Bowel movements are a window into digestive health. While most people focus on frequency or consistency, the color of your stool can reveal important clues about your internal systems—especially your liver, gallbladder, and pancreas. Light tan poop is not always alarming, but it’s never typical. Unlike the familiar medium to dark brown shades resulting from bile breakdown, pale or clay-colored stools suggest a disruption in bile flow. Understanding why this happens—and when it matters—is essential for catching potential issues early.
Why Stool Is Usually Brown
The characteristic brown color of healthy stool comes from bilirubin, a pigment formed during the breakdown of red blood cells. This substance travels to the liver, where it’s processed into bile. Bile is stored in the gallbladder and released into the small intestine during digestion to help break down fats. As bacteria in the colon act on bile, bilirubin transforms into urobilin, which gives feces its brown hue.
When bile production or delivery is impaired, that transformation doesn’t occur properly, leading to lighter-colored stools. A light tan, clay, or grayish appearance often indicates reduced or blocked bile flow—a condition known as cholestasis.
Common Causes of Light Tan Poop
Several factors can interfere with bile secretion or intestinal processing. Some are temporary and benign; others point to underlying disease.
- Gallstones: One of the most frequent causes. Stones in the gallbladder or bile ducts can block bile from reaching the intestines, especially after fatty meals. This may lead to intermittent pale stools accompanied by right upper abdominal pain.
- Liver conditions: Hepatitis (viral, alcoholic, or autoimmune), cirrhosis, or fatty liver disease can impair bile production. In these cases, stool discoloration often appears alongside fatigue, jaundice, or elevated liver enzymes.
- Pancreatic disorders: Chronic pancreatitis or pancreatic cancer may obstruct the bile duct indirectly. These conditions typically present with additional symptoms like weight loss, back pain, or greasy, foul-smelling stools (steatorrhea).
- Medications: Certain drugs—including antacids containing aluminum hydroxide, some antibiotics, and anti-diarrheal agents like bismuth subsalicylate—can temporarily alter stool color.
- Dietary factors: Rapid transit through the gut due to diarrhea may limit bacterial interaction with bile, resulting in paler-than-normal stools. High intake of white foods (rice, bread, dairy) without fiber can also contribute transiently.
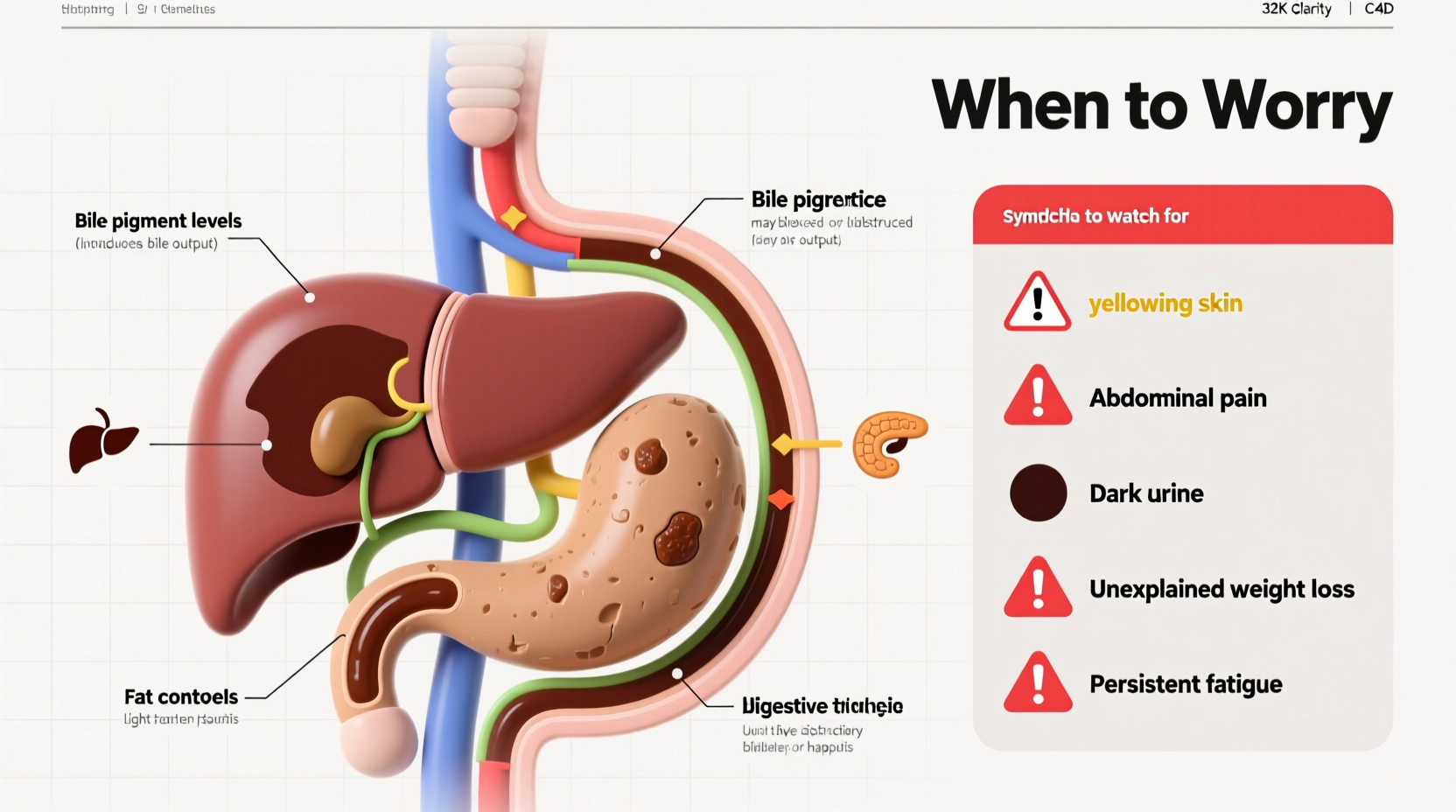
When to Be Concerned: Red Flags
Occasional variation in stool color is normal. However, consistently light tan, clay-colored, or ash-gray poop should prompt closer attention, particularly if paired with other symptoms. The presence of certain warning signs increases the urgency for medical evaluation.
“Persistent pale stools are one of the earliest clinical indicators of biliary obstruction. I always ask patients about stool color when assessing liver enzyme abnormalities.” — Dr. Alan Reeves, Gastroenterologist, Cleveland Clinic Digestive Institute
| Symptom | What It Might Indicate | Urgency Level |
|---|---|---|
| Jaundice (yellow skin/eyes) | Liver dysfunction or bile duct blockage | High – Seek care within 24–48 hours |
| Dark urine | Bilirubin buildup in blood | Moderate to high |
| Abdominal pain (right upper quadrant) | Gallstones or inflammation | Moderate – Evaluate soon |
| Unintended weight loss | Potential malignancy or malabsorption | High – Requires investigation |
| Fever or chills | Infection such as cholangitis | Emergency – Go to ER |
Diagnostic Process and What to Expect
If you report light tan stools to a healthcare provider, expect a systematic approach to rule out serious causes. Diagnosis usually begins with a detailed history and physical exam, followed by targeted testing.
- Medical History: Your doctor will ask about recent illnesses, medications, alcohol use, family history of liver disease, and associated symptoms.
- Blood Tests: Liver function tests (LFTs) check levels of enzymes like ALT, AST, ALP, and bilirubin. Elevated alkaline phosphatase and direct bilirubin suggest bile duct issues.
- Imaging: Abdominal ultrasound is often first-line to detect gallstones or bile duct dilation. MRCP (Magnetic Resonance Cholangiopancreatography) provides detailed images of ducts without radiation.
- Endoscopic Evaluation: ERCP (Endoscopic Retrograde Cholangiopancreatography) may be used both to diagnose and treat obstructions, such as removing stones or placing stents.
- Stool Analysis: In cases of suspected malabsorption, a fecal fat test may be ordered.
Mini Case Study: Recognizing Early Signs
Julia, a 54-year-old teacher, noticed her stool had turned pale over three weeks. She initially dismissed it as a side effect of a new probiotic. But when she developed yellowing eyes and itching across her arms, she scheduled a visit. Blood work revealed elevated bilirubin and ALP. An ultrasound showed a stone lodged in her common bile duct. After an ERCP removed the blockage, her stool returned to normal within days. Julia’s case illustrates how seemingly minor changes—when persistent—can signal significant pathology.
Prevention and Daily Habits That Support Bile Flow
While not all causes of light tan poop are preventable, supporting liver and gallbladder health reduces risk. Simple lifestyle adjustments can make a meaningful difference.
Checklist: Promote Healthy Digestion and Bile Secretion
- Eat balanced meals with healthy fats (e.g., olive oil, avocado) to trigger bile release
- Maintain a healthy weight—rapid weight loss increases gallstone risk
- Limits alcohol consumption to protect liver cells
- Avoid skipping meals, which can stagnate bile in the gallbladder
- Exercise regularly to improve metabolic and liver function
- Review medications with your doctor for potential liver impact
Frequently Asked Questions
Can light tan poop be caused by something I ate?
Yes, but only indirectly. No food directly turns stool tan. However, a diet very low in fiber and high in refined carbohydrates may speed up transit time, reducing bile breakdown. Additionally, excessive dairy or antacid use might contribute to paler stools. True clay-colored stools, however, are rarely diet-related and warrant further investigation.
Is light tan poop dangerous in children?
In infants, stool color varies widely, especially in the first months. However, persistent pale stools in babies—particularly with poor weight gain or jaundice—can indicate biliary atresia, a rare but serious condition requiring surgery. Pediatricians routinely screen for this during well-baby visits. In older children, causes resemble adult patterns, including viral hepatitis or medication effects.
How long does it take for stool color to return to normal?
If the cause is temporary—like a short course of antibiotics or mild gastroenteritis—stool color may normalize within a few days after recovery. With resolved gallstones or treated infections, improvement can occur within 1–2 weeks. Chronic conditions like cirrhosis may result in ongoing variations, managed through treatment of the underlying disease.
Conclusion: Listen to Your Body
Stool color is a subtle yet powerful indicator of internal health. Light tan poop isn't an emergency every time, but it should never be ignored when it persists. Unlike fleeting digestive upsets, changes in pigmentation reflect deeper physiological processes—often involving the liver or biliary system. Catching issues early, such as gallstones or liver inflammation, can prevent complications like infection, chronic damage, or even cancer.
You don’t need to panic at the sight of one odd-colored bowel movement. But if pale stools become routine—or come with other symptoms—take action. Talk to your doctor, request appropriate tests, and advocate for your digestive wellness. Your body sends signals for a reason. Learning to interpret them could make all the difference.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?