Hormonal balance plays a pivotal role in a woman’s overall health, influencing everything from menstrual regularity and fertility to mood, energy, and long-term wellness. Yet, many women experience symptoms like fatigue, weight gain, irregular periods, or mood swings without knowing the underlying cause. Accurately checking female hormone levels is the first step toward identifying imbalances and taking informed action. This guide walks through the most reliable testing methods, when to test, how to interpret results, and what to do next—based on clinical standards and expert insights.
Why Hormone Testing Matters
Hormones such as estrogen, progesterone, testosterone, thyroid hormones, and cortisol regulate critical bodily functions. Imbalances can stem from stress, aging, polycystic ovary syndrome (PCOS), perimenopause, or thyroid disorders. Symptoms often overlap, making self-diagnosis unreliable. Blood, saliva, and urine tests offer measurable data that can clarify whether hormonal issues are at play.
According to Dr. Felice Gersh, OB-GYN and integrative medicine specialist:
“Hormones don’t operate in isolation. A complete picture requires not just testing but understanding how these systems interact—especially between the ovaries, adrenal glands, and thyroid.” — Dr. Felice Gersh, Author of *Hormone Harmony*
Key Hormones to Test and Their Roles
Understanding which hormones to evaluate depends on your symptoms and life stage. The following table summarizes the primary female hormones, their functions, and common imbalance symptoms:
| Hormone | Primary Function | Common Imbalance Symptoms |
|---|---|---|
| Estrogen | Regulates menstrual cycle, supports bone and cardiovascular health | Heavy periods, bloating, breast tenderness, mood swings |
| Progesterone | Prepares uterus for pregnancy, balances estrogen | Irregular cycles, PMS, insomnia, anxiety |
| Testosterone (androgens) | Supports libido, muscle mass, energy | Low sex drive, fatigue, acne, hair loss |
| Thyroid Hormones (TSH, T3, T4) | Regulate metabolism, energy, temperature | Weight changes, cold intolerance, hair thinning, depression |
| Cortisol | Stress response, blood sugar regulation, immune function | Chronic fatigue, sleep disturbances, weight gain (abdominal) |
How to Test Hormone Levels: Methods Compared
There are three main ways to test hormone levels—each with advantages and limitations.
- Blood (serum) testing: Most commonly used in conventional medicine. Provides accurate measurements of total hormone levels, especially for thyroid and reproductive hormones. Best for detecting deficiencies or excesses.
- Saliva testing: Measures free (active) hormone levels. Useful for tracking cortisol rhythm throughout the day or assessing sex hormones in saliva. Often used in functional medicine.
- Dried urine testing (DUTCH test): Offers a comprehensive view by measuring both parent hormones and their metabolites. Can reveal how hormones are being processed, which is valuable for understanding estrogen metabolism and detoxification pathways.
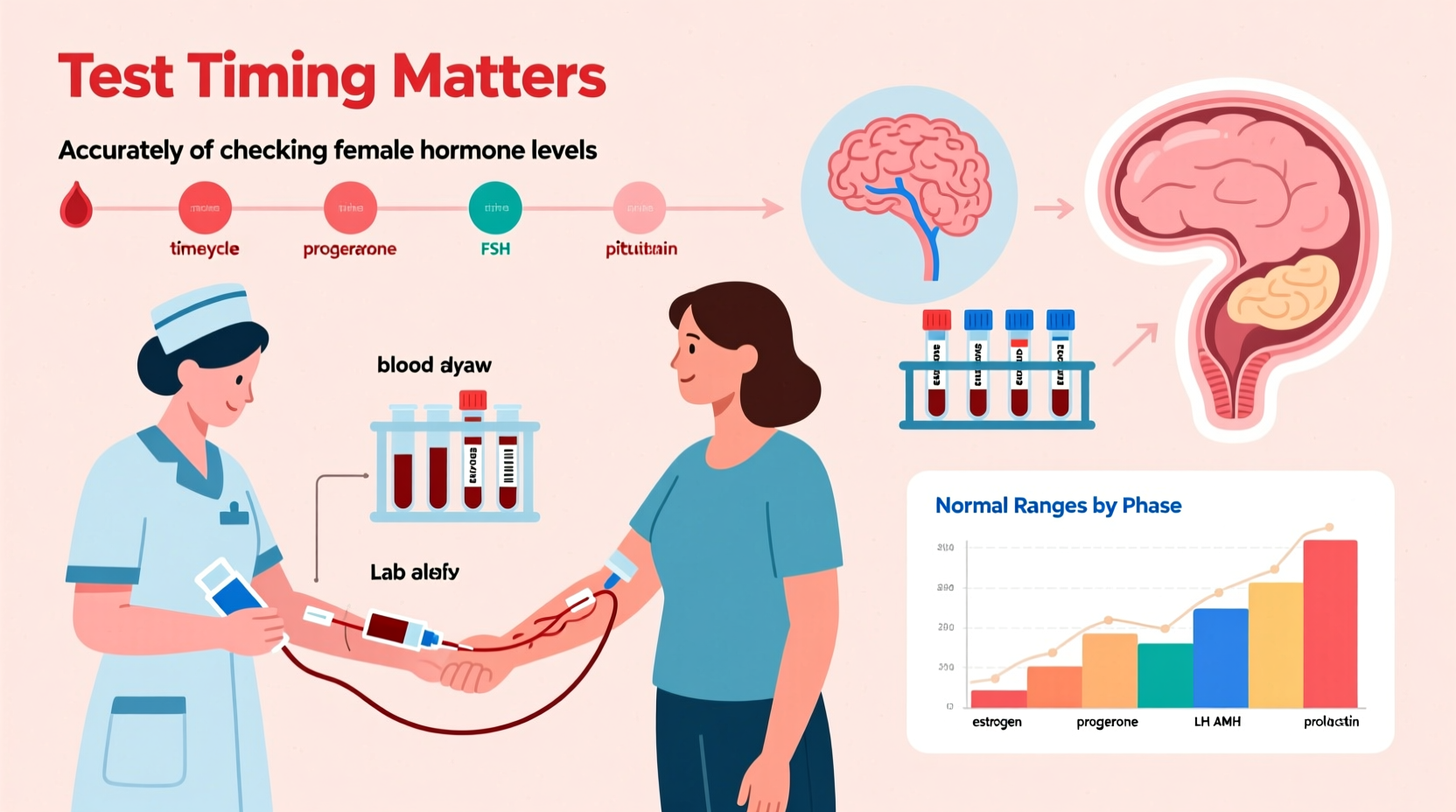
When and How to Test: A Step-by-Step Guide
Timing and preparation are crucial for accurate results. Follow this timeline based on your menstrual cycle and symptoms:
- Determine your cycle phase: For menstruating women, day 3 and day 21 of the cycle are standard testing windows. Day 3 assesses baseline FSH, LH, and estradiol; day 21 checks progesterone to confirm ovulation.
- Avoid testing during illness or high stress: Acute conditions can skew cortisol and thyroid markers.
- Fasting requirements: Some panels (e.g., insulin, glucose, lipid profile) require 8–12 hours of fasting. Confirm with your provider.
- Track symptoms: Keep a journal of symptoms, sleep patterns, and cycle dates to correlate with lab results.
- Collect samples properly: For at-home kits (saliva or urine), follow instructions precisely—contamination or incorrect timing can invalidate results.
- Review with a qualified practitioner: Interpretation should consider symptoms, medical history, and reference ranges (which vary by lab).
Real Example: Identifying Hidden PCOS
Sarah, age 29, had irregular periods, acne, and difficulty losing weight. Her doctor initially dismissed concerns, citing “normal” estrogen and progesterone on a day-3 blood test. However, she pursued further testing through a functional medicine clinic. A comprehensive panel revealed elevated free testosterone, high insulin, and low SHBG—classic markers of PCOS. With targeted lifestyle changes and medication, Sarah restored regular cycles within six months. Her case underscores the importance of full-panel testing and not relying on isolated markers.
Interpreting Your Results: Beyond the Reference Range
Laboratory reference ranges are population-based, but optimal levels for symptom relief may differ. For example, a progesterone level of 5 ng/mL on day 21 might fall within the \"normal\" range but is insufficient to counteract estrogen dominance, potentially causing heavy bleeding or irritability.
Consider these key interpretation principles:
- Look at ratios: The estrogen-to-progesterone ratio is more telling than either hormone alone. A high ratio suggests estrogen dominance.
- Evaluate patterns: Cortisol should peak in the morning and decline at night. Flattened curves indicate adrenal dysfunction.
- Check metabolic byproducts: DUTCH testing shows if estrogen is metabolized into protective (2-OH) or carcinogenic (16α-OH) compounds, guiding prevention strategies.
Common Testing Mistakes to Avoid
Even accurate labs can lead to misdiagnosis if protocols aren't followed. Avoid these pitfalls:
- Testing on the wrong cycle day
- Relying solely on TSH without checking free T3 and T4
- Ignoring symptoms because “everything is normal”
- Using at-home tests without professional guidance
- Not retesting after interventions to assess progress
Frequently Asked Questions
Can I test my hormones at home?
Yes, several FDA-approved at-home kits (like LetsGetChecked or Everlywell) allow you to collect saliva or dried blood spots. While convenient, they may not cover all necessary markers. Always consult a healthcare provider to interpret results and plan next steps.
What if my doctor says my hormones are normal but I still feel unwell?
This is common. Standard labs use broad reference ranges that may miss subtle imbalances. Seek a practitioner trained in functional or integrative medicine who considers optimal ranges and symptom correlation.
How often should I retest?
After starting treatment or lifestyle changes, retest in 3–6 months. Hormonal shifts take time, and monitoring ensures adjustments are effective.
Action Plan: What to Do After Testing
Once you have your results, take these steps:
- Consult a knowledgeable provider—endocrinologist, functional medicine doctor, or integrative gynecologist.
- Prioritize foundational health: balanced nutrition, quality sleep, stress management, and exercise.
- Address root causes: insulin resistance, gut health, environmental toxins, or chronic inflammation.
- Consider bioidentical hormone therapy only if indicated and monitored carefully.
- Track symptoms monthly to gauge progress.
Conclusion
Accurate hormone testing empowers women to understand their bodies and address issues at the root. Whether you're navigating perimenopause, struggling with fertility, or simply feeling off, the right tests at the right time can provide clarity and direction. Don’t settle for vague explanations or one-size-fits-all lab ranges. Take charge of your hormonal health with precise testing, informed interpretation, and proactive care.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?