In today’s digital healthcare environment, patient data flows through electronic systems, mobile devices, and verbal conversations across hospital departments. While technology improves care coordination, it also increases the risk of sensitive medical information being exposed. Families and caregivers play a crucial role in safeguarding this information—not just for legal compliance, but to preserve dignity, trust, and safety. Understanding how health records are stored, shared, and protected empowers you to act as an informed advocate while minimizing risks of unauthorized access or breaches.
Understanding Patient Privacy and HIPAA Basics
The Health Insurance Portability and Accountability Act (HIPAA) sets the national standard for protecting patient health information in the United States. It restricts who can access medical records, under what conditions they can be shared, and how long they must be secured. As a family member or caregiver, you may be granted authorized access—but only with proper consent from the patient or legal representative.
HIPAA defines “protected health information” (PHI) as any data that identifies a patient and relates to their physical or mental health, treatment history, or payment for care. This includes names, dates of birth, diagnosis reports, lab results, insurance details, and even appointment schedules.
“Privacy isn’t just about locking files—it’s about awareness. One misplaced conversation in a hallway can violate HIPAA just as much as a hacked database.” — Dr. Linda Tran, Hospital Compliance Officer
You don’t need to memorize every regulation, but knowing that PHI must remain confidential, used only for treatment or necessary operations, and disclosed only with permission is essential when supporting a loved one.
How Hospitals Protect Patient Data: Behind the Scenes
Modern hospitals use layered security strategies to protect patient information. These include:
- Encryption: All electronic records are encrypted both at rest (stored) and in transit (being sent).
- Access Controls: Staff log in using unique credentials, and permissions are based on job roles—doctors see more than janitorial staff.
- Audit Trails: Every time a record is viewed or modified, the system logs who accessed it and when.
- Secure Networks: Wi-Fi systems used by medical staff are isolated from public guest networks.
- Training: Employees undergo regular HIPAA training and sign confidentiality agreements.
Despite these measures, human error remains the leading cause of data exposure. A nurse leaving a workstation unlocked, a doctor discussing a case in an elevator, or a printed chart left unattended can all compromise privacy.
Practical Steps for Families and Caregivers
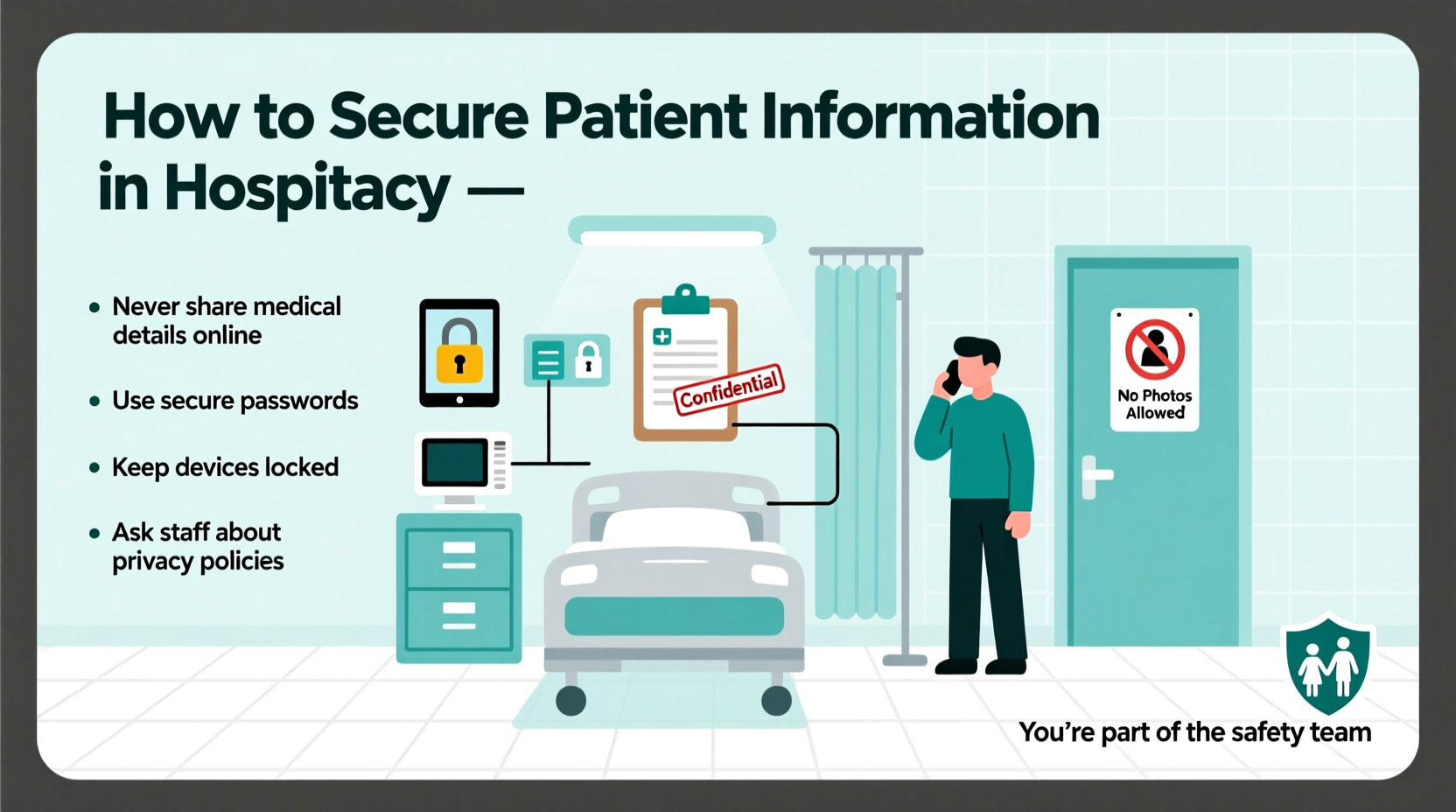
Your actions directly influence how safely patient information is handled. Here’s what you can do to support security efforts:
1. Limit Sharing Outside Authorized Channels
Only discuss the patient’s condition with individuals directly involved in care or those explicitly approved by the patient. Avoid posting updates on social media—even seemingly vague posts like “Mom had surgery today” can reveal too much when combined with other clues.
2. Verify Identity Before Disclosing Information
If someone claims to be from the hospital, ask for their name, department, and employee ID. Call the main hospital line to confirm their identity before sharing anything. Scammers often pose as billing clerks or insurance agents.
3. Use Secure Communication Methods
When receiving test results or instructions, prefer secure patient portals over email or text messages unless encrypted options are confirmed. If using phone calls, step away from crowded areas to prevent eavesdropping.
4. Handle Paper Documents Carefully
Pick up any forms, discharge instructions, or prescriptions immediately after appointments. Shred old documents containing personal health details instead of tossing them in the trash.
5. Monitor Access to Digital Devices
If you’re managing a patient’s smartphone, tablet, or laptop, ensure it has a passcode, biometric lock, and updated software. Avoid saving login details for medical apps in browsers.
Checklist: Securing Patient Information – What You Should Do
- Confirm the patient has signed appropriate release forms if you need access to records.
- Use hospital-approved communication tools (e.g., patient portal) for updates.
- Never leave medical paperwork unattended in cars, bags, or public spaces.
- Ask staff to lower their voice if discussing the patient near others.
- Report suspicious behavior (e.g., unknown persons asking detailed medical questions).
- Enable two-factor authentication on any health-related accounts.
- Review privacy settings on wearable health devices (like smartwatches).
Common Risks and How to Avoid Them
| Risk | Why It's Dangerous | How to Prevent It |
|---|---|---|
| Talking in public areas | Eavesdroppers can gather identifying details | Move conversations to private rooms or wait until off-site |
| Using personal email for medical info | Emails can be intercepted or forwarded accidentally | Use secure messaging via the hospital portal |
| Carrying unsecured USB drives with records | Lost drives expose full medical histories | Avoid storing PHI on portable devices; use cloud storage with encryption |
| Sharing updates on social media | Photos or check-ins reveal location and status | Post only after discharge and without identifiable details |
Real-Life Scenario: A Preventable Breach
Sarah visited her father daily during his recovery from heart surgery. To keep relatives informed, she created a private Facebook group and posted updates like, “Dad is responding well to medication X,” along with photos showing the hospital room number. A friend shared the post outside the group, and days later, Sarah received a call from a reporter asking specific questions about her father’s treatment plan.
Though no official breach occurred within the hospital, Sarah unknowingly exposed protected information. After speaking with a patient advocate, she deleted the posts and switched to using the hospital’s secure family update system—reducing risk while keeping loved ones informed.
Frequently Asked Questions
Can I access my elderly parent’s medical records?
Yes, but only if they’ve granted you formal authorization through a HIPAA release form or you have legal power of attorney. Without documentation, hospitals cannot share details—even with immediate family.
What should I do if I see a nurse’s station computer left open?
Do not touch the screen. Notify any nearby staff immediately so they can lock the device. Unattended workstations are a common source of accidental data exposure.
Is it safe to use the hospital’s Wi-Fi to check medical results?
Public hospital Wi-Fi is generally not secure for accessing sensitive accounts. Avoid logging into patient portals or sending personal information unless connected to a trusted, password-protected network or using a virtual private network (VPN).
Final Thoughts: Your Role Matters
Securing patient information isn’t solely the hospital’s responsibility—it’s a shared effort. As a family member or caregiver, your vigilance helps close gaps that policies alone cannot cover. From resisting the urge to overshare online to questioning unfamiliar requests for information, small choices add up to meaningful protection.
Data breaches erode trust and can lead to identity theft, emotional distress, or discrimination. By treating every piece of medical information as sensitive, you honor the patient’s autonomy and contribute to a culture of privacy.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?