Dissociative Identity Disorder (DID), formerly known as multiple personality disorder, is a complex psychological condition that stems from severe trauma during early childhood, usually extreme, repetitive physical, sexual, or emotional abuse. It’s characterized by the presence of two or more distinct identities or personality states that recurrently take control of an individual’s behavior. Recognizing the signs early can make a critical difference in recovery and long-term well-being.
Despite its portrayal in popular media—often dramatized or misrepresented—DID is a legitimate and diagnosable mental health condition. Understanding its symptoms, knowing when to be concerned, and taking steps toward professional support are essential for anyone affected or supporting someone who may be struggling.
Understanding Dissociative Identity Disorder
DID is classified under dissociative disorders in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). The core feature is a disruption of identity involving two or more distinct personality states. These states may have unique names, ages, genders, mannerisms, voices, and even physiological responses.
The transitions between these identities—often called “switching”—are typically accompanied by gaps in memory, known as amnesia barriers. A person with DID might not recall conversations, actions, or events that occurred while another identity was present. This isn’t simple forgetfulness; it’s a profound dissociation from consciousness and continuity of self.
Dissociation itself is a coping mechanism. In children exposed to chronic trauma, the mind may “split off” experiences as a way to survive overwhelming pain. Over time, this can evolve into fully formed alternate identities, each serving a protective or functional role.
“DID is not about theatrical performance or manipulation. It’s a survival strategy developed in childhood under conditions of extreme helplessness.” — Dr. Bethany Brand, Clinical Psychologist and DID Researcher
Key Signs and Symptoms of DID
Recognizing DID requires attention to subtle, often overlapping behaviors. Many symptoms mimic other conditions like depression, anxiety, PTSD, or bipolar disorder, which can lead to misdiagnosis. However, certain patterns point specifically to dissociation and identity fragmentation.
- Memory lapses beyond ordinary forgetfulness: Forgetting important personal information, daily activities, or entire periods of time.
- Distinct shifts in behavior, speech, or mood: Sudden changes in tone, preferences, or values that seem inconsistent with the person’s usual self.
- Hearing internal voices: Some individuals report hearing multiple voices inside their head, arguing or commenting on their actions.
- Feeling detached from oneself (depersonalization): Descriptions like “watching myself from outside” or feeling robotic.
- Unexplained possessions or behaviors: Finding items they don’t remember buying or being told they said things they don’t recall.
- Time loss: Waking up in unfamiliar places with no memory of how they got there.
- Self-harming behaviors or unexplained injuries: Often linked to identities that carry trauma or engage in self-punishment.
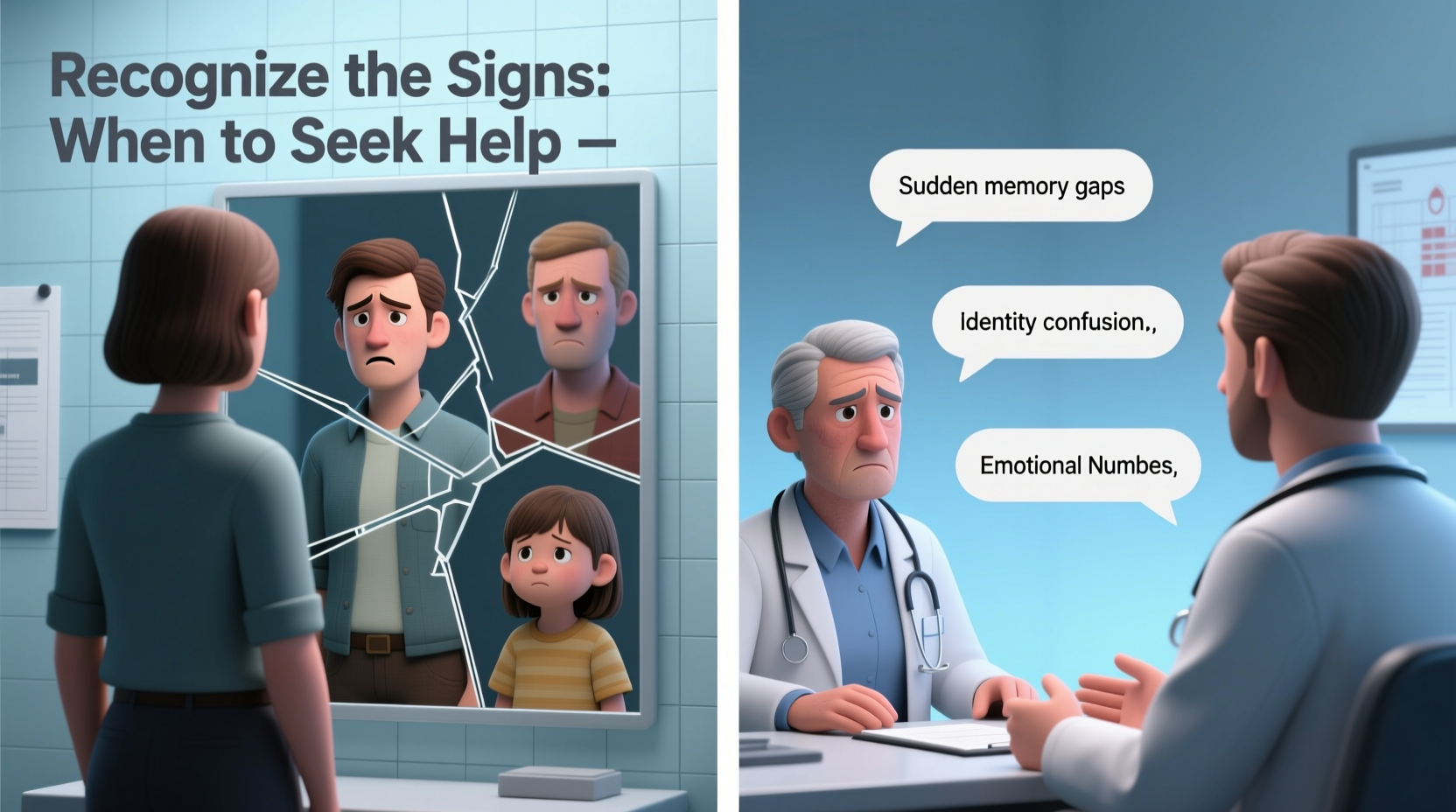
When to Seek Professional Help
Early intervention significantly improves outcomes for people with DID. Because the disorder often develops in childhood but goes undiagnosed for years—even decades—many live with confusion, shame, and isolation before receiving proper care.
Seek help if you or someone close to you experiences:
- Repeated episodes of unexplained memory loss affecting work, relationships, or safety.
- Observable switches in voice, demeanor, or handwriting.
- History of childhood trauma combined with ongoing mental health struggles.
- Co-occurring symptoms like depression, anxiety, PTSD, or suicidal thoughts.
- Diagnoses that don’t fully explain the symptoms, especially after trying multiple treatments.
A licensed mental health professional trained in trauma and dissociation—such as a clinical psychologist or psychiatrist—can conduct a thorough assessment. Tools like the Structured Clinical Interview for DSM-5 Dissociative Disorders (SCID-D) are used to evaluate dissociative symptoms reliably.
Mini Case Study: Sarah’s Journey to Diagnosis
Sarah, a 34-year-old teacher, began therapy for severe anxiety and depression. She reported frequent blackouts, finding handwritten notes in different penmanship, and being reprimanded at work for saying things she didn’t remember. Her therapist noticed sudden shifts in her speech and affect during sessions—sometimes soft-spoken and childlike, other times angry and defensive.
After ruling out neurological conditions and using the SCID-D, Sarah was diagnosed with DID. Her alters—some protective, others holding memories of abuse—had formed in response to years of childhood neglect and violence. With specialized trauma therapy, Sarah began integrating her identities and reclaiming continuity of memory and self.
Her case underscores the importance of looking beyond surface symptoms. Without a trauma-informed approach, her DID might have remained hidden behind labels like “bipolar” or “borderline,” leading to ineffective treatment.
Do’s and Don’ts When Supporting Someone with DID
| Do | Don’t |
|---|---|
| Listen without judgment when they share experiences. | Challenge or argue with an alter identity. |
| Respect the presence of different identities as part of their reality. | Try to force a switch or “bring out” a specific identity. |
| Encourage professional treatment with a trauma specialist. | Minimize their symptoms as “acting” or attention-seeking. |
| Help maintain routines and grounding techniques during stress. | Share their diagnosis with others without consent. |
| Be patient—integration and healing take time. | Expect quick fixes or complete “cure” of all identities. |
Step-by-Step Guide to Getting Help
If you suspect DID in yourself or someone else, follow these steps to access appropriate care:
- Document symptoms: Keep a journal of memory gaps, behavioral changes, or unusual experiences. Note frequency and triggers.
- Consult a general mental health provider: Start with a therapist or psychiatrist familiar with trauma, even if they aren’t a DID specialist.
- Request a dissociative disorders screening: Ask specifically for tools like the Dissociative Experiences Scale (DES) or SCID-D.
- Seek a specialist: Look for clinicians certified by organizations like the International Society for the Study of Trauma and Dissociation (ISSTD).
- Begin trauma-focused therapy: Treatments such as Phase-Oriented Therapy focus first on safety, then trauma processing, and finally integration or functional collaboration among identities.
- Build a support system: Involve trusted friends or family members, with the individual’s permission, to create a stable environment.
Frequently Asked Questions
Is DID the same as schizophrenia?
No. Schizophrenia is a psychotic disorder involving delusions, hallucinations, and disorganized thinking, but not multiple identities. People with DID experience dissociation, not psychosis. Hearing “voices” in DID refers to internal identities, whereas in schizophrenia, voices are perceived as external.
Can DID develop in adulthood?
No. The condition originates in early childhood, typically before age 6–9, as a response to prolonged trauma. While symptoms may not become apparent until adolescence or adulthood, the dissociative patterns form during developmental years.
Do all people with DID have violent alters?
No. This is a myth perpetuated by media. Most alters are not violent. Some may express anger as a protective response, but the vast majority are focused on survival, protection, or managing daily life.
Conclusion: Take Action with Compassion and Clarity
Recognizing the signs of dissociative identity disorder is the first step toward healing. Misunderstanding and stigma still surround DID, but informed awareness can transform lives. Whether you’re concerned about yourself or someone you care about, reaching out to a qualified mental health professional is not a sign of weakness—it’s an act of courage.
Trauma survivors deserve compassionate, evidence-based care. With proper diagnosis and therapy, people with DID can achieve stability, reduce distress, and live fulfilling lives. Healing is possible—not by erasing parts of the self, but by integrating them into a cohesive whole.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?