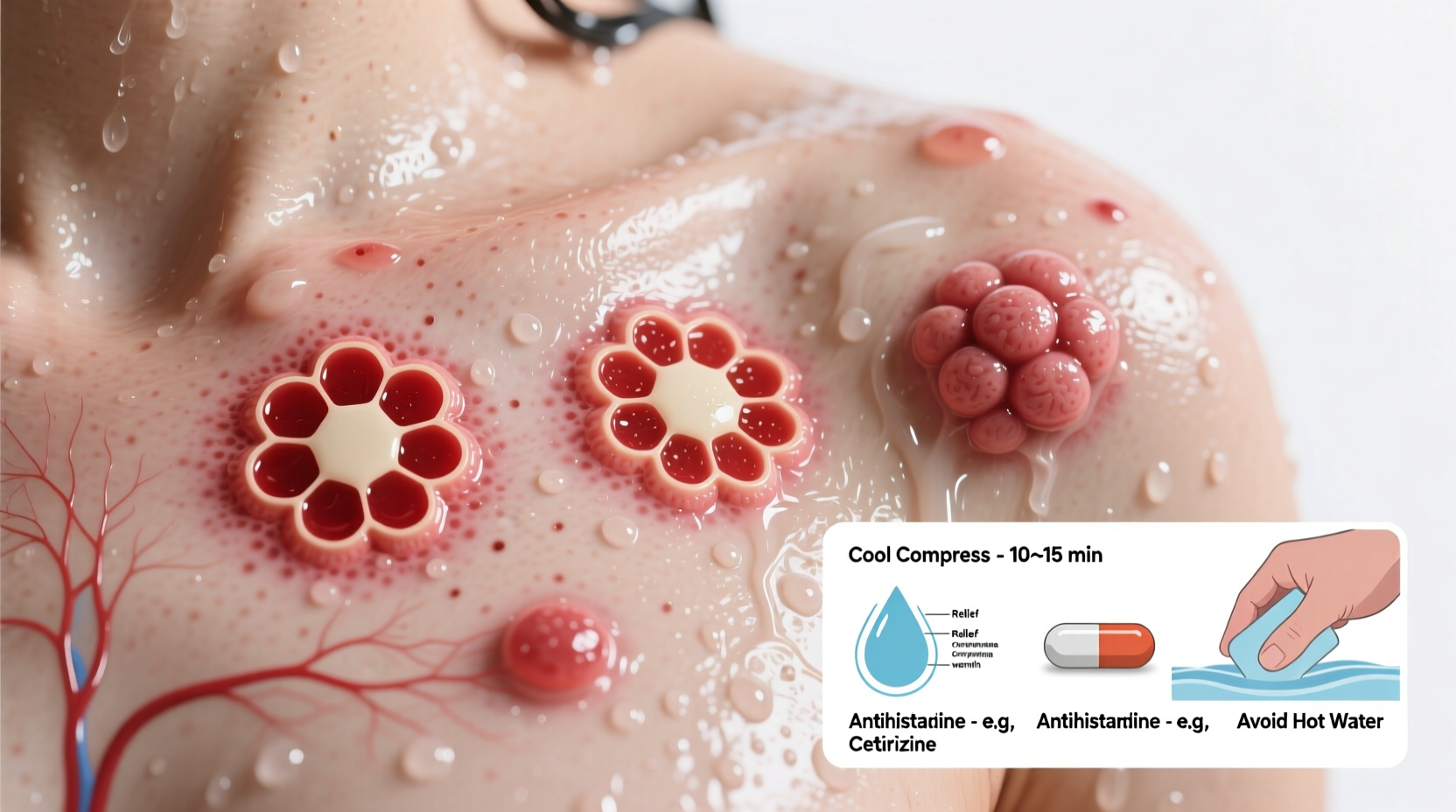
Relief Strategies and Immediate Actions
If you notice hives forming shortly after showering, immediate steps can reduce discomfort and prevent worsening:
- Cool down: Rinse the affected area with cool water or apply a cold compress to soothe inflammation.
- Stop using scented products: Immediately discontinue any new soaps, shampoos, or body scrubs introduced recently.
- Pat dry gently: Avoid rubbing with towels, which can further irritate sensitive skin.
- Take an antihistamine: Over-the-counter options like cetirizine (Zyrtec), loratadine (Claritin), or diphenhydramine (Benadryl) can block histamine and reduce itching.
- Moisturize: Apply a fragrance-free emollient like ceramide-based creams to restore the skin barrier.
For recurring cases, long-term adjustments are essential. Chronic hives lasting more than six weeks warrant consultation with a dermatologist or allergist.
“Many patients assume their hives are allergy-related, but physical triggers like heat or water contact are often overlooked. A detailed history is key to accurate diagnosis.” — Dr. Lena Torres, Board-Certified Dermatologist
Step-by-Step Prevention Plan
Preventing post-shower hives involves modifying habits, testing variables, and monitoring responses. Follow this timeline to identify and eliminate triggers:
- Week 1: Simplify your routine
Switch to fragrance-free, dye-free soap and shampoo. Use only one product at a time to isolate reactions. - Week 2: Adjust water temperature
Lower the shower heat to lukewarm. Limit showers to under 10 minutes to reduce skin exposure. - Week 3: Test water quality
Consider installing a shower filter to remove chlorine and heavy metals. Alternatively, collect water for a hardness test kit. - Week 4: Monitor clothing and towels
Wash bath linens with fragrance-free detergent. Avoid fabric softeners, which leave chemical residues. - Week 5: Track symptoms
Maintain a daily log noting shower duration, products used, water temperature, and hive occurrence. - Week 6: Consult a specialist
If hives persist, schedule an appointment with a dermatologist. Request patch testing or a methacholine challenge if cholinergic urticaria is suspected.
Real-Life Example: Managing Cholinergic Urticaria
Sarah, a 28-year-old teacher, began noticing small, intensely itchy bumps on her chest and arms every morning after her usual hot shower. At first, she blamed a new body wash, but switching brands didn’t help. The hives appeared even when she skipped soap entirely. After tracking her symptoms for two weeks, she realized the reaction occurred only when her skin felt warm—not cold or room-temperature showers triggered it.
She consulted a dermatologist who diagnosed cholinergic urticaria. Sarah was advised to lower her shower temperature, take antihistamines before exercise, and avoid sudden shifts in body heat. Within three weeks of cooler showers and daily loratadine, her outbreaks stopped completely. Her case highlights how subtle triggers can mimic allergies but respond best to lifestyle adjustments rather than medication alone.
Frequently Asked Questions
Can drinking water cause hives too?
No—drinking water does not trigger aquagenic urticaria. The condition only affects skin exposed to water externally. Internal consumption does not produce the same reaction.
Is it safe to continue showering if I get hives?
Yes, but modify your routine. Use lukewarm water, gentle products, and limit exposure time. If hives are severe or accompanied by swelling, dizziness, or breathing issues, seek medical attention immediately—this could indicate a systemic reaction.
How long do shower-induced hives last?
Most resolve within 1–2 hours. Persistent hives beyond six weeks may indicate chronic urticaria, which requires professional evaluation and possibly prescription treatment like H2 blockers or omalizumab.
Checklist: Post-Shower Hive Prevention
- ✅ Use fragrance-free, hypoallergenic cleansers
- ✅ Set water temperature to lukewarm (below 100°F / 38°C)
- ✅ Install a shower filter if you have hard or chlorinated water
- ✅ Limit shower time to 5–10 minutes
- ✅ Dry skin gently—no vigorous rubbing
- ✅ Wear loose, breathable clothing post-shower
- ✅ Take daily non-sedating antihistamine if recommended by a doctor
- ✅ Keep a symptom journal for at least four weeks
Conclusion: Take Control of Your Skin Health
Hives after showering aren’t something you have to accept as normal. Whether driven by heat, chemicals, or a rare sensitivity to water, solutions exist. Small changes in routine—like lowering the thermostat on your water heater or switching to gentler products—can bring dramatic relief. More importantly, understanding your body’s signals empowers you to act early and prevent recurrence.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?