Allergies affect over 50 million Americans annually, making them one of the most common chronic conditions in the United States. Whether you're struggling with seasonal sniffles, unexplained rashes, or digestive discomfort after eating certain foods, allergy testing can provide clarity and a path toward relief. Yet many people hesitate due to uncertainty about the process, risks, or how to interpret results. Understanding what lies ahead—and how to prepare—can transform anxiety into empowerment.
Why Allergy Testing Matters
Accurate diagnosis is the foundation of effective treatment. Without proper testing, individuals often misattribute symptoms to other causes, leading to ineffective treatments or prolonged discomfort. Allergy tests identify specific allergens triggering immune responses, such as pollen, pet dander, mold, dust mites, or food proteins like peanuts or shellfish.
Knowing your triggers allows for targeted avoidance strategies, personalized medication plans, and, in some cases, immunotherapy. For children, early identification can prevent severe reactions and support healthier development. For adults, it can improve sleep, concentration, and overall quality of life.
“Many patients come in thinking they’re allergic to something when the real culprit is different. Testing removes guesswork and guides precise care.” — Dr. Lena Patel, Board-Certified Allergist & Immunologist
Types of Allergy Tests: What’s Available?
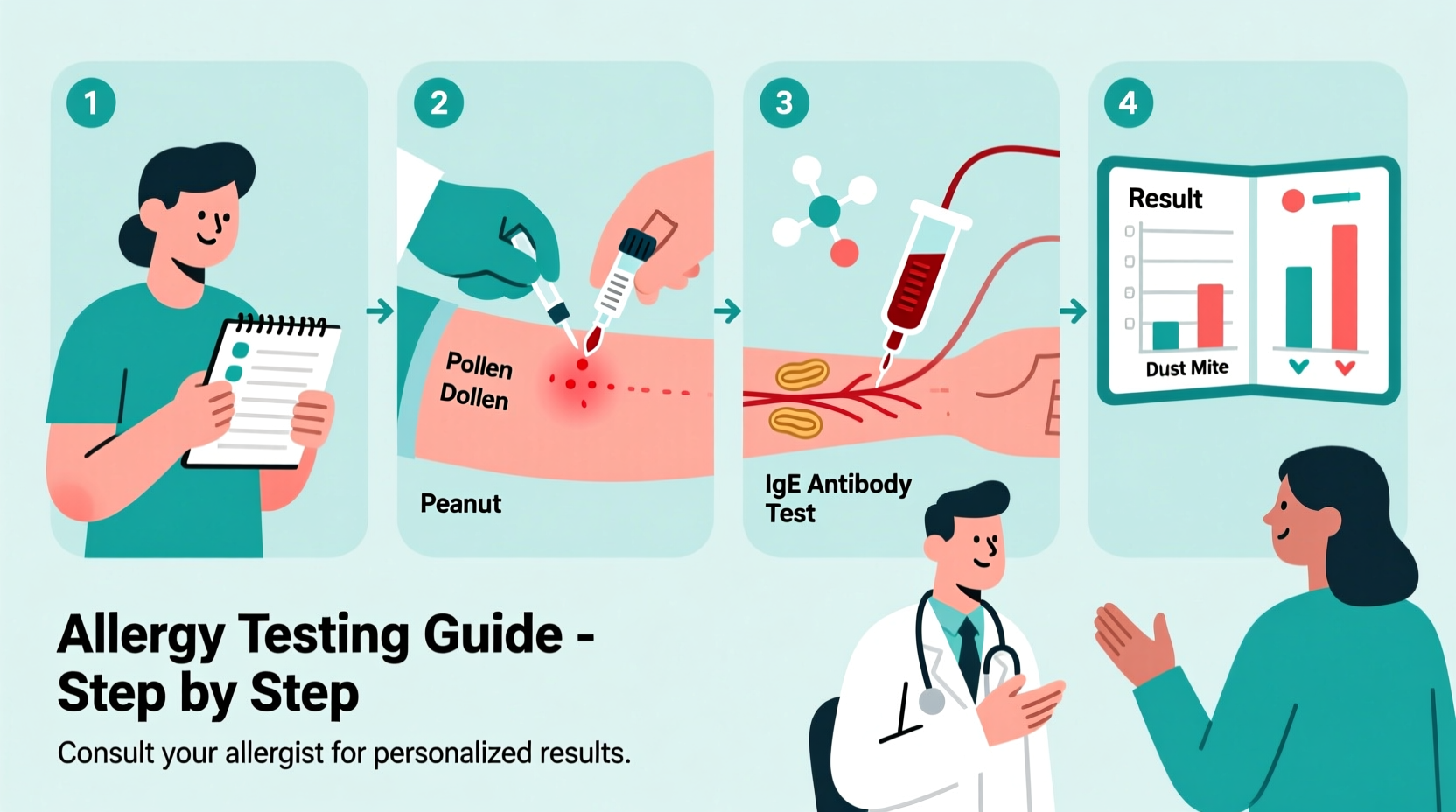
Not all allergy tests are the same. The type recommended depends on your symptoms, medical history, and suspected allergens. Here's a breakdown of the most common methods:
| Test Type | How It Works | Best For | Time to Results |
|---|---|---|---|
| Skin Prick Test | Small amounts of allergens applied to skin via tiny pricks | Seasonal allergies, food, pet dander, dust mites | 15–20 minutes |
| Intradermal Test | Allergen injected just under the skin | When skin prick is inconclusive (e.g., penicillin allergy) | 15–20 minutes |
| Blood Test (IgE) | Measures allergen-specific antibodies in blood sample | Patients who can’t stop antihistamines or have skin conditions | Several days |
| Oral Food Challenge | Controlled ingestion of suspected food under supervision | Confirming or ruling out food allergies | Hours (done in clinic) |
| Elimination Diet | Removing and reintroducing foods at home | Non-IgE food sensitivities (e.g., intolerances) | 2–6 weeks |
The skin prick test remains the most widely used method due to its speed, accuracy, and cost-effectiveness. Blood tests are valuable when skin testing isn't feasible, but they tend to be more expensive and slower.
Step-by-Step Guide to Preparing for Allergy Testing
Preparation plays a crucial role in ensuring accurate results. Follow this timeline to get ready effectively:
- Consult Your Doctor (1–2 Weeks Before)
Discuss your symptoms, family history, and any medications you’re taking. Your primary care provider may refer you to an allergist for specialized testing. - Review Medications With Your Allergist
Antihistamines (like Benadryl, Zyrtec, Claritin) can suppress skin test reactions. You’ll typically need to stop them 3–7 days before testing. Never discontinue prescription meds without approval from your doctor. - Keep a Symptom Journal
Note when and where symptoms occur, what you were exposed to, and their severity. This helps your allergist narrow down possible triggers. - Avoid Known Triggers (If Possible)
While you don’t want to artificially alter your environment, minimizing exposure shortly before testing won’t impact diagnostic accuracy and may reduce baseline symptoms. - Dress Comfortably for the Appointment
Wear loose clothing that exposes your forearms and upper back—common test sites. Avoid wearing perfume or heavy scents, which could irritate sensitive skin. - Bring a List of Questions
Clarify concerns about pain, safety, follow-up steps, and costs. Being informed reduces anxiety and improves outcomes.
What to Expect During the Test
Most allergy tests are quick and minimally invasive. A typical skin prick test takes less than 30 minutes. Here’s how it unfolds:
- You’ll sit comfortably while the allergist marks small areas on your forearm or back.
- A drop of each allergen solution is placed on the skin, then a lancet gently pricks the surface—no needles involved.
- After 15–20 minutes, the doctor measures any raised, red bumps (wheals). Larger wheals usually indicate stronger sensitivity.
- Results are discussed immediately, often with a printed report detailing reactive allergens.
Blood tests require a simple venipuncture. While results take longer, they’re especially useful for those with eczema, dermatographism, or who cannot pause antihistamine use.
“I was terrified of needles, so I assumed allergy testing would be awful. But the skin prick felt like a mild mosquito bite—barely noticeable. Getting answers was worth every second.” — Maria T., patient from Portland, OR
Interpreting Results: Beyond the Positive or Negative
A positive test doesn’t always mean you have a clinical allergy. Some people show sensitization (immune response) without experiencing symptoms. Conversely, false negatives can occur, especially with delayed-type reactions.
Your allergist will correlate test findings with your symptom history. For example, if you test positive for birch pollen but live in a desert climate and only sneeze indoors, the real issue might be dust mites, not pollen.
Common Mistakes to Avoid
- Stopping asthma or heart medications without guidance – Some beta-blockers can interfere with emergency treatment during rare severe reactions.
- Testing too soon after an allergic reaction – Wait until symptoms stabilize unless urgent.
- Assuming food additives are the cause – Artificial colors or preservatives rarely cause true IgE-mediated allergies.
- Skipping follow-up appointments – Management plans evolve; retesting may be needed every few years.
Frequently Asked Questions
Is allergy testing safe?
Yes. Serious reactions are extremely rare, especially with skin prick tests. Clinics are equipped with epinephrine and emergency protocols. Oral challenges are conducted under strict supervision.
Can children be tested?
Absolutely. Testing can be performed at any age, even in infants. Skin testing is generally safe for babies over 6 months. Early detection helps manage eczema, food allergies, and respiratory issues.
How long do results last?
Allergies can change over time. Children often outgrow milk or egg allergies, while adults may develop new sensitivities. Re-evaluation every 2–3 years—or after major symptom changes—is advisable.
Action Plan: Next Steps After Testing
Once you have results, work with your allergist to build a personalized management strategy. This checklist ensures you stay proactive:
- ✅ Identify top 3–5 triggers to prioritize avoidance
- ✅ Install HEPA filters if allergic to airborne particles
- ✅ Read food labels carefully if diagnosed with food allergy
- ✅ Carry prescribed epinephrine auto-injector if at risk for anaphylaxis
- ✅ Schedule follow-up visits to monitor progress or adjust therapy
- ✅ Consider immunotherapy (allergy shots or tablets) for long-term desensitization
Conclusion
Understanding and preparing for allergy testing removes fear and unlocks better health. From knowing which medications to pause to interpreting complex results, being informed leads to smarter decisions. Millions live with undiagnosed allergies, enduring symptoms they assume are “just part of life.” But relief is possible—with the right test, the right timing, and the right guidance.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?