Brain fog—characterized by mental fatigue, poor concentration, memory lapses, and a general sense of mental cloudiness—is not a medical diagnosis but a common symptom affecting millions. While stress, sleep deprivation, and hormonal imbalances contribute, emerging cognitive research highlights diet as a central modifiable factor. The foods we eat directly influence neurotransmitter production, inflammation levels, gut-brain communication, and cerebral blood flow. By aligning your diet with neuroscience-backed principles, you can significantly reduce brain fog and enhance cognitive resilience.
The Science Behind Diet and Cognitive Function
The brain consumes about 20% of the body’s energy despite accounting for only 2% of its weight. This high metabolic demand makes it especially sensitive to nutritional deficiencies and inflammatory triggers. Cognitive research shows that chronic consumption of processed foods, refined sugars, and trans fats promotes systemic inflammation and oxidative stress—both linked to impaired neuronal function and reduced neuroplasticity.
Conversely, diets rich in antioxidants, omega-3 fatty acids, fiber, and phytonutrients support brain health by reducing neuroinflammation, enhancing mitochondrial efficiency, and promoting the growth of beneficial gut microbiota. The gut-brain axis plays a pivotal role: approximately 90% of serotonin, a key neurotransmitter for mood and cognition, is produced in the gut. Disruptions in gut health due to poor diet can therefore manifest as brain fog.
“Nutrition is one of the most powerful levers we have for influencing brain health. What you eat today shapes your cognitive trajectory tomorrow.” — Dr. Lisa Mosconi, Director of the Women’s Brain Initiative and author of *The XX Brain*
Foods That Fuel Mental Clarity
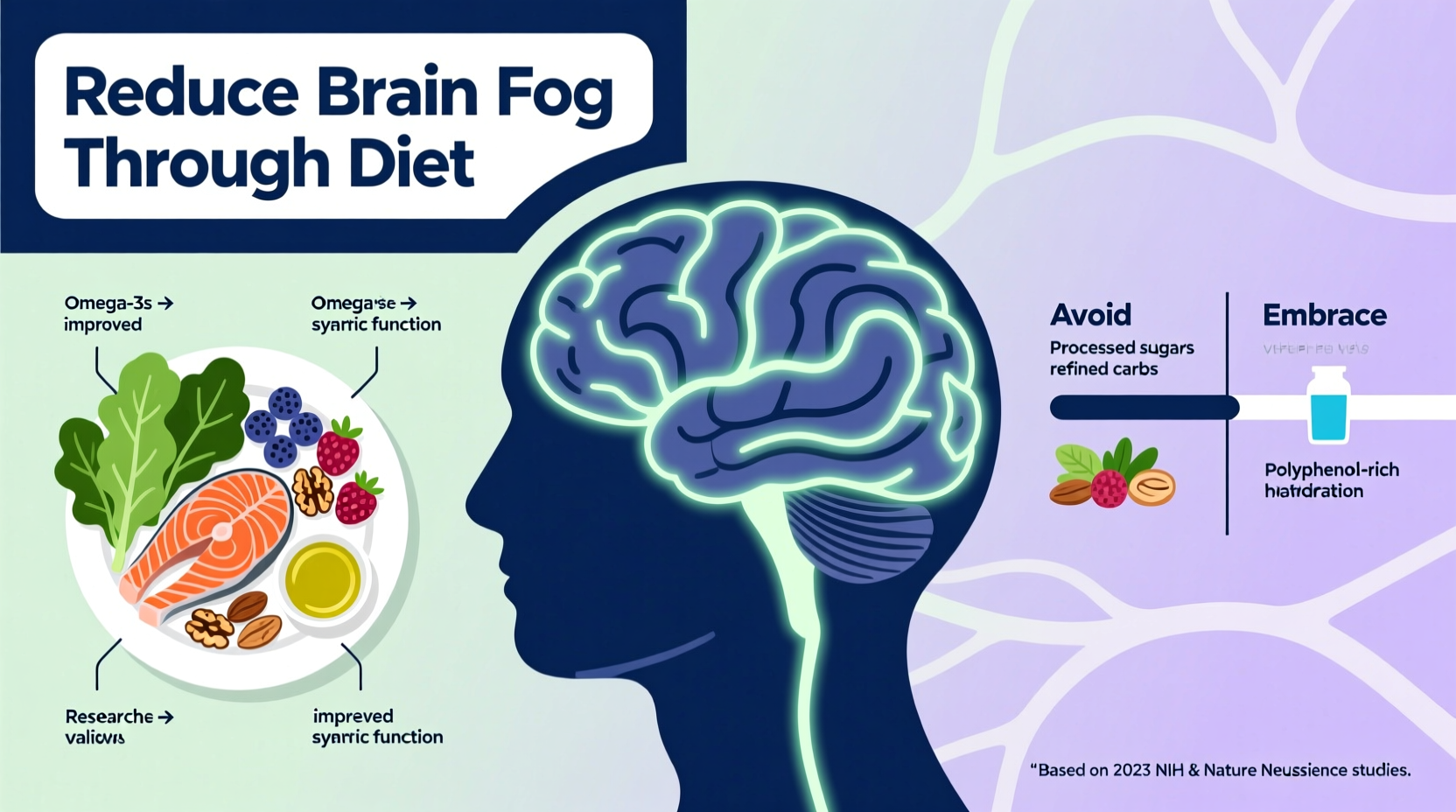
Certain foods consistently emerge in cognitive research as promoters of sharp thinking and sustained focus. These are not miracle cures but components of a synergistic dietary pattern that nourishes the brain at a cellular level.
- Fatty fish (salmon, mackerel, sardines): High in EPA and DHA, essential omega-3 fatty acids that integrate into neuronal membranes and support synaptic function. A 2020 meta-analysis in Nutrients found that higher omega-3 intake correlates with improved processing speed and executive function.
- Leafy greens (kale, spinach, Swiss chard): Packed with folate, vitamin K, and lutein—nutrients associated with slower cognitive decline. The MIND diet study showed participants who ate leafy greens daily had the cognitive equivalent of being 11 years younger than those who rarely consumed them.
- Blueberries: Rich in anthocyanins, potent antioxidants that cross the blood-brain barrier and reduce oxidative stress in the hippocampus, the brain’s memory center.
- Extra virgin olive oil: Contains oleocanthal, which has anti-inflammatory and neuroprotective properties. Studies link Mediterranean-style olive oil consumption to lower risks of cognitive impairment.
- Nuts and seeds (walnuts, flaxseeds, pumpkin seeds): Provide zinc, magnesium, and plant-based omega-3s. Walnuts, in particular, have been shown in randomized trials to improve inferential reasoning and working memory.
- Fermented foods (kefir, sauerkraut, kimchi): Support a diverse gut microbiome, which produces short-chain fatty acids like butyrate—known to reduce neuroinflammation and strengthen the blood-brain barrier.
Dietary Patterns Proven to Reduce Brain Fog
While individual superfoods help, long-term cognitive benefits come from consistent eating patterns. Three dietary frameworks stand out in cognitive research:
- Mediterranean Diet: Emphasizes whole grains, legumes, vegetables, fruits, nuts, olive oil, and fish while limiting red meat and processed foods. A 2023 study in Neurology found that older adults adhering closely to this pattern had 23% lower odds of subjective cognitive decline.
- MIND Diet (Mediterranean-DASH Intervention for Neurodegenerative Delay): Combines elements of the Mediterranean and DASH diets with a specific focus on brain-healthy foods. It prioritizes berries over other fruits and recommends at least two weekly servings of leafy greens. Participants following the MIND diet showed up to a 53% reduction in Alzheimer’s risk.
- Low-Glycemic Index (Low-GI) Eating: Stabilizes blood sugar by avoiding rapid spikes and crashes that impair attention and trigger fatigue. Research from the American Journal of Clinical Nutrition indicates that low-GI diets improve memory performance and reaction time compared to high-GI diets.
What to Avoid: Foods That Worsen Brain Fog
Just as important as what you add is what you eliminate. Certain foods disrupt neural signaling and promote inflammation.
| Foods to Avoid | Why They Harm Cognition | Better Alternatives |
|---|---|---|
| Refined sugars (soda, candy, pastries) | Cause insulin spikes and oxidative stress; linked to hippocampal shrinkage | Fresh fruit, small amounts of honey or maple syrup |
| Ultra-processed foods (chips, frozen meals, fast food) | High in trans fats and additives that increase neuroinflammation | Whole, single-ingredient foods |
| Excessive alcohol | Impairs neurotransmission and damages the prefrontal cortex | Occasional moderate wine (especially red), or non-alcoholic alternatives |
| Artificial sweeteners (aspartame, sucralose) | May alter gut microbiota and impair glucose regulation in the brain | Stevia (in moderation), monk fruit |
Step-by-Step Guide to Transitioning Your Diet
Changing your diet doesn’t require overnight perfection. A gradual, sustainable approach yields better long-term results. Follow this four-week timeline to reset your brain nutrition:
- Week 1: Eliminate the Worst Offenders
Remove sugary beverages, processed snacks, and industrial seed oils (like soybean or corn oil). Replace soda with sparkling water infused with lemon or cucumber. Swap chips for raw veggies with hummus. - Week 2: Add One Brain-Boosting Food Daily
Incorporate a serving of fatty fish, leafy greens, or berries each day. Start with simple additions: add spinach to your morning smoothie or top yogurt with blueberries. - Week 3: Optimize Meal Timing and Balance
Structure meals around protein + healthy fat + fiber. For example: grilled salmon (protein/fat) with quinoa and roasted broccoli (fiber). Avoid skipping meals to prevent blood sugar dips that trigger fogginess. - Week 4: Introduce Fermented Foods and Hydration Focus
Add a daily serving of kefir, sauerkraut, or kombucha. Simultaneously, aim for at least 2 liters of water daily—dehydration as mild as 2% impairs attention and short-term memory.
Real-Life Example: Maria’s Cognitive Turnaround
Maria, a 42-year-old project manager, struggled with persistent brain fog that made meetings overwhelming and deadlines stressful. She often skipped breakfast, relied on coffee and pastries, and ate takeout several nights a week. After consulting a functional medicine practitioner, she began tracking her symptoms alongside dietary changes.
Within three weeks of eliminating processed foods, adding leafy greens at lunch, and eating salmon twice weekly, Maria reported sharper focus and fewer mid-afternoon crashes. By week six, she no longer needed afternoon naps and felt confident leading complex discussions. Her experience mirrors clinical findings: dietary interventions can yield noticeable cognitive improvements in under a month.
Checklist: Build Your Anti-Brain-Fog Diet
Use this checklist to guide your daily choices:
- ✅ Eat at least 2 cups of leafy greens per day
- ✅ Include omega-3-rich foods (fish, flaxseed, walnuts) at least 3 times per week
- ✅ Limit added sugar to under 25g per day
- ✅ Drink water consistently—aim for pale yellow urine
- ✅ Consume one fermented food daily
- ✅ Choose whole grains over refined carbs (e.g., brown rice instead of white)
- ✅ Prepare one home-cooked meal per day using fresh ingredients
- ✅ Avoid eating within 3 hours of bedtime to support overnight brain detoxification
FAQ: Common Questions About Diet and Brain Fog
Can going gluten-free help reduce brain fog?
For individuals with celiac disease or non-celiac gluten sensitivity, eliminating gluten can dramatically improve cognitive symptoms. However, for the general population, there’s limited evidence that gluten causes brain fog. Unnecessarily restrictive diets may lead to nutrient gaps. If considering a gluten-free trial, consult a healthcare provider and monitor symptoms for at least four weeks.
How quickly can diet changes improve mental clarity?
Many people report subtle improvements in focus and energy within 1–2 weeks of removing processed foods and stabilizing blood sugar. More significant gains in memory and processing speed typically emerge after 4–6 weeks of consistent, brain-supportive eating. Individual responses vary based on baseline diet, gut health, and lifestyle factors.
Are supplements necessary if I eat a good diet?
While food should be the primary source of nutrients, some individuals benefit from targeted supplementation—especially if deficient. Vitamin B12 (critical for nerve function), vitamin D (linked to cognitive health), and omega-3s (if fish intake is low) are commonly recommended. Always test before supplementing and work with a qualified professional to avoid imbalances.
Conclusion: Take Control of Your Cognitive Health
Brain fog is not an inevitable part of modern life. Cognitive research overwhelmingly supports the idea that diet is a foundational pillar of mental clarity. By shifting toward whole, anti-inflammatory foods and away from processed, sugar-laden options, you create the internal environment your brain needs to thrive. These changes don’t require perfection—just consistency and intention.
You don’t need a dramatic overhaul to see results. Start with one meal, one swap, or one new habit. Over time, these small choices compound into lasting cognitive resilience. Your brain is listening to every bite you take. Make sure it’s hearing nourishment.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?