Implantation is a crucial step in early pregnancy—when a fertilized embryo attaches to the uterine lining and begins to grow. When this process fails repeatedly, it can be emotionally and physically taxing for individuals trying to conceive. Implantation failure doesn't always mean infertility, but it does signal that something may be interfering with the body's ability to support early embryonic development. Understanding the underlying causes and knowing what actions to take can significantly improve outcomes.
What Is Implantation Failure?
Implantation failure occurs when a genetically viable embryo does not successfully attach to the endometrium—the inner lining of the uterus—despite being transferred during IVF or naturally conceived. It’s typically diagnosed after multiple failed assisted reproductive technology (ART) cycles or unexplained infertility despite regular ovulation and healthy sperm parameters.
There are two main categories:
- Primary implantation failure: No implantation occurs after several embryo transfers.
- Recurrent implantation failure (RIF): Generally defined as three or more failed IVF cycles with high-quality embryos.
It’s important to note that occasional failure is normal—even under optimal conditions, only about 30–50% of embryos implant successfully. However, repeated failures warrant investigation.
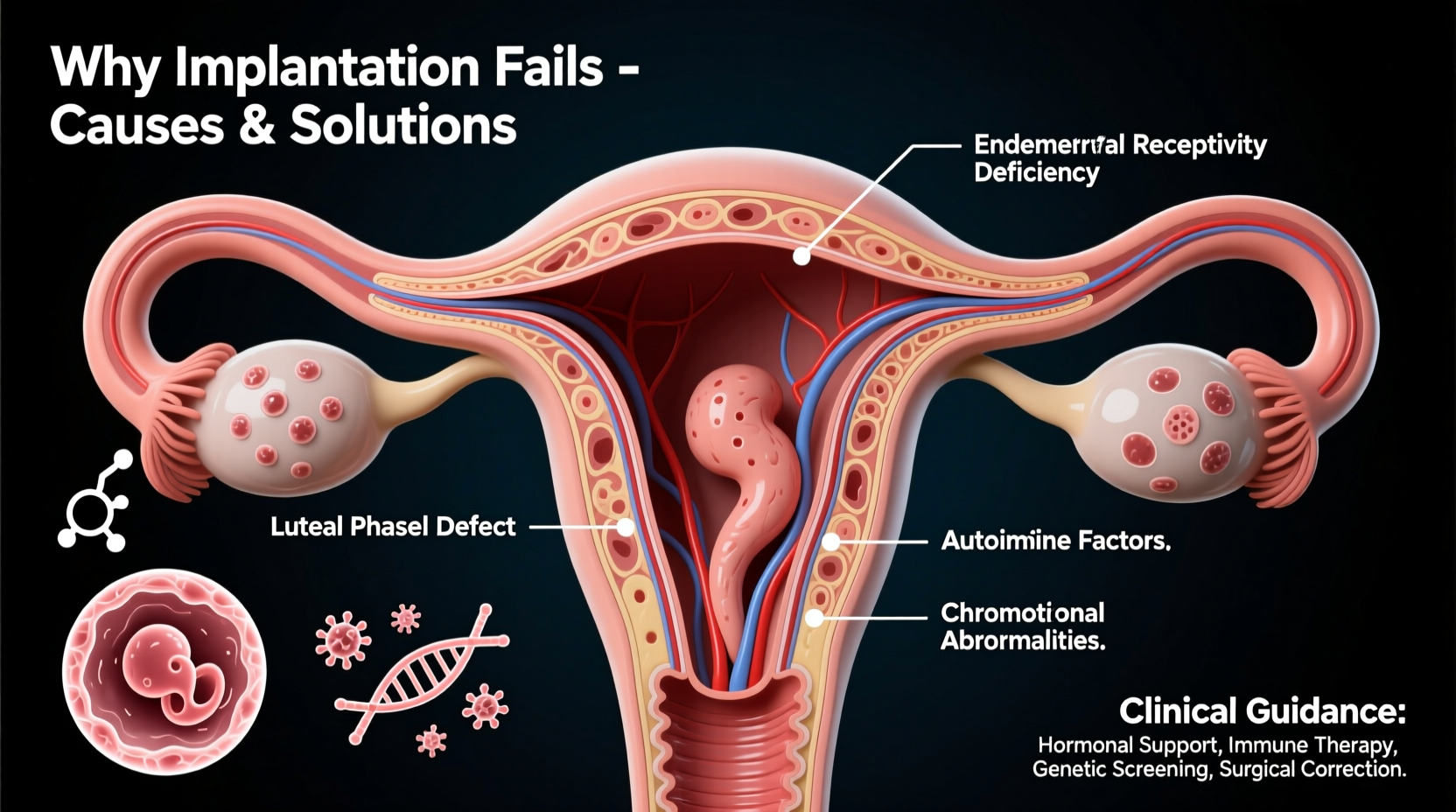
Common Causes of Implantation Failure
Implantation depends on a complex interplay between embryo quality, uterine receptivity, hormonal balance, and immune function. Disruptions in any of these areas can lead to failure.
1. Embryo Quality and Chromosomal Abnormalities
The most frequent cause of implantation failure is poor embryo quality, often due to chromosomal abnormalities (aneuploidy). These errors increase with maternal age and can prevent proper development even if fertilization occurs.
“Over 60% of early miscarriages and implantation failures are linked to embryonic chromosomal anomalies.” — Dr. Sarah Lin, Reproductive Endocrinologist
2. Uterine Receptivity Issues
The window for implantation—called the “window of implantation” (WOI)—is narrow, usually lasting just 1–2 days per cycle. If the endometrium isn’t receptive during this time, implantation won’t occur.
Conditions affecting receptivity include:
- Endometrial polyps or fibroids
- Asherman’s syndrome (intrauterine adhesions)
- Chronic endometritis (low-grade uterine infection)
- Thin endometrial lining (<7mm)
3. Hormonal Imbalances
Progesterone is essential for preparing and maintaining the endometrial lining. Insufficient progesterone production or resistance can impair implantation. Other imbalances involving thyroid hormones or elevated prolactin levels also play a role.
4. Immune System Dysregulation
In some cases, the immune system may mistakenly attack the embryo, treating it as a foreign invader. Autoimmune disorders like antiphospholipid syndrome (APS) or abnormal natural killer (NK) cell activity have been associated with recurrent failure.
5. Thrombophilias and Blood Flow Issues
Clotting disorders such as factor V Leiden or protein S deficiency can restrict blood flow to the uterus, reducing oxygen and nutrient delivery necessary for implantation.
6. Lifestyle and Environmental Factors
Smoking, excessive alcohol consumption, obesity, stress, and exposure to endocrine-disrupting chemicals (like BPA) can all negatively influence both egg and embryo quality as well as uterine health.
Diagnostic Approaches After Recurrent Failure
If you’ve experienced repeated implantation failure, a comprehensive evaluation is essential. Your fertility specialist may recommend the following tests:
| Test | Purpose | When Recommended |
|---|---|---|
| Karyotyping (both partners) | Detect chromosomal translocations or abnormalities | After 2+ failed cycles |
| Endometrial Receptivity Array (ERA) | Identify personalized window of implantation | Repeated unexplained failures |
| Hysteroscopy | Visualize and treat structural issues (polyps, adhesions) | Suspected anatomical problems |
| Thrombophilia panel | Check for inherited clotting disorders | History of miscarriage or thin lining |
| Autoimmune screening (APA, ANA) | Rule out immune-mediated rejection | Unexplained RIF |
| Preimplantation Genetic Testing for Aneuploidy (PGT-A) | Select chromosomally normal embryos | Advanced maternal age or prior aneuploid embryos |
Action Plan: What You Can Do to Improve Success
While not every cause of implantation failure can be corrected, many factors are modifiable. Here’s a practical roadmap to enhance your chances:
Step-by-Step Guide to Addressing Implantation Failure
- Comprehensive Medical Review: Schedule a consultation with a reproductive immunologist or fertility specialist experienced in RIF.
- Optimize Embryo Quality: Consider PGT-A testing to select euploid embryos for transfer, especially if over 35.
- Assess Uterine Health: Undergo hysteroscopy or saline sonogram to rule out polyps, fibroids, or scar tissue.
- Test Hormone Levels: Check progesterone, TSH, prolactin, and AMH mid-luteal phase and adjust treatment accordingly.
- Evaluate Immune & Clotting Factors: Screen for APS, NK cells, and inherited thrombophilias if indicated.
- Personalize Transfer Timing: Use ERA or similar tests to identify your unique implantation window.
- Adopt Fertility-Supportive Habits: Focus on nutrition, sleep, stress reduction, and avoiding toxins.
Mini Case Study: Overcoming Recurrent Failure
Lena, 38, had four unsuccessful IVF cycles using her own eggs. All embryos were graded as good quality, yet none implanted. Her initial workup showed normal tubes and ovaries, but further testing revealed:
- Positive antiphospholipid antibodies
- Thin endometrial lining (5mm) despite estrogen support
- Mild chronic endometritis
After treatment with low-dose aspirin, heparin injections, antibiotics, and a tailored hormone protocol, Lena underwent another cycle. This time, with immune modulation and optimized endometrial preparation, she achieved a successful pregnancy and gave birth to a healthy baby boy.
Frequently Asked Questions
Can stress cause implantation failure?
While acute stress alone is unlikely to block implantation, chronic stress can disrupt hormonal balance and affect immune regulation. High cortisol levels may interfere with progesterone signaling and reduce uterine blood flow. Managing stress through mindfulness, yoga, or therapy can support overall reproductive health.
Is it possible to have implantation failure with donor eggs?
Yes. Even with high-quality donor eggs, implantation can fail due to uterine factors, immune responses, or undiagnosed medical conditions. The recipient’s endometrial environment plays a critical role regardless of embryo origin.
How long should I wait after a failed transfer before trying again?
Most specialists recommend waiting one full menstrual cycle to allow the body to recover hormonally and emotionally. Some protocols require longer breaks, especially if surgical procedures or infections were involved.
Conclusion: Moving Forward with Confidence
Implantation failure is not the end of your journey to parenthood—it’s often a signpost pointing toward underlying issues that can be addressed. With advances in reproductive medicine, personalized diagnostics, and targeted treatments, many patients go on to achieve successful pregnancies after multiple setbacks.
The key lies in persistence, informed decision-making, and working with a care team that listens and investigates thoroughly. Don’t hesitate to seek second opinions or explore integrative approaches alongside conventional treatment.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?