Heat stroke is a life-threatening medical emergency that occurs when the body overheats—typically above 104°F (40°C)—and can no longer regulate its temperature. Unlike milder forms of heat-related illness, such as heat exhaustion, heat stroke progresses rapidly and requires immediate intervention. Each year, thousands are hospitalized due to extreme heat exposure, many of which could have been prevented with early recognition and prompt action. Understanding the subtle and overt signs of heat stroke, knowing who is most at risk, and acting decisively can mean the difference between recovery and long-term health consequences—or worse.
Understanding Heat Stroke: How It Happens
The human body maintains a stable internal temperature through mechanisms like sweating and blood vessel dilation. When exposed to high temperatures—especially in humid conditions or during intense physical activity—these cooling systems can become overwhelmed. Sweating may not be enough to dissipate heat, particularly if dehydration sets in. As core temperature climbs, critical organs begin to suffer damage. The brain, heart, kidneys, and muscles are especially vulnerable.
There are two main types of heat stroke:
- Exertional heat stroke: Occurs in otherwise healthy individuals during intense physical activity in hot environments—common among athletes, military personnel, and outdoor laborers.
- Non-exertional (classic) heat stroke: Typically affects older adults, young children, or those with chronic illnesses during prolonged heat waves, often without significant physical exertion.
Both types demand urgent attention, but their onset and risk factors differ. Recognizing these distinctions helps in prevention and timely response.
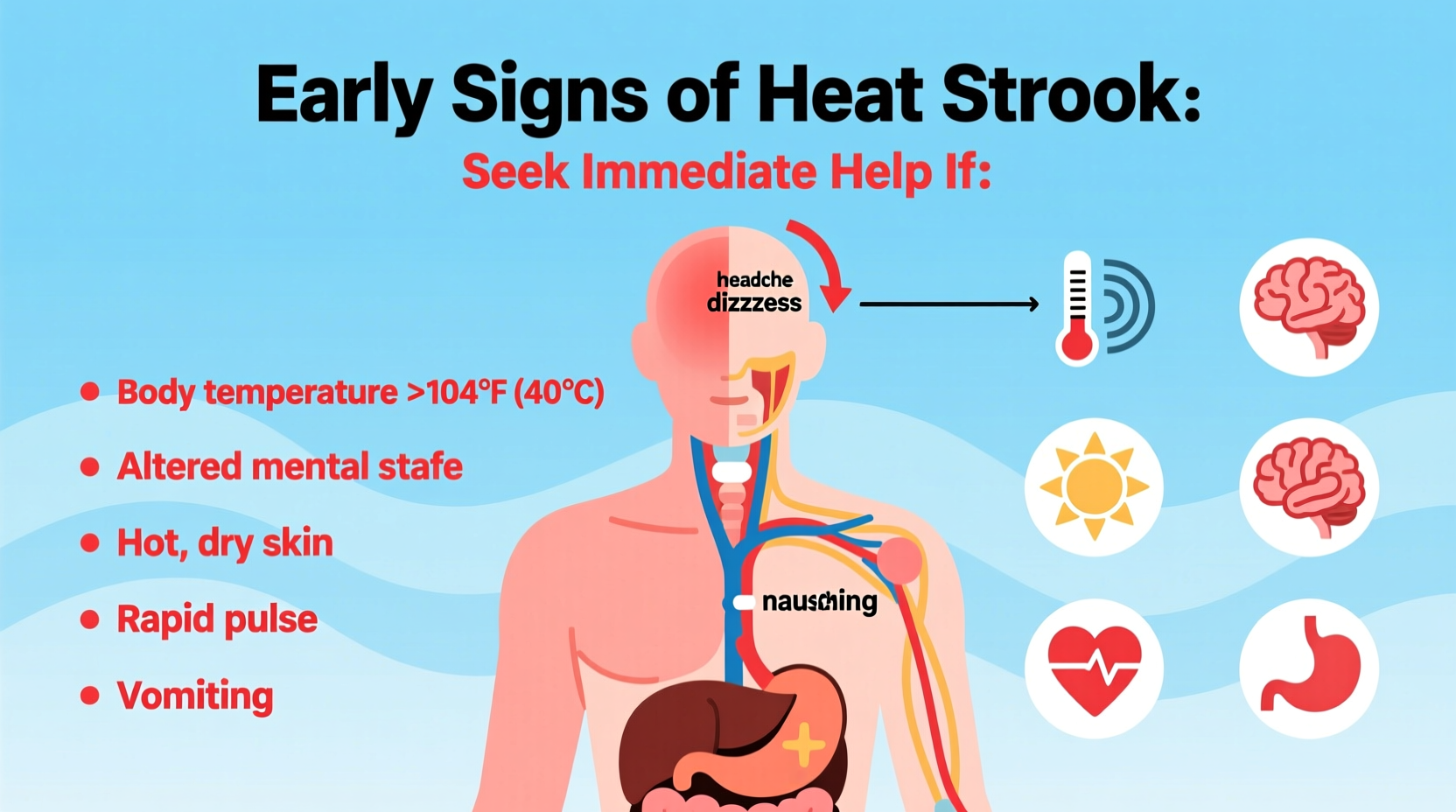
Key Early Warning Signs of Heat Stroke
Early detection is critical. Symptoms often start subtly and escalate quickly. Being alert to the progression from mild discomfort to severe distress can save lives.
The hallmark sign of heat stroke is an elevated core body temperature, but this isn’t always measurable in the field. Instead, rely on observable symptoms:
- High body temperature: A core temperature of 104°F or higher is diagnostic, though clinical confirmation may come later.
- Altered mental state: Confusion, agitation, slurred speech, irritability, delirium, seizures, or loss of consciousness are strong indicators.
- Hot, dry skin or profuse sweating: In classic heat stroke, skin is typically hot and dry due to failed sweating mechanisms. In exertional cases, the person may still be sweating heavily.
- Rapid pulse and breathing: The heart races to cool the body, leading to tachycardia and hyperventilation.
- Nausea or vomiting: Gastrointestinal distress is common as organ systems begin to falter.
- Flushed skin: Skin may appear red as blood vessels dilate in a failing attempt to release heat.
- Headache: Often severe and throbbing, caused by increased intracranial pressure and dehydration.
Unlike heat exhaustion, where a person remains alert and sweaty with cooler skin, heat stroke involves neurological compromise. This distinction is vital for determining urgency.
Distinguishing Heat Stroke from Heat Exhaustion
| Symptom | Heat Exhaustion | Heat Stroke |
|---|---|---|
| Body Temperature | Up to 103°F (39.4°C) | 104°F+ (40°C+) |
| Skin Condition | Cool, moist, pale | Hot, dry, or sweaty (exertional) |
| Mental Status | Anxious, fatigued, but alert | Confused, disoriented, unconscious |
| Pulse | Fast and weak | Rapid and strong |
| Response to Cooling | Improves with rest and fluids | No improvement; worsens without emergency care |
When to Seek Immediate Medical Help
If someone displays signs of altered mental status along with high body temperature, assume it is heat stroke and act immediately. Do not wait for all symptoms to appear.
Call emergency services (e.g., 911) if the person:
- Loses consciousness or cannot be awakened
- Is confused or speaking incoherently
- Has stopped sweating and has hot, dry skin (in non-exertional cases)
- Is experiencing seizures
- Shows no improvement after 30 minutes of cooling efforts
“Time is brain in heat stroke. Every minute delay increases the risk of permanent neurological injury or death.” — Dr. Rafael Medina, Emergency Medicine Physician
Immediate First Aid Steps While Waiting for Help
- Move to a cooler environment: Get the person indoors or into shade immediately.
- Remove excess clothing: Loosen or take off clothes to facilitate heat loss.
- Cool rapidly: Use any available method—immerse in cool water, spray with a hose, apply ice packs to neck, armpits, and groin, or fan while misting with water.
- Do not give fluids if unconscious: Avoid giving water or sports drinks if the person is vomiting or unresponsive due to choking risk.
- Monitor breathing: Be prepared to perform CPR if breathing stops.
Do not rely on fever-reducing medications like ibuprofen or acetaminophen—they are ineffective and potentially harmful in heat stroke.
Vulnerable Populations and Prevention Strategies
While anyone can suffer heat stroke, certain groups face higher risks:
- Infants and children under 4 years old
- Adults over 65
- People with chronic conditions (heart disease, obesity, diabetes, respiratory issues)
- Those taking medications that impair thermoregulation (diuretics, antihistamines, beta-blockers)
- Athletes and outdoor workers
Prevention Checklist
- Stay hydrated with water throughout the day—avoid alcohol and caffeine.
- Wear lightweight, loose-fitting, light-colored clothing.
- Limit outdoor activity during peak heat (10 a.m. to 4 p.m.).
- Use air conditioning or cooling centers when possible.
- Never leave anyone—especially children or pets—in a parked car.
- Acclimatize gradually to hot environments over 7–14 days.
- Monitor urine color—pale yellow indicates good hydration.
Real-Life Scenario: A Coach’s Quick Response Saves a Player
During a late summer football practice in Texas, 16-year-old Marcus began stumbling during drills. He complained of a headache and nausea. His coach noticed his skin was flushed and unusually hot, despite heavy sweating. When Marcus became confused and couldn’t recall the play, the coach recognized the signs of exertional heat stroke.
Without hesitation, he called 911, moved Marcus to the shaded training room, and began aggressive cooling using ice towels and a fan. Paramedics arrived within 12 minutes and confirmed a core temperature of 105.1°F. Thanks to the rapid response, Marcus recovered fully after two days in the hospital.
This case underscores the importance of education and preparedness. The school later implemented mandatory heat safety training for all coaches, including recognition drills and access to cooling tubs.
Frequently Asked Questions
Can heat stroke occur indoors?
Yes. Non-exertional heat stroke commonly occurs in homes without air conditioning during heat waves. Poor ventilation and high indoor humidity increase risk, especially for elderly individuals living alone.
Is it safe to resume activity after recovering from heat stroke?
Only under medical supervision. Recovery can take weeks, and susceptibility to future episodes increases. Doctors often recommend avoiding strenuous activity in heat for at least one month.
Are sports drinks better than water for preventing heat illness?
For prolonged activity (over 60–90 minutes), electrolyte-containing drinks can help maintain balance. However, water remains the best choice for general hydration. Overconsumption of sugary sports drinks can impair fluid absorption.
Act Now to Prevent Tragedy
Heat stroke doesn’t announce itself gently. It escalates silently, then strikes with devastating speed. But with awareness, vigilance, and swift action, it is largely preventable and treatable. Whether you’re a parent, caregiver, athlete, or worksite supervisor, your ability to recognize the early signs could protect someone’s life.
Share this knowledge with your community. Advocate for cooling stations at events. Install window shades or fans in homes without AC. Most importantly, trust your instincts—if something feels dangerously wrong in the heat, it probably is.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?