Preparing for a colonoscopy or other lower gastrointestinal procedure requires more than just following prep instructions—it demands confidence that your colon is truly clean. An inadequately cleansed bowel can obscure polyps, delay diagnosis, or even require repeating the procedure. While many patients complete their prep regimens diligently, uncertainty often remains: Is my colon really clear? Understanding the physical cues, timing, and visual indicators of effective cleansing empowers you to proceed with assurance.
Understanding Colon Cleansing and Why It Matters
A successful colonoscopy hinges on visibility. The physician must examine the entire lining of the colon for abnormalities such as polyps or inflammation. If residual stool obstructs the view, small but significant findings may be missed. Studies show that up to 25% of colonoscopies are performed with suboptimal bowel preparation, increasing the risk of incomplete exams and repeat procedures.
Bowel prep works by flushing out contents through osmotic laxatives or large-volume solutions that stimulate frequent bowel movements. The goal isn't merely frequent trips to the bathroom—it's achieving a state where effluent is clear enough to allow unobstructed visualization during the exam.
“Bowel preparation is not optional—it’s foundational. A poorly prepped colon is like trying to inspect a muddy windshield; no matter how advanced the scope, clarity depends on cleanliness.” — Dr. Lena Patel, Gastroenterologist at Boston Digestive Institute
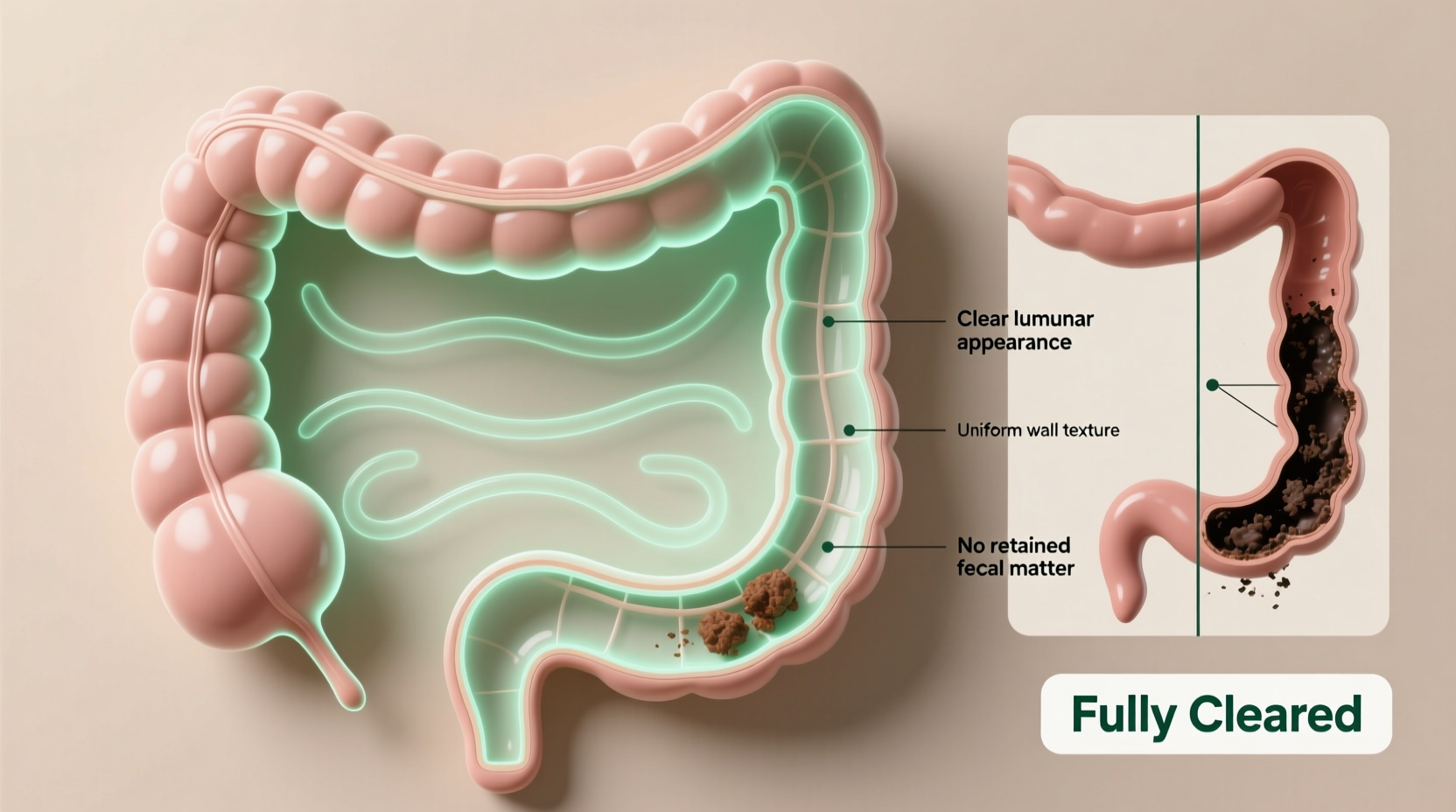
Key Visual and Physical Signs of a Fully Cleared Colon
Knowing what to look for in the toilet bowl is essential. Many patients mistake dark fluids or cloudy output as signs of completion, when in fact these may indicate lingering residue. Here’s how to interpret what you see:
- Clear or light yellow fluid: This is the gold standard. When your bowel movements resemble pale tea or lemonade, it indicates minimal particulate matter.
- No solid particles: Any visible chunks, flecks, or sediment suggest undigested food or residual stool.
- Translucent consistency: Fluid should not be cloudy, murky, or brownish. Even faint discoloration can signal incomplete clearance.
- Reduced frequency tapering off: As the colon empties, bowel movements decrease from constant to every hour or two—eventually stopping altogether.
It’s also important to note that green-colored liquid (especially after drinking PEG-based solutions) is normal and does not indicate incomplete prep. However, red or bloody discharge should be reported immediately to your healthcare provider.
Step-by-Step Guide to Confirming Bowel Clearance
Follow this timeline-based approach to assess your prep status accurately:
- Begin monitoring after the first few hours of starting prep. Initial bowel movements will likely be semi-solid or loose, which is expected.
- Track changes every 30–60 minutes. Note color, consistency, and presence of solids. Use a journal or mental checklist.
- Look for transition to liquid stools within 2–3 hours. This signals the colon is beginning to empty.
- Wait for clear, particle-free output. Most patients achieve this 4–6 hours after starting prep, though timing varies.
- Continue drinking solution until scheduled stop time—even if output appears clear earlier. Stopping early risks incomplete cleansing in the proximal (upper) colon.
- Resume only clear liquids until the procedure. No solid food, pulp-containing drinks, or red/purple liquids.
Do not rely solely on frequency. Some individuals continue having watery stools without full clearance due to poor motility or inadequate solution intake. Completing the full volume prescribed is critical—even if you feel “done.”
Do’s and Don’ts During Bowel Prep
| Do’s | Don’ts |
|---|---|
| Drink the full volume of prep solution as directed | Stop drinking the solution early because you feel clear |
| Consume only clear liquids (broth, apple juice, sports drinks) | Eat solid foods or consume dairy products |
| Sip slowly if nausea occurs; use anti-nausea meds if approved | Ignore persistent vomiting—contact your doctor if unable to keep liquids down |
| Use soft toilet paper or wipes to protect irritated skin | Sit on the toilet for extended periods; minimize straining |
| Stay near a bathroom and rest as needed | Engage in strenuous activity or drive while sedated from medications |
Real-World Example: Sarah’s Experience
Sarah, a 52-year-old teacher, followed her colonoscopy prep instructions closely but stopped drinking the second half of her PEG solution after six hours because her output “looked pretty clear.” During the procedure, her gastroenterologist found patches of retained stool in the ascending colon, obscuring two small polyps. Although they were eventually detected, the exam took longer and required additional maneuvers.
Afterward, her doctor explained that the right side of the colon often clears last and requires complete solution intake for optimal results. For her next screening, Sarah set hourly reminders to drink and used a flashlight to verify clarity. She completed the full prep and received a “perfect prep” rating—leading to a smooth, efficient procedure.
When to Contact Your Healthcare Provider
While mild discomfort, bloating, and fatigue are normal during prep, certain symptoms warrant medical attention:
- Inability to keep any liquids down for more than two hours
- Severe abdominal pain or distension
- Dizziness, lightheadedness, or rapid heartbeat (signs of dehydration)
- Fever over 100.4°F (38°C)
- Rectal bleeding (not minor streaking from irritation)
If you're unsure whether your prep is sufficient, contact your clinic the day before the procedure. Many offices offer photo assessment via secure messaging—sending a well-lit image of your final bowel movement can provide peace of mind.
Frequently Asked Questions
Can I stop drinking the prep solution once my stool is clear?
No. Even with clear output, you must finish the full prescribed volume unless instructed otherwise by your doctor. The upper colon may still contain residue not reflected in early-clearing segments.
What counts as a “clear liquid”?
Clear liquids include water, broth, plain gelatin (not red or purple), black coffee or tea (no cream), sports drinks (Gatorade, Powerade—avoid red/purple), and apple juice. Anything you can see through is generally acceptable.
I have diabetes. How do I manage my diet during prep?
Work with your care team ahead of time. You may need to adjust insulin or oral medications. Use sugar-free options when possible, and monitor blood glucose frequently. Some facilities provide specialized prep plans for diabetic patients.
Final Checklist Before Your Procedure
- ✔ Completed full volume of bowel prep solution
- ✔ Final bowel movement was clear, light-colored, and free of particles
- ✔ Consumed only approved clear liquids for at least 12 hours prior
- ✔ Nothing eaten or drunk (except sips of water with meds) for at least 4 hours before the procedure
- ✔ Arranged transportation—no driving post-procedure
- ✔ Contacted provider about any concerns or complications
Conclusion: Confidence Starts with Clarity
Knowing whether your colon is fully cleared isn’t guesswork—it’s a process grounded in observation, discipline, and informed decision-making. By recognizing the signs of effective cleansing, adhering to prep guidelines, and using tools like split dosing and visual verification, you take control of your diagnostic accuracy. A well-prepared colon isn’t just about convenience; it’s about ensuring your health screening delivers the most reliable results possible. Take pride in your preparation—your future self will thank you for the clarity you’ve achieved today.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?