The human papillomavirus (HPV) vaccine has become a standard part of pediatric preventive care in many countries, yet confusion remains among parents about whether it’s required, when to get it, and most importantly—why it matters. While not universally mandated for school entry, the HPV vaccine is strongly recommended by leading health organizations as a critical tool in preventing several types of cancer later in life. Understanding its role, timing, and benefits can help parents make informed decisions that protect their children long-term.
Understanding HPV and Its Risks
Human papillomavirus is the most common sexually transmitted infection in the world. According to the Centers for Disease Control and Prevention (CDC), nearly all sexually active individuals will contract at least one strain of HPV at some point, often without symptoms. While most infections clear on their own, persistent infections with high-risk strains can lead to serious health issues—including cervical, anal, throat, penile, vaginal, and vulvar cancers.
Each year in the United States, HPV causes approximately 45,000 new cancer diagnoses. What many don’t realize is that these cancers develop decades after initial infection, which is why prevention during childhood is so effective. The virus spreads through intimate skin-to-skin contact, not necessarily full sexual intercourse, making early vaccination before exposure the best defense.
“HPV vaccination is cancer prevention. We have a real opportunity to reduce the burden of several cancers by vaccinating adolescents before they’re exposed.” — Dr. Nancy Messonnier, Former Director, National Center for Immunization and Respiratory Diseases, CDC
Is the HPV Vaccine Mandatory for Kids?
No, the HPV vaccine is not federally or universally mandatory for school attendance in the United States. Unlike vaccines for measles or polio, which are required in most states for public school enrollment, HPV vaccine requirements vary significantly by state. As of 2024, only a few states—including Rhode Island, Virginia, and the District of Columbia—have implemented mandates, typically allowing exemptions for medical, religious, or personal beliefs.
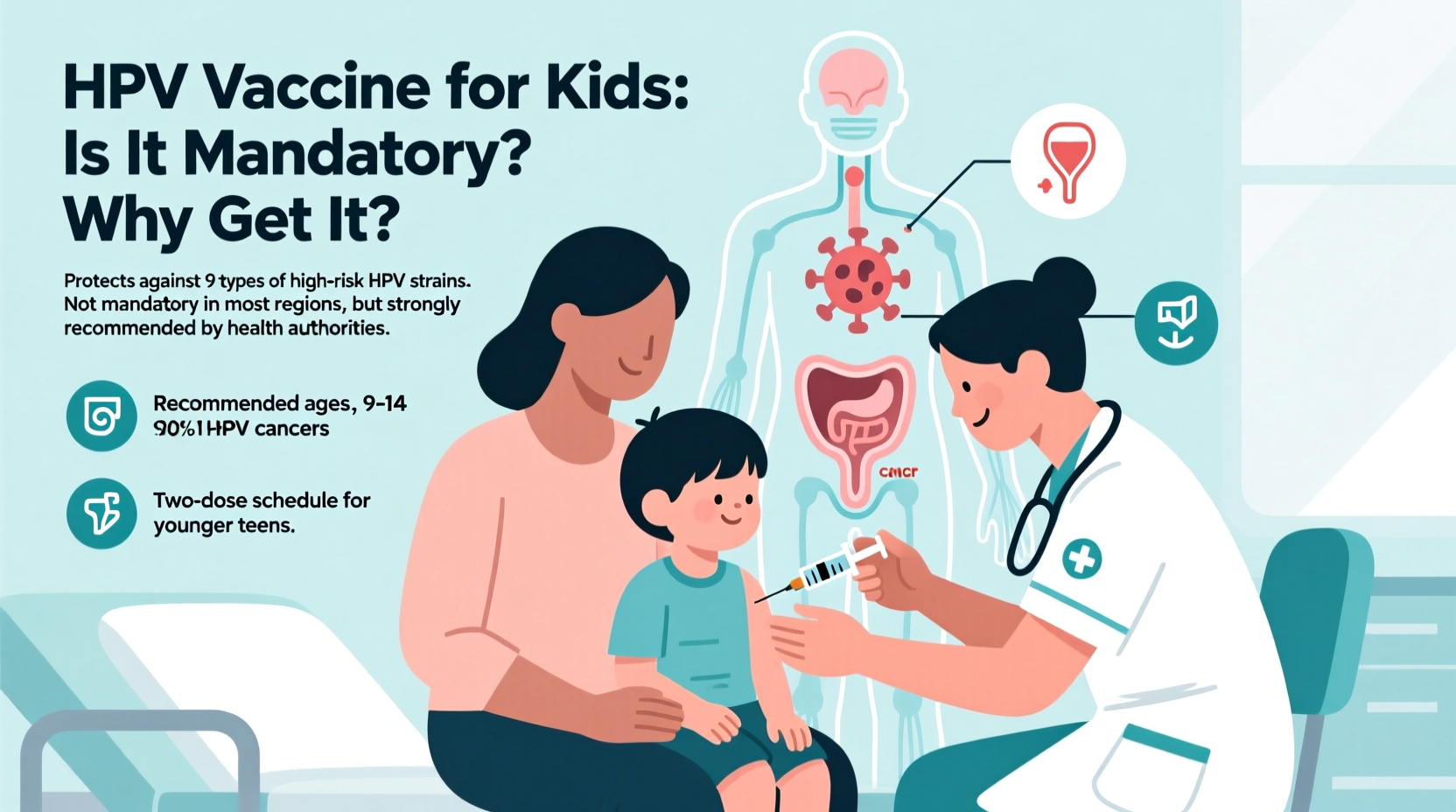
Despite the lack of widespread mandates, the CDC, American Academy of Pediatrics (AAP), and World Health Organization (WHO) all recommend routine HPV vaccination for boys and girls starting at age 11 or 12. Some children may receive it as early as age 9, especially if they are immunocompromised or at higher risk.
The absence of a mandate doesn’t diminish the vaccine’s importance. Public health experts emphasize that voluntary uptake based on education and trust leads to more sustainable, long-term acceptance than compulsory policies.
Why Get the HPV Vaccine? Key Benefits
The primary reason to vaccinate children against HPV is cancer prevention. The current vaccine, Gardasil 9, protects against nine strains of HPV responsible for over 90% of HPV-related cancers and genital warts. When administered at the recommended age, it provides near-complete protection from these strains.
- Highly effective: Studies show the vaccine reduces HPV infection rates by over 85% and precancerous cervical lesions by up to 97% in vaccinated populations.
- Long-lasting immunity: Research indicates protection lasts at least 12 years, with no evidence of waning immunity.
- Herd immunity: Widespread vaccination reduces transmission across communities, protecting even unvaccinated individuals.
- Cost-effective: Preventing cancer through vaccination is far less expensive than treating advanced disease.
Vaccination Schedule and Effectiveness by Age
The timing of the HPV vaccine is crucial. The immune response is strongest in early adolescence, and vaccination before any potential exposure ensures maximum protection. The CDC recommends the following schedule:
| Age at First Dose | Doses Required | Interval Between Doses |
|---|---|---|
| 9–14 years | 2 doses | 6–12 months apart |
| 15 years and older | 3 doses | 0, 1–2 months, 6 months |
| Immunocompromised (any age) | 3 doses | Same as above |
Children who start the series before their 15th birthday need only two shots. Those who begin later require three, highlighting the advantage of early vaccination. Delaying the vaccine increases the risk of prior HPV exposure, which could limit its effectiveness.
Addressing Common Concerns and Myths
Despite strong scientific support, some parents hesitate due to misconceptions. Addressing these concerns with facts is essential for informed decision-making.
Myth: The vaccine encourages early sexual activity.
Multiple studies have found no link between HPV vaccination and changes in sexual behavior. A large study published in Pediatrics followed over 1,300 girls for three years and found no difference in sexual activity between vaccinated and unvaccinated groups.
Myth: It’s not safe.
The HPV vaccine has undergone rigorous testing and is continuously monitored. Most side effects are mild—such as soreness at the injection site, fever, or dizziness—and serious reactions are extremely rare. Over 135 million doses have been administered in the U.S. with an excellent safety record.
Myth: Only girls need it.
While cervical cancer is the most well-known outcome, HPV also causes cancers in men. Vaccinating both boys and girls reduces overall transmission and protects against oropharyngeal (throat) cancer, which now affects men at higher rates than cervical cancer affects women.
Real-World Impact: A Case Study in Cancer Prevention
In Australia, where a national HPV vaccination program began in 2007 with high coverage (over 80% of adolescents), researchers have observed dramatic results. By 2020, the country reported a 90% drop in genital warts among young people and a significant decline in precancerous cervical lesions. Projections suggest Australia could eliminate cervical cancer within decades, becoming the first country to do so.
This success wasn’t achieved through mandates but through strong public education, school-based vaccination programs, and trust in healthcare providers. It demonstrates that high vaccination rates are possible when families understand the stakes and feel supported in their choices.
What Parents Should Do: A Practical Checklist
To ensure your child receives the full protective benefit of the HPV vaccine, follow this simple action plan:
- Talk to your pediatrician about the HPV vaccine during your child’s 11- or 12-year-old check-up.
- Ask whether your child should receive two or three doses based on age and health status.
- Schedule all doses in advance to avoid missed opportunities.
- Review your state’s school vaccination requirements—some colleges and boarding schools recommend or require HPV vaccination.
- Share accurate information with other parents to combat misinformation.
Frequently Asked Questions
Can the HPV vaccine treat an existing infection?
No, the vaccine prevents future infections but does not treat existing ones. This is why vaccination before exposure is critical.
Is the vaccine necessary if my child isn’t sexually active?
Yes. The goal is to provide protection before potential exposure. Waiting until sexual activity begins may be too late.
Do vaccinated individuals still need cervical cancer screening?
Yes. While the vaccine protects against the most dangerous strains, it doesn’t cover all HPV types. Regular Pap smears remain important for women starting at age 21.
Conclusion: Protecting Future Health Starts Now
The HPV vaccine is one of the most powerful tools available to prevent cancer in both men and women. Though not mandatory in most places, its value is undisputed among medical experts. By vaccinating children at the recommended age, parents can provide long-term protection against diseases that may not appear for decades.
Decisions made today have lasting consequences. Waiting, hesitating, or opting out due to misinformation could mean missing a vital window of prevention. The science is clear: the HPV vaccine is safe, effective, and life-saving.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?