Endometriosis affects an estimated 1 in 10 women of reproductive age, yet it takes an average of 7 to 10 years to receive a formal diagnosis. This delay often stems from misunderstood symptoms, lack of awareness, and limited access to specialized care. Endometriosis occurs when tissue similar to the lining of the uterus grows outside the uterine cavity—commonly on the ovaries, fallopian tubes, bowel, or bladder—leading to chronic pain, inflammation, and sometimes infertility. Recognizing the signs early and knowing how to pursue testing can significantly improve long-term outcomes.
Understanding the Symptoms of Endometriosis
Endometriosis presents with a wide range of symptoms, many of which overlap with other conditions like irritable bowel syndrome (IBS) or pelvic inflammatory disease (PID). Common indicators include:
- Severe menstrual cramps that interfere with daily activities
- Pain during or after sexual intercourse
- Chronic pelvic or lower back pain
- Painful bowel movements or urination during periods
- Heavy or irregular menstrual bleeding
- Fatigue, bloating, or nausea around menstruation
- Difficulty conceiving
Some individuals experience no symptoms at all and only discover they have endometriosis during fertility evaluations. Because symptoms vary widely, self-awareness and detailed communication with healthcare providers are critical first steps toward diagnosis.
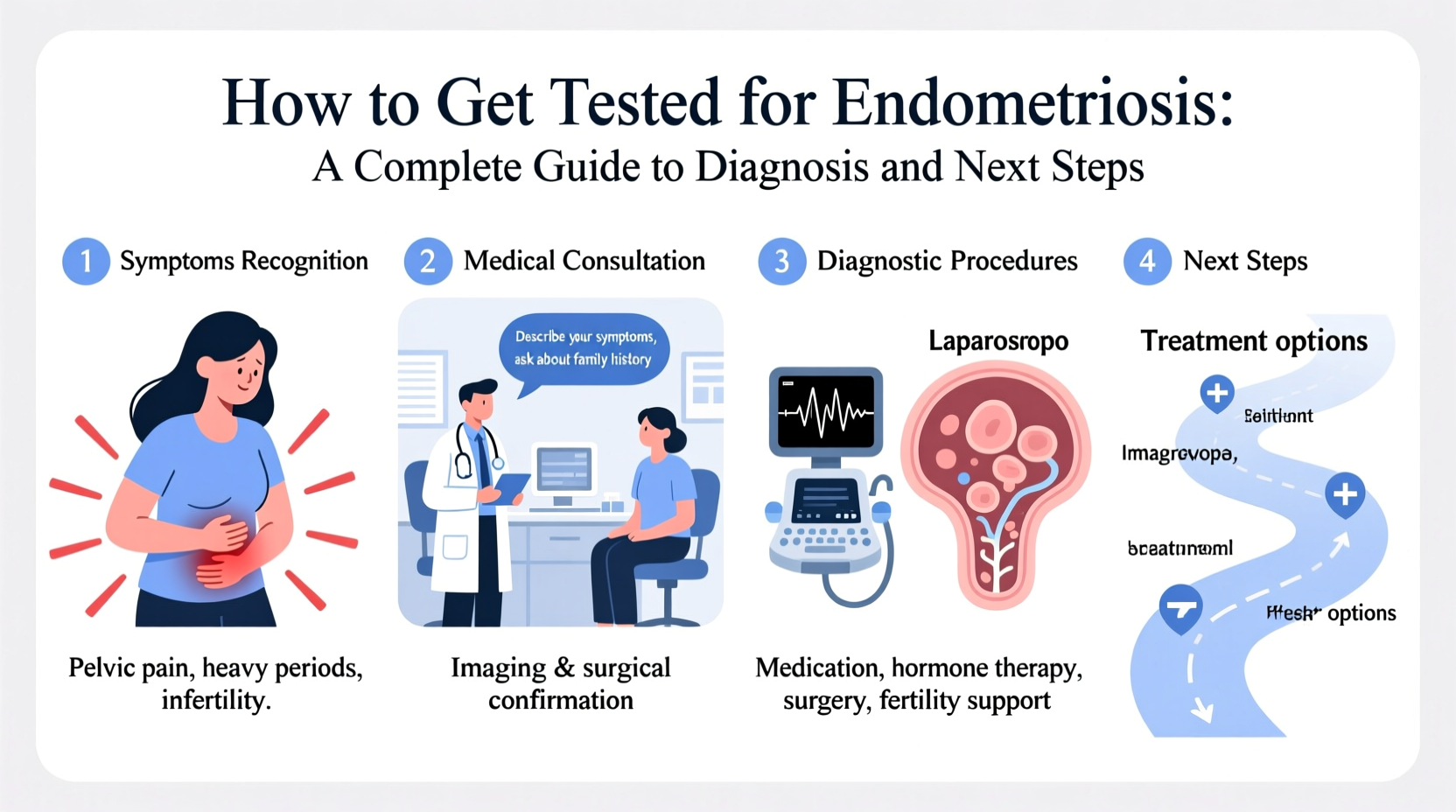
The Diagnostic Process: What to Expect
There is no single non-invasive test that definitively diagnoses endometriosis. Instead, diagnosis involves a combination of clinical evaluation, imaging, and sometimes surgery. The process typically follows this sequence:
- Medical history review: Your doctor will ask about your symptoms, family history (endometriosis can run in families), and reproductive health.
- Physical pelvic exam: A manual examination may reveal cysts, tenderness, or abnormal tissue, though mild cases often appear normal.
- Imaging tests: Transvaginal ultrasound or MRI can detect endometriomas (ovarian cysts caused by endometriosis) but cannot confirm superficial lesions.
- Laparoscopic surgery: The gold standard for diagnosis. A surgeon inserts a small camera through an abdominal incision to visualize and biopsy suspected endometrial implants.
It’s important to understand that a normal ultrasound does not rule out endometriosis. Many lesions are too small or shallow to be seen without direct visualization during laparoscopy.
“Many patients are told their pain is ‘normal’ or psychological. We now know that severe period pain is not typical and should always prompt further investigation.” — Dr. Sarah Thompson, Gynecological Surgeon and Endometriosis Specialist
Step-by-Step Guide to Getting Tested
If you suspect you have endometriosis, taking structured action improves your chances of timely diagnosis. Follow this timeline to navigate the healthcare system effectively:
- Week 1–2: Document your symptoms
Create a detailed log tracking pain levels, menstrual patterns, bowel and urinary changes, and impact on work or relationships. - Week 3: Schedule an appointment with your primary care provider or gynecologist
Bring your symptom journal. Be specific about how pain affects your life. Ask directly: “Could this be endometriosis?” - Week 4–6: Request appropriate imaging
Ask for a transvaginal ultrasound if available. If results are inconclusive but symptoms persist, request a referral to a gynecologist with expertise in pelvic pain or endometriosis. - Week 7–10: Consult a specialist
A skilled gynecologist may recommend further imaging (like an MRI) or discuss diagnostic laparoscopy based on your history. - Week 11+: Surgical evaluation (if needed)
If laparoscopy is advised, ensure the surgeon plans to excise (remove) suspicious tissue for biopsy, not just ablate (burn) it. Histological confirmation is essential for definitive diagnosis.
Do’s and Don’ts During the Diagnostic Journey
| Do’s | Don’ts |
|---|---|
| Keep a detailed symptom journal | Minimize your pain as “just bad periods” |
| Seek a second opinion if dismissed | Assume a normal ultrasound means nothing is wrong |
| Ask for referrals to endometriosis specialists | Delay care due to fear of surgery |
| Discuss fertility concerns early | Rely solely on painkillers without investigating causes |
| Prepare questions before appointments | Accept vague explanations without follow-up |
Real Example: Delayed Diagnosis and Advocacy
Maya, a 28-year-old teacher, experienced debilitating cramps since her teens. Doctors prescribed birth control and dismissed her discomfort as normal. Over ten years, she missed work monthly and struggled with painful intercourse. After researching online, she tracked her symptoms and found a specialist in her region who performed a laparoscopy. She was diagnosed with Stage III endometriosis involving her ovaries and bowel. Following excision surgery and hormonal therapy, her pain decreased dramatically. Maya now advocates for better education and earlier intervention. Her story underscores the importance of persistence and informed self-advocacy.
What Happens After Diagnosis?
Receiving a diagnosis is both validating and overwhelming. Next steps depend on your goals—whether managing pain, preserving fertility, or preventing progression.
Treatment options include:
- Hormonal therapies: Birth control pills, progestins, or GnRH agonists to suppress ovulation and reduce lesion activity.
- Pain management: NSAIDs, physical therapy, or nerve-targeting medications.
- Surgery: Laparoscopic excision to remove endometrial implants; preferred for deep infiltrating endometriosis.
- Fertility support: IVF or surgical restoration of anatomy if conception is difficult.
Work with a multidisciplinary team—gynecologists, pain specialists, fertility experts, and mental health providers—to build a personalized plan. Early, comprehensive care reduces complications and improves quality of life.
FAQ
Can endometriosis be diagnosed without surgery?
No definitive diagnosis can be made without visual confirmation and biopsy via laparoscopy. While imaging and symptoms may strongly suggest endometriosis, only surgery provides conclusive proof.
Is endometriosis the same as PCOS?
No. Polycystic Ovary Syndrome (PCOS) is a hormonal disorder affecting ovulation, while endometriosis involves misplaced endometrial-like tissue causing inflammation and scarring. They can coexist but are distinct conditions.
Does hysterectomy cure endometriosis?
Not necessarily. Since endometriosis lesions exist outside the uterus, removing the uterus alone does not eliminate the disease. Excision of all affected tissue is required for optimal outcomes.
Checklist: Preparing for Your Doctor’s Visit
- ✅ Record symptoms: date, duration, severity, triggers
- ✅ List all medications and supplements you’re taking
- ✅ Write down key personal details: family history, sexual health, fertility goals
- ✅ Prepare questions: “Could this be endometriosis?” “What tests do I need?” “Can I see a specialist?”
- ✅ Bring a trusted friend or partner for support, if possible
Conclusion: Take Control of Your Health
Getting tested for endometriosis requires courage, persistence, and proactive engagement with the healthcare system. You are not alone, and your pain is not normal. With accurate diagnosis and expert care, effective treatment is within reach. Whether you're seeking pain relief, trying to conceive, or simply want answers, start today by documenting your symptoms and speaking up. Share this guide with someone who might need it. Together, we can reduce the diagnostic delay and ensure more people receive the care they deserve.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?