Fibromyalgia affects millions worldwide, yet it remains one of the most misunderstood chronic conditions. Characterized by widespread pain, fatigue, and cognitive disturbances, fibromyalgia often goes undiagnosed for years due to its overlapping symptoms with other disorders. Recognizing the early warning signs is critical—not just for symptom management, but for regaining control over daily life. Understanding what to look for, when to act, and how to navigate the medical system can make all the difference in long-term well-being.
Understanding Fibromyalgia: A Hidden Chronic Condition
Fibromyalgia is a neurological disorder that amplifies pain signals in the brain and spinal cord. Unlike arthritis, it does not cause inflammation or damage to joints, muscles, or tissues. Instead, it alters the way the central nervous system processes pain, resulting in heightened sensitivity. The exact cause remains unknown, though researchers believe a combination of genetic predisposition, physical trauma, infections, and psychological stress may trigger onset.
Because there are no definitive lab tests or imaging scans to confirm fibromyalgia, diagnosis relies heavily on clinical evaluation and symptom history. This often leads to delays—some patients report waiting up to five years before receiving an accurate diagnosis. Early recognition of hallmark symptoms improves outcomes significantly, allowing for timely intervention and personalized treatment plans.
Core Symptoms: What to Watch For
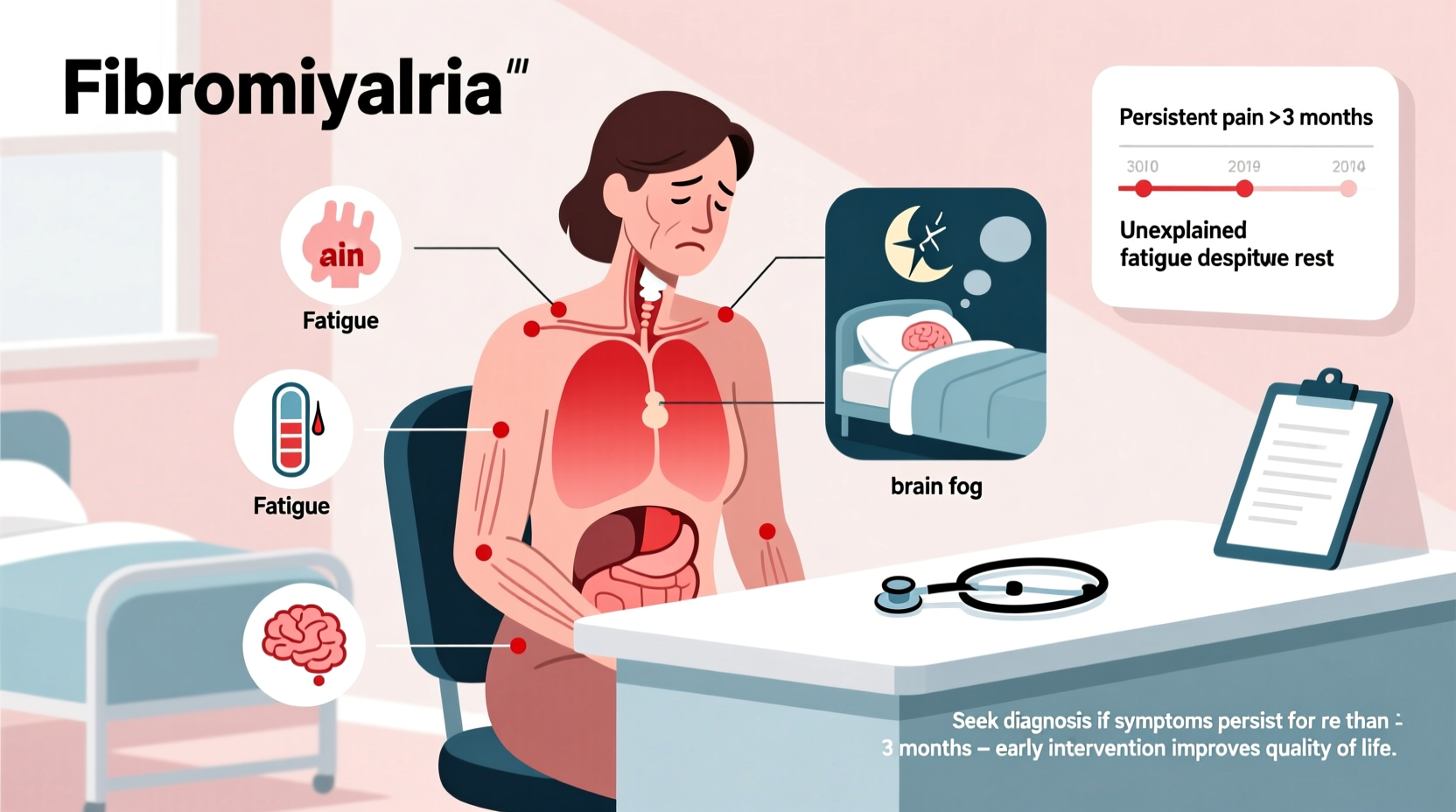
The symptoms of fibromyalgia vary from person to person, but several core indicators consistently appear across cases. These include:
- Widespread musculoskeletal pain: A constant dull ache lasting at least three months, occurring on both sides of the body and above and below the waist.
- Chronic fatigue: Even after full nights of sleep, individuals often wake up feeling unrefreshed. Sleep disturbances like restless legs syndrome or insomnia are common.
- Cognitive difficulties (“fibro fog”): Problems with memory, concentration, and task execution, particularly under stress or fatigue.
- Headaches and migraines: Frequent tension-type headaches or migraines are reported by over half of patients.
- Sensitivity to stimuli: Heightened reactions to noise, light, temperature, or touch.
- Mood disorders: Anxiety and depression frequently coexist with fibromyalgia, though they are not causes—rather, consequences of chronic pain and lifestyle disruption.
Lesser-Known Signs That May Indicate Fibromyalgia
Beyond the primary symptoms, many patients experience secondary issues that are often overlooked. These include:
- Irregular bowel habits (often linked with irritable bowel syndrome)
- Temporomandibular joint (TMJ) pain
- Numbness or tingling in hands and feet
- Menstrual pain that is more severe than usual
- Painful bladder syndrome or frequent urination
These symptoms don’t confirm fibromyalgia on their own, but when combined with widespread pain and fatigue, they form a recognizable cluster that warrants further investigation.
When to Seek a Diagnosis: Key Triggers
Many people dismiss fibromyalgia symptoms as normal aging, stress, or poor sleep hygiene. However, certain red flags should prompt immediate consultation with a healthcare provider:
- You’ve experienced persistent pain throughout your body for more than three months.
- Over-the-counter pain relievers provide little to no relief.
- Your ability to work, exercise, or perform household tasks has declined significantly.
- You’re struggling with mental clarity or memory, even without a prior neurological condition.
- You have a family history of fibromyalgia or autoimmune diseases.
- You’ve recently undergone physical trauma, surgery, infection, or significant emotional stress—all known potential triggers.
“Fibromyalgia is not ‘all in your head.’ It’s a real, diagnosable condition with measurable impacts on the nervous system. Delaying evaluation only prolongs suffering.” — Dr. Linda Russell, Rheumatologist at Johns Hopkins Medicine
Diagnosis Process: What to Expect
There is no single test for fibromyalgia. Doctors rely on a combination of patient history, physical assessment, and exclusion of other conditions. Blood tests may be ordered to rule out rheumatoid arthritis, lupus, hypothyroidism, or vitamin deficiencies. In the past, diagnosis involved checking 18 specific tender points, but modern criteria focus more on symptom severity and duration.
The American College of Rheumatology currently uses the following guidelines:
| Symptom Domain | Description | Scoring Threshold |
|---|---|---|
| Widespread Pain Index (WPI) | Number of painful areas out of 19 body regions | ≥7 |
| Severity Scale (SSS) | Measures fatigue, waking unrefreshed, cognitive issues | ≥5 |
| Symptom Duration | Symptoms present for at least 3 months | Required |
| Exclusion of Other Conditions | No alternative explanation for symptoms | Mandatory |
If your scores meet these thresholds and other conditions are ruled out, a diagnosis of fibromyalgia may be made. Seeing a rheumatologist increases the likelihood of an accurate assessment, especially if initial evaluations were inconclusive.
Real-Life Example: Sarah’s Journey to Diagnosis
Sarah, a 42-year-old teacher from Oregon, began experiencing morning stiffness and exhaustion five years ago. Initially, she attributed it to her busy schedule. Over time, the fatigue worsened, and sharp pains developed in her neck, back, and hips. She visited her primary care physician multiple times, receiving treatments for stress and mild depression. Blood tests showed no abnormalities.
After reading an article about fibromyalgia, Sarah noticed her symptoms aligned closely. She started tracking her pain and sleep, bringing detailed notes to a rheumatologist. Within one visit, she was evaluated using the WPI and SSS scales. With a WPI of 9 and SSS of 6, and no evidence of autoimmune disease, she received a fibromyalgia diagnosis.
Starting a tailored treatment plan—including low-dose medication, physical therapy, and mindfulness practices—Sarah regained much of her functionality within six months. Her case underscores the importance of self-advocacy and informed dialogue with specialists.
Action Plan: Steps to Take If You Suspect Fibromyalgia
If you're experiencing symptoms consistent with fibromyalgia, follow this checklist to move toward clarity and care:
- Document your symptoms: Use a notebook or app to log pain location, intensity, sleep quality, energy levels, and cognitive function daily.
- Review family history: Note any relatives with fibromyalgia, lupus, or chronic fatigue syndrome.
- Rule out other conditions: Request blood work to check for thyroid dysfunction, anemia, autoimmune markers, and vitamin D/B12 levels.
- Request a specialist referral: Ask your primary care provider for a rheumatology consult.
- Prepare for your appointment: Bring your symptom journal, list of medications, and questions about diagnosis criteria and treatment options.
- Explore multidisciplinary care: Consider input from physical therapists, pain specialists, or mental health professionals familiar with chronic illness.
Frequently Asked Questions
Can fibromyalgia go away on its own?
No, fibromyalgia is a chronic condition with no cure. However, symptoms can be managed effectively through medication, lifestyle changes, and therapy. Some people experience periods of remission where symptoms lessen significantly.
Is fibromyalgia considered a disability?
In some cases, yes. Severe fibromyalgia can impair the ability to work full-time. Individuals may qualify for disability benefits if they can demonstrate functional limitations supported by medical records and physician statements.
Are there natural ways to reduce fibromyalgia symptoms?
Yes. Regular low-impact exercise (like walking or swimming), stress reduction techniques (such as meditation or yoga), improved sleep hygiene, and a balanced diet rich in anti-inflammatory foods can help reduce symptom severity.
Conclusion: Take Control of Your Health
Recognizing the key signs of fibromyalgia is the first step toward reclaiming your quality of life. While the path to diagnosis can be frustrating, persistence pays off. Armed with knowledge, documentation, and a proactive mindset, you can work with healthcare providers to get the answers you need. Early intervention doesn’t eliminate fibromyalgia, but it empowers you to manage it effectively.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?