Bronchitis is a common respiratory condition affecting millions each year. It occurs when the bronchial tubes—responsible for carrying air to and from the lungs—become inflamed, often due to infection or irritation. While many cases are mild and resolve on their own, recognizing the early signs and knowing when to seek medical help can prevent complications and speed up recovery. Understanding the difference between acute and chronic bronchitis, identifying hallmark symptoms, and being aware of red flags are essential steps in managing your respiratory health effectively.
Understanding Bronchitis: Acute vs. Chronic
Bronchitis comes in two primary forms: acute and chronic. Each has distinct causes, durations, and implications for long-term health.
Acute bronchitis typically develops after a viral upper respiratory infection, such as a cold or flu. It usually lasts 1–3 weeks and resolves without lasting damage. Most people recover fully with rest and supportive care.
Chronic bronchitis is a more serious, long-term condition defined by a persistent cough with mucus most days for at least three months, occurring over two consecutive years. It is a type of chronic obstructive pulmonary disease (COPD) and is often linked to smoking or long-term exposure to lung irritants like dust, fumes, or pollution.
“Bronchitis isn’t just a ‘bad cold’—it’s inflammation of the airways that can escalate if ignored, especially in vulnerable populations.” — Dr. Lena Patel, Pulmonologist
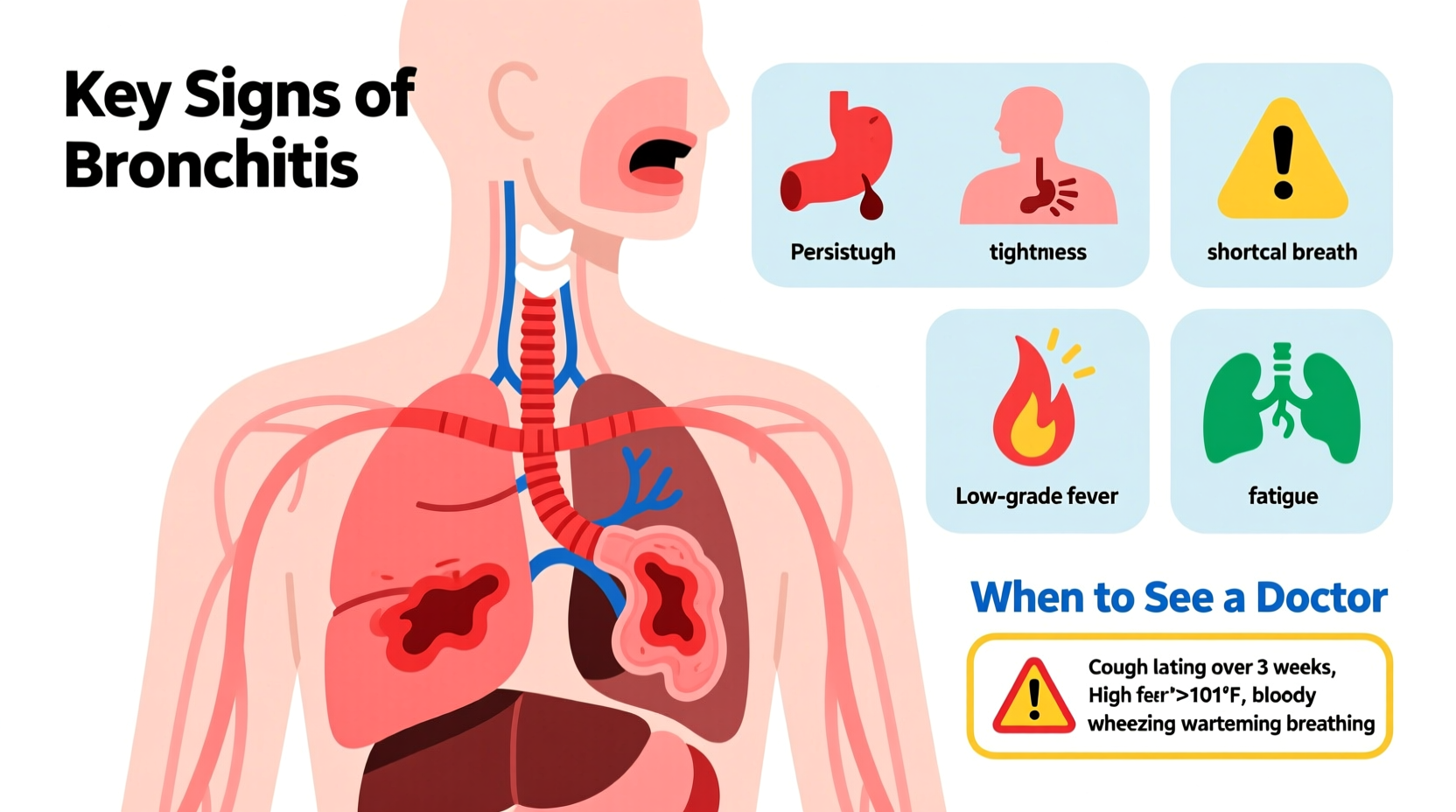
Key Signs and Symptoms of Bronchitis
Symptoms of bronchitis often mimic those of a cold or flu but tend to linger longer, particularly the cough. Recognizing these signs early helps in managing discomfort and preventing progression.
- Persistent cough (dry or productive)
- Coughing up clear, white, yellowish, or green mucus
- Chest discomfort or tightness
- Shortness of breath, especially during activity
- Fatigue
- Mild fever or chills (more common in acute cases)
- Wheezing or a whistling sound when breathing
The hallmark symptom is a cough that persists beyond the typical 7–10 days of a cold. In acute bronchitis, this cough may last several weeks even after other symptoms fade, as the airways remain irritated. In chronic bronchitis, the cough is recurrent and often worse in the mornings.
When Symptoms Warrant Immediate Attention
While bronchitis is often self-limiting, certain symptoms indicate a need for prompt medical evaluation. These may suggest pneumonia, worsening COPD, or another serious condition.
| Symptom | May Indicate | Action |
|---|---|---|
| Fever above 100.4°F (38°C) lasting more than 3 days | Bacterial infection or pneumonia | See a doctor promptly |
| Cough lasting over 3 weeks | Chronic bronchitis or asthma | Medical evaluation recommended |
| Shortness of breath at rest or worsening over time | Lung function decline | Seek urgent care |
| Coughing up blood | Severe irritation or underlying condition | Immediate medical attention |
| Bluish lips or fingertips | Low oxygen levels | Emergency care required |
Common Causes and Risk Factors
Identifying what triggers bronchitis helps in prevention and management. The most frequent causes include:
- Viral infections: Over 90% of acute bronchitis cases stem from viruses like influenza, rhinovirus, or RSV.
- Bacterial infections: Less common, but possible, especially in individuals with weakened immune systems.
- Tobacco smoke: The leading cause of chronic bronchitis. Even secondhand smoke increases risk.
- Air pollution and occupational hazards: Long-term exposure to dust, chemical fumes, or exhaust fumes can inflame the bronchial tubes.
- Weakened immunity: Conditions like diabetes, HIV, or chemotherapy increase susceptibility.
People over 50, smokers, young children, and those with pre-existing lung or heart conditions are at higher risk. Frequent respiratory infections also raise the likelihood of developing chronic bronchitis over time.
Step-by-Step Guide to Managing Mild Bronchitis at Home
If diagnosed with mild acute bronchitis, most recovery happens through supportive care. Follow this timeline to ease symptoms and promote healing.
- Days 1–3: Rest and Hydration
Stay home, drink plenty of fluids (water, herbal teas), and get adequate sleep. This supports your immune system and thins mucus. - Days 4–7: Symptom Management
Use over-the-counter remedies like acetaminophen for fever, honey for cough (adults and children over 1), and saline nasal sprays. Avoid decongestants if you have high blood pressure. - Days 8–14: Monitor Progress
Track cough frequency and mucus color. A lingering cough is normal, but worsening symptoms require medical review. - After 14 Days: Reassess
If cough persists beyond three weeks, consult a healthcare provider to rule out pneumonia, asthma, or GERD-related cough.
Note: Antibiotics are not effective for viral bronchitis and should only be used if a bacterial infection is confirmed.
Real-Life Example: When a Cough Was More Than Just a Cold
James, a 42-year-old office worker and former smoker, developed a nagging cough after a mild cold. He assumed it would pass, but after two weeks, he felt increasingly fatigued and noticed shortness of breath climbing stairs. His mucus turned green, and he developed a low-grade fever. Concerned, he visited his primary care physician, who listened to his lungs and ordered a chest X-ray. The results revealed early signs of pneumonia, likely stemming from untreated acute bronchitis. With a course of antibiotics and rest, James recovered fully—but the experience taught him to take persistent respiratory symptoms seriously.
This case highlights how easily bronchitis can be dismissed as “just a cough,” yet progress into something more serious without proper monitoring.
Do’s and Don’ts for Bronchitis Recovery
| Do’s | Don’ts |
|---|---|
| Drink plenty of fluids to loosen mucus | Smoke or expose yourself to secondhand smoke |
| Use a humidifier to soothe airways | Take antibiotics unless prescribed |
| Rest and avoid strenuous activity | Suppress a productive cough completely—coughing clears mucus |
| Wash hands frequently to prevent spreading germs | Return to work or school while still contagious or fatigued |
| Consult a doctor if symptoms worsen | Ignore difficulty breathing or chest pain |
FAQ: Common Questions About Bronchitis
Can bronchitis turn into pneumonia?
Yes, in some cases. While bronchitis and pneumonia are different conditions, untreated or severe bronchitis can lead to pneumonia, especially in older adults or those with compromised immune systems. Persistent fever, worsening cough, and sharp chest pain are warning signs.
Is bronchitis contagious?
Acute bronchitis caused by a virus is contagious, primarily through respiratory droplets from coughing or sneezing. Chronic bronchitis itself is not contagious, though underlying infections may be.
How can I prevent bronchitis?
Get an annual flu vaccine, practice good hand hygiene, avoid smoking, wear a mask in polluted environments, and manage allergies. For those with COPD, follow your treatment plan diligently.
Checklist: When to See a Doctor for Bronchitis
- ☐ Cough lasts more than 3 weeks
- ☐ Fever above 100.4°F persists beyond 3 days
- ☐ Shortness of breath at rest or with minimal activity
- ☐ Chest pain or pressure
- ☐ Coughing up blood or rust-colored mucus
- ☐ Lips or nails turning blue
- ☐ History of asthma, COPD, or heart disease
- ☐ Symptoms improve then suddenly worsen
Conclusion: Take Your Respiratory Health Seriously
Bronchitis is more than just a lingering cough—it’s a signal from your body that your airways are under stress. By learning to recognize its key signs and understanding when symptoms cross the line from manageable to dangerous, you empower yourself to make informed health decisions. Whether it’s adjusting your routine at home or seeking timely medical advice, proactive care can prevent complications and support faster recovery. Don’t downplay persistent respiratory symptoms. Your lungs are vital—listen to them, act early, and prioritize long-term wellness.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?