Sudden, sharp pain radiating through the pelvic region—often described as a “lightning bolt” sensation—is commonly associated with pregnancy. However, many people who are not pregnant experience this same jolt, leaving them confused and concerned. While occasional pelvic discomfort can be normal, recurring or intense \"lightning crotch\" episodes outside of pregnancy may signal underlying conditions that require attention. Understanding the potential causes, symptoms, and appropriate responses is essential for managing pelvic health effectively.
What Is Lightning Crotch?
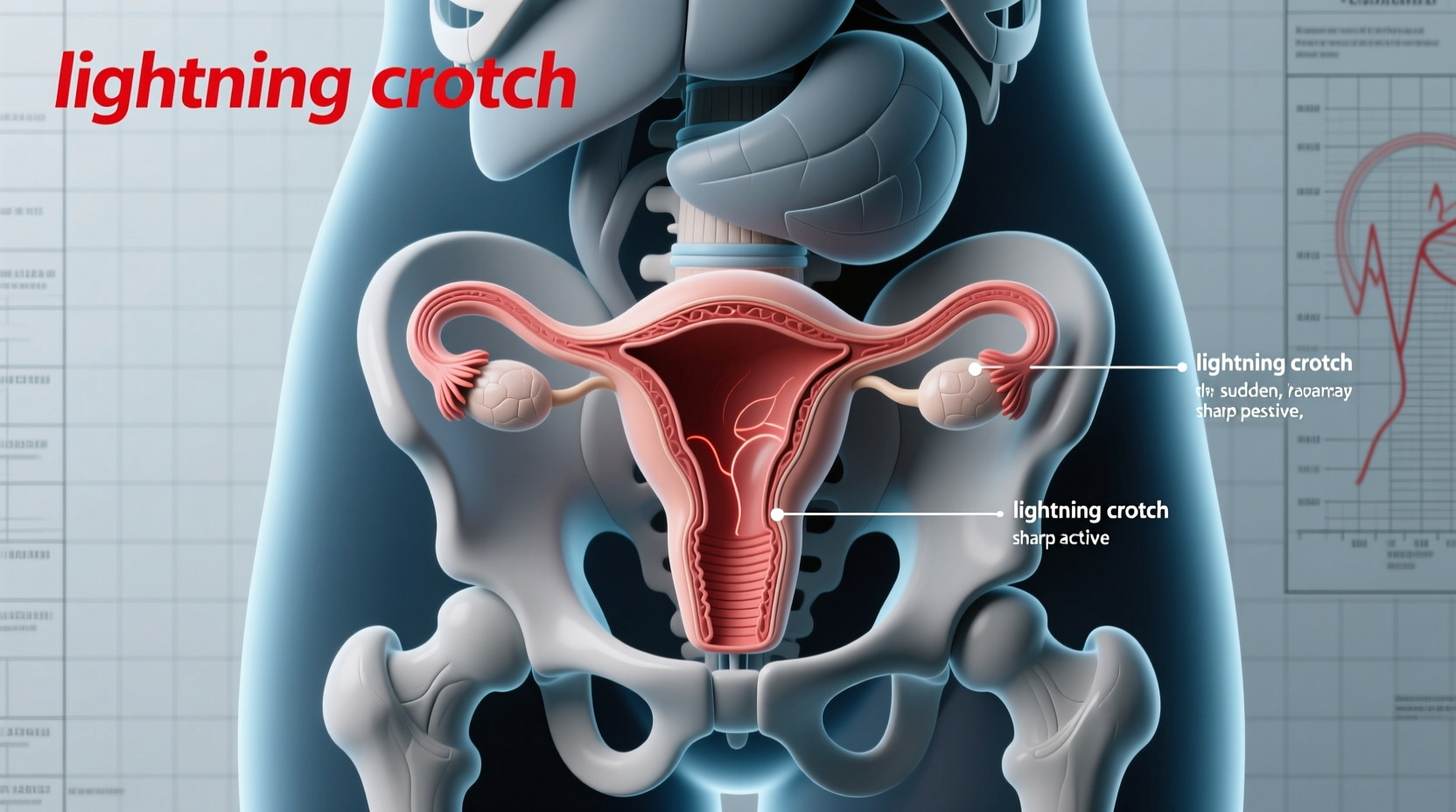
The term “lightning crotch” refers to a sudden, electric-like shock of pain that shoots through the lower abdomen, groin, or perineum. It typically lasts only a few seconds but can be severe enough to cause momentary immobility. Though widely discussed in prenatal communities, this phenomenon is not exclusive to pregnancy. In non-pregnant individuals, it often indicates nerve irritation, muscular strain, or urogenital system involvement.
Unlike general pelvic aches, lightning crotch is characterized by its sharp, shooting quality and unpredictable onset. It may occur during movement, at rest, or even during sleep, making it both disruptive and alarming.
Common Causes in Non-Pregnant Individuals
Several physiological and neurological factors can trigger lightning crotch sensations in those not expecting. The most frequent causes include:
- Pudendal Neuralgia: Compression or irritation of the pudendal nerve, which supplies sensation to the pelvic floor, genitals, and anus. This condition often results from prolonged sitting, cycling, trauma, or pelvic surgery.
- Pelvic Floor Dysfunction: Overactive or imbalanced pelvic floor muscles can compress nerves or refer pain along nerve pathways, mimicking electric shocks.
- Sciatica: Irritation of the sciatic nerve can radiate pain into the lower abdomen and groin, especially if lumbar spine issues are present.
- Urinary Tract Infections (UTIs): Severe or chronic UTIs may cause referred nerve pain or bladder spasms that feel like sharp jolts.
- Endometriosis: When endometrial-like tissue grows outside the uterus, it can infiltrate nerves such as the lumbosacral plexus, leading to neuropathic pain episodes.
- Ovarian Cysts or Torsion: Large cysts or sudden twisting of the ovary can stretch surrounding tissues and nerves, producing acute, stabbing pain.
- Musculoskeletal Strain: Sudden movements, heavy lifting, or athletic activity can strain pelvic ligaments or pubic symphysis, triggering sharp pain.
“Neuropathic pelvic pain is underdiagnosed. Patients describing 'electric' or 'shooting' pain should be evaluated for nerve entrapment syndromes, especially pudendal neuralgia.” — Dr. Lena Torres, Pelvic Pain Specialist, Cleveland Clinic
When to Seek Medical Evaluation
While isolated incidents of lightning crotch may resolve on their own, certain red flags warrant prompt medical assessment:
Warning Signs Requiring Immediate Attention
- Pain that increases in frequency or intensity over time
- Loss of bladder or bowel control
- Numbness or tingling in the saddle area (perineum, inner thighs)
- Fever accompanied by pelvic pain (possible infection)
- Pain localized to one side with nausea or vomiting (possible ovarian torsion)
If any of these symptoms occur, consult a healthcare provider immediately. Conditions like cauda equina syndrome or ovarian torsion are medical emergencies requiring urgent intervention.
Diagnostic Process and Treatment Options
Diagnosing the root cause of non-pregnancy-related lightning crotch involves a multidisciplinary approach. A primary care physician may refer patients to gynecologists, neurologists, urologists, or pelvic floor physical therapists based on initial findings.
Common Diagnostic Tools
| Test | Purpose | Conditions Identified |
|---|---|---|
| Pelvic Ultrasound | Visualize reproductive organs | Ovarian cysts, fibroids, endometriosis |
| MRI of Lumbar Spine/Pelvis | Detect nerve compression or soft tissue abnormalities | Sciatica, pudendal nerve entrapment, deep infiltrating endometriosis |
| Urine Analysis/Culture | Check for infection | UTI, interstitial cystitis |
| Pelvic Floor EMG | Assess muscle coordination and nerve function | Pelvic floor dysfunction, neuromuscular imbalance |
Treatment depends on the underlying diagnosis:
- Physical Therapy: Specialized pelvic floor therapy can release tight muscles, improve coordination, and reduce nerve compression.
- Medications: Neuropathic pain agents like gabapentin or pregabalin may help manage nerve-related pain. Hormonal therapies are used for endometriosis.
- Injections: Pudendal nerve blocks can provide diagnostic clarity and temporary relief.
- Surgery: Reserved for cases like large cysts, severe endometriosis, or confirmed nerve decompression needs.
Real-Life Example: Sarah’s Experience
Sarah, a 34-year-old office worker, began experiencing sharp, electric pains in her left groin after starting a new job that required long hours at a desk. Initially dismissing it as muscle strain, she noticed the pain worsened after cycling on weekends. Over three months, the episodes became more frequent—sometimes occurring multiple times a day—and were accompanied by numbness in her inner thigh.
After seeing a gynecologist and receiving a normal ultrasound, she was referred to a pelvic pain specialist. An MRI revealed mild pudendal nerve compression. With targeted physical therapy, ergonomic adjustments at work, and temporary use of gabapentin, Sarah reduced her pain significantly within eight weeks. Her case highlights the importance of looking beyond gynecological causes and considering nerve and musculoskeletal factors.
Practical Tips for Managing Symptoms
- Practice gentle stretching routines focusing on hip flexors, piriformis, and pelvic floor.
- Stay hydrated and maintain regular bowel habits to minimize pelvic nerve irritation.
- Wear supportive, non-restrictive clothing—tight underwear or jeans can exacerbate nerve pressure.
- Apply heat to the lower abdomen or back to relax tense muscles and improve blood flow.
Step-by-Step Guide to Addressing Lightning Crotch
- Track Symptoms: Record when pain occurs, its duration, and possible triggers.
- Consult a Doctor: Begin with a primary care provider or gynecologist.
- Rule Out Urgent Causes: Ensure no infections, cysts, or neurological emergencies are present.
- Seek Specialty Care: If initial tests are inconclusive, consider a pelvic pain clinic or neurologist.
- Start Conservative Treatment: Begin with physical therapy and lifestyle modifications.
- Reevaluate Progress: After 6–8 weeks, assess improvement and adjust treatment as needed.
Frequently Asked Questions
Can men experience lightning crotch?
Yes. Though less commonly reported, men can experience similar nerve-related pelvic pain due to pudendal neuralgia, prostatitis, or sciatica. The sensation may radiate to the testicles, perineum, or inner thighs.
Is lightning crotch a sign of cancer?
Rarely. While persistent pelvic pain should always be evaluated, lightning crotch is not typically a direct symptom of cancer. However, tumors in the pelvis or spine could compress nerves and cause similar pain—making thorough evaluation important.
Can stress cause lightning crotch?
Indirectly, yes. Chronic stress contributes to muscle tension, particularly in the pelvic floor, which can irritate nerves and trigger pain episodes. Stress management techniques like mindfulness or biofeedback may help reduce flare-ups.
Final Thoughts and Call to Action
Experiencing lightning crotch when not pregnant can be unsettling, but it's not uncommon—and most causes are treatable with proper care. Ignoring persistent symptoms may lead to chronic pain or delayed diagnosis of manageable conditions. By understanding potential causes, recognizing warning signs, and seeking timely evaluation, you can take control of your pelvic health.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?