The human appendix is a small, finger-shaped pouch attached to the large intestine. While its exact function remains unclear, one thing is certain: when it becomes inflamed—a condition known as appendicitis—it can quickly escalate into a life-threatening situation if not addressed promptly. A ruptured appendix can lead to widespread infection in the abdominal cavity, known as peritonitis, which requires emergency medical intervention. Recognizing the early signs of an impending rupture and knowing how to respond could mean the difference between a swift recovery and severe complications.
Understanding Appendicitis and the Risk of Rupture
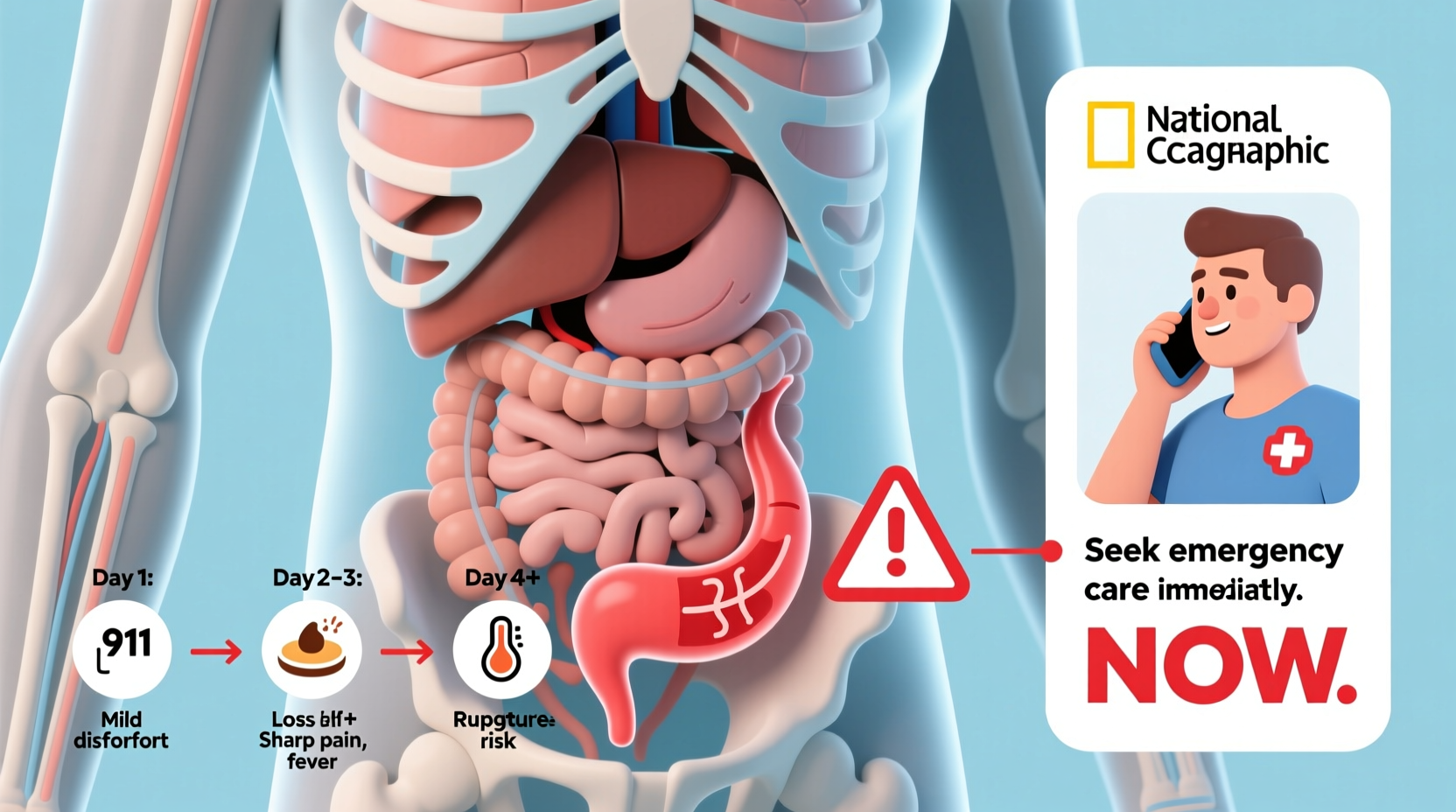
Appendicitis occurs when the appendix becomes blocked—often by stool, a foreign body, or infection—leading to inflammation and swelling. As pressure builds inside the organ, blood flow is restricted, increasing the risk of tissue death and rupture. The average time from symptom onset to rupture ranges from 36 to 72 hours, though this can vary significantly depending on age, overall health, and individual anatomy.
Children and older adults are at higher risk for delayed diagnosis because symptoms may be less typical or easily mistaken for other conditions. According to the American College of Surgeons, approximately 250,000 cases of appendicitis are reported annually in the U.S., with about 30% involving perforation at the time of surgery.
“Time is critical in suspected appendicitis. Every hour that passes without treatment increases the risk of rupture and postoperative complications.” — Dr. Rebecca Nguyen, Emergency Medicine Specialist, Johns Hopkins Hospital
Key Early Warning Signs of Impending Appendix Rupture
Recognizing the progression of symptoms is crucial. While initial discomfort may seem mild, certain changes signal worsening inflammation and potential rupture:
- Shifting pain: Pain often begins near the navel and gradually moves to the lower right abdomen. This migration is a hallmark of appendicitis.
- Increasing intensity: Dull ache turning into sharp, constant pain that worsens with movement, coughing, or sneezing.
- Fever that escalates: A low-grade fever (around 99–100.5°F) may spike above 101°F as the infection spreads.
- Nausea and vomiting: Often follows the onset of pain, sometimes accompanied by loss of appetite or bloating.
- Abdominal rigidity: The abdomen becomes tender to touch, especially in the lower right quadrant, and may feel hard or swollen.
- Sudden relief of pain: Paradoxically, a brief decrease in pain may indicate rupture—the appendix has burst, releasing pressure—but this is followed by rapid deterioration.
What Happens When the Appendix Bursts?
A burst appendix allows bacteria and infected material to spill into the abdominal cavity, triggering peritonitis—an inflammation of the lining of the abdominal wall. This condition causes systemic infection (sepsis), organ dysfunction, and can be fatal without urgent care.
After rupture, symptoms typically intensify rapidly:
- Severe, diffuse abdominal pain across the entire belly
- High fever with chills
- Rapid heart rate and shallow breathing
- Dizziness or lightheadedness due to infection and fluid loss
- Inability to pass gas or have a bowel movement
In some cases, the body may form an abscess around the rupture, temporarily containing the infection. While this might delay full-blown peritonitis, it still requires drainage and antibiotics before surgical removal of the appendix can occur.
Step-by-Step: What to Do If You Suspect Appendicitis
If you or someone else shows signs of possible appendicitis, follow this timeline of actions to minimize the risk of rupture:
- Monitor symptoms closely (within first 6–12 hours): Note the location, duration, and progression of pain. Track fever and any gastrointestinal symptoms.
- Avoid painkillers and laxatives: These can mask symptoms or increase intestinal movement, raising rupture risk.
- Do not eat or drink: In case surgery is needed, an empty stomach reduces anesthesia risks.
- Seek immediate medical evaluation (within 24 hours of symptom onset): Visit an urgent care clinic or emergency room. Diagnostic tools like ultrasound or CT scans can confirm appendicitis.
- Follow medical advice: If diagnosed early, most patients undergo laparoscopic appendectomy within hours. Delayed cases may require more complex procedures.
Common Misconceptions That Delay Treatment
Misunderstanding appendicitis symptoms contributes to dangerous delays. Below is a comparison of myths versus facts:
| Myth | Fact |
|---|---|
| “Appendicitis always starts with severe pain.” | Pain often begins mildly and progresses over hours. |
| “Only young people get appendicitis.” | It can occur at any age, though most common between 10–30. |
| “If I’m not vomiting, it’s not serious.” | Not all patients vomit; localized pain and fever are key indicators. |
| “I should wait to see if it gets better.” | Waiting increases rupture risk. Early evaluation saves lives. |
Real-Life Scenario: A Close Call with Rupture
At 16, Mark began feeling mildly nauseous after dinner, followed by vague stomach discomfort. He assumed it was food poisoning and rested at home. By midnight, the pain had shifted to his lower right side and intensified. His mother noticed he was running a fever and reluctant to move. They arrived at the ER at 2 a.m.—just 30 hours after symptom onset. A CT scan confirmed acute appendicitis with early signs of perforation. Surgeons performed an emergency appendectomy and drained a small abscess. Mark spent five days in the hospital recovering. His doctor later said that waiting another 12 hours could have led to full sepsis.
This case underscores how quickly appendicitis can progress—and how parental awareness and timely action prevented a worse outcome.
Checklist: When to Seek Immediate Medical Help
Use this checklist if abdominal pain persists beyond a few hours:
- ✔ Pain localized to lower right abdomen
- ✔ Fever rising above 100.4°F
- ✔ Nausea or vomiting after pain begins
- ✔ Increased pain with movement or coughing
- ✔ Loss of appetite or inability to pass gas
- ✔ Abdominal swelling or rigidity
- ✔ Rapid heartbeat or dizziness
If three or more apply, go to the emergency room immediately.
Frequently Asked Questions
Can appendicitis resolve on its own?
While rare cases of mild appendicitis may improve temporarily, the risk of recurrence and future rupture remains high. Most medical experts recommend surgical removal once diagnosed.
Is there a test for appendicitis?
There is no single definitive test. Doctors use a combination of physical exams, blood tests (to check for elevated white blood cells), and imaging such as ultrasound or CT scans to make a diagnosis.
What happens if my appendix bursts?
A rupture leads to peritonitis, requiring emergency surgery, intravenous antibiotics, and potentially longer hospitalization. Recovery time increases significantly compared to uncomplicated appendectomy.
Final Thoughts: Act Fast, Stay Safe
Appendicitis doesn’t announce itself with fanfare. It creeps in with subtle signals that can be mistaken for indigestion or a virus. But beneath the surface, a ticking clock is running. The window between treatable inflammation and dangerous rupture is narrow—often less than two days. Knowing the signs, resisting the urge to “wait and see,” and seeking prompt medical attention are the most effective ways to protect yourself and your loved ones.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?