Experiencing light bleeding or spotting after your period ends is more common than many realize. While it’s often harmless and linked to natural hormonal shifts, persistent or unusual bleeding can signal an underlying condition that requires medical attention. Understanding the difference between normal post-period spotting and a symptom that warrants concern empowers you to make informed decisions about your reproductive health.
This article explores the most frequent causes of light bleeding after menstruation, identifies red flags, and provides actionable guidance on when to consult a healthcare provider.
Common Causes of Post-Period Spotting
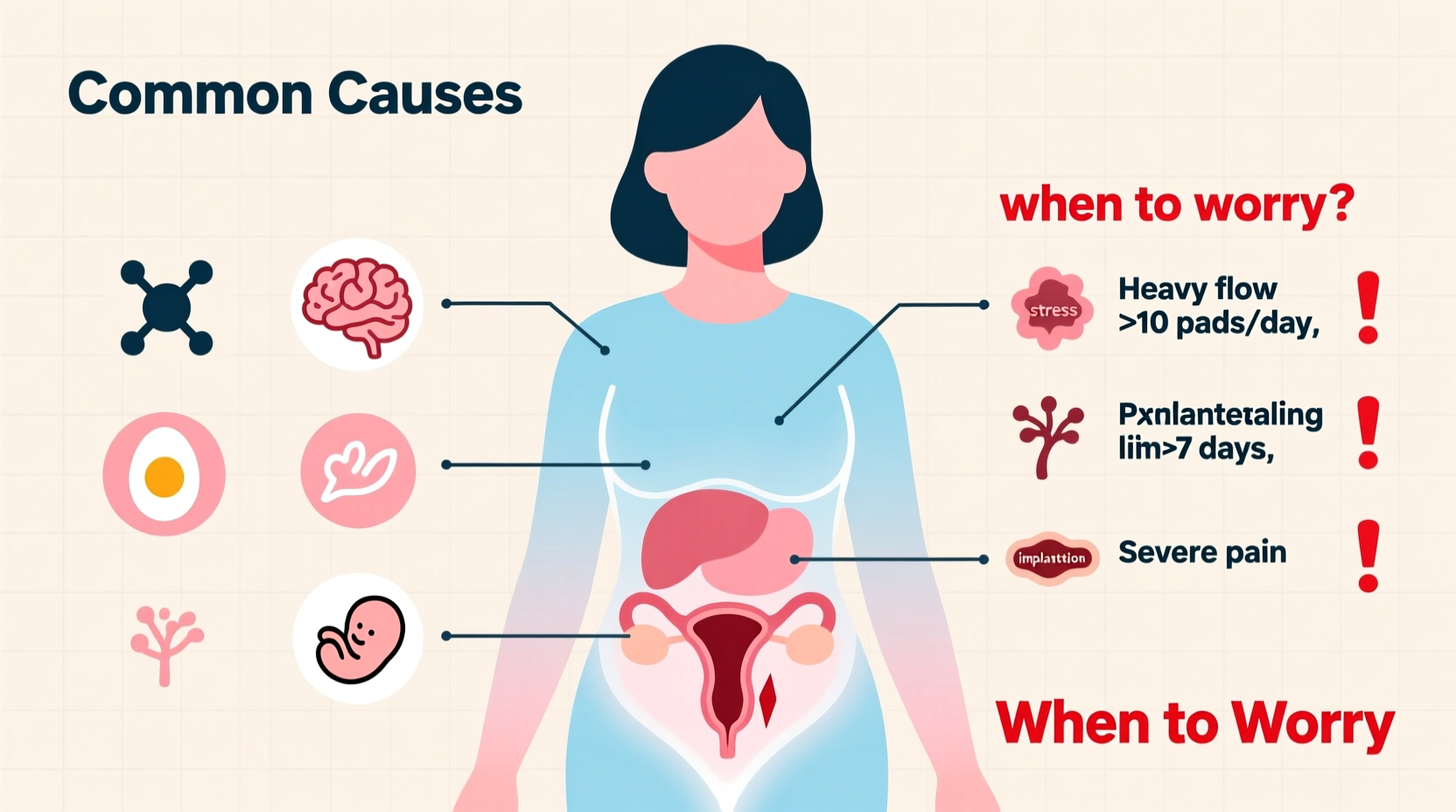
Spotting in the days following your period can stem from various physiological and lifestyle-related factors. Most are benign and resolve on their own.
- Ovulation spotting: Around mid-cycle, some women experience light pink or brown discharge due to a brief drop in estrogen levels when the egg is released. This typically lasts 1–2 days.
- Hormonal fluctuations: Natural changes in estrogen and progesterone can cause the uterine lining to shed slightly outside of your regular cycle.
- Birth control use: Especially during the first few months of starting oral contraceptives, patches, or hormonal IUDs, irregular bleeding is common as the body adjusts.
- Cervical irritation: Sexual intercourse, gynecological exams, or even tampon use can cause minor trauma to the cervix, leading to light bleeding.
- Stress or significant weight changes: Both can disrupt your hormonal balance and menstrual cycle, potentially causing unexpected spotting.
When Light Bleeding May Signal a Health Concern
While occasional spotting is usually not alarming, certain signs suggest the need for further evaluation. Persistent or symptomatic bleeding should never be ignored.
“Post-menstrual bleeding that lasts longer than three days, occurs frequently, or is accompanied by pain or odor should prompt a visit to a gynecologist.” — Dr. Lena Patel, OB-GYN Specialist
Conditions associated with abnormal post-period bleeding include:
- Polyps or fibroids: Non-cancerous growths in the uterus or cervix can cause irregular bleeding, including after your period.
- Endometriosis: Tissue similar to the uterine lining grows outside the uterus, often causing pelvic pain and unpredictable bleeding.
- Adenomyosis: The endometrial tissue grows into the muscular wall of the uterus, leading to heavy periods and spotting.
- Infections: Pelvic inflammatory disease (PID) or sexually transmitted infections like chlamydia or gonorrhea may present with intermenstrual bleeding and discharge.
- Thyroid disorders: Both hypothyroidism and hyperthyroidism can disrupt menstrual regularity.
- Perimenopause: As women approach menopause, cycles become irregular, and spotting between periods becomes more common.
Do’s and Don’ts: Managing Post-Period Spotting
| Do’s | Don’ts |
|---|---|
| Track your symptoms and cycle length | Ignore bleeding that lasts more than 3 days |
| Maintain a healthy weight and manage stress | Assume all spotting is normal without evaluation |
| Use panty liners instead of tampons during spotting | Engage in unprotected sex if infection is suspected |
| Schedule routine gynecological check-ups | Self-diagnose based on internet research |
| Stay hydrated and eat a balanced diet rich in iron | Stop birth control abruptly without medical advice |
Mini Case Study: When Spotting Was a Warning Sign
Sarah, a 34-year-old teacher, noticed light brown spotting about five days after her period ended. At first, she dismissed it as stress-related since she had recently changed jobs. However, the spotting recurred every cycle for three months and began to be accompanied by mild pelvic discomfort.
After tracking her symptoms and consulting her gynecologist, an ultrasound revealed a small endometrial polyp. It was removed during a simple outpatient procedure, and her post-period bleeding stopped completely within the next cycle. Sarah’s case highlights how consistent tracking and timely medical consultation can prevent complications.
Step-by-Step Guide: What to Do If You Experience Post-Period Bleeding
- Observe the pattern: Note how often spotting occurs, its color (pink, brown, red), duration, and any associated symptoms like cramping or fatigue.
- Review recent changes: Consider new medications, birth control, sexual activity, or lifestyle shifts that might influence your cycle.
- Start a symptom journal: Record dates, flow intensity, and triggers. Apps like Clue or Flo can help visualize trends.
- Rule out pregnancy: Take a home pregnancy test, especially if you’re sexually active—even light bleeding can occur with early pregnancy or implantation.
- Schedule a gynecological exam: If spotting persists beyond two or three cycles, or if you have pain, fever, or foul-smelling discharge, see your doctor promptly.
- Undergo recommended tests: These may include a pelvic exam, Pap smear, STI screening, ultrasound, or blood work to check hormone or thyroid levels.
Frequently Asked Questions
Is it normal to bleed a week after my period ends?
Occasional light spotting around ovulation (about 7–10 days after your period) is normal for some women. However, regular or heavy bleeding at this time should be evaluated by a healthcare provider.
Can stress really cause post-period bleeding?
Yes. Chronic stress affects the hypothalamus, which regulates hormones that control your menstrual cycle. This disruption can lead to irregular bleeding, including spotting after your period.
Should I be worried about cancer if I have post-period spotting?
While rare, post-menopausal bleeding is a known warning sign of endometrial cancer. In premenopausal women, cancer is much less likely, but persistent unexplained bleeding still requires investigation to rule out precancerous changes or other conditions.
Action Plan: Stay Proactive About Your Cycle Health
Your menstrual cycle is a vital sign of overall health. Light bleeding after your period doesn’t always indicate a problem, but it shouldn’t be automatically dismissed either. Pay attention to your body’s signals, document changes, and seek clarity when something feels off.
Early detection of conditions like fibroids, infections, or hormonal imbalances leads to better outcomes and less invasive treatments. Don’t hesitate to advocate for your health—even seemingly minor symptoms deserve professional insight.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?