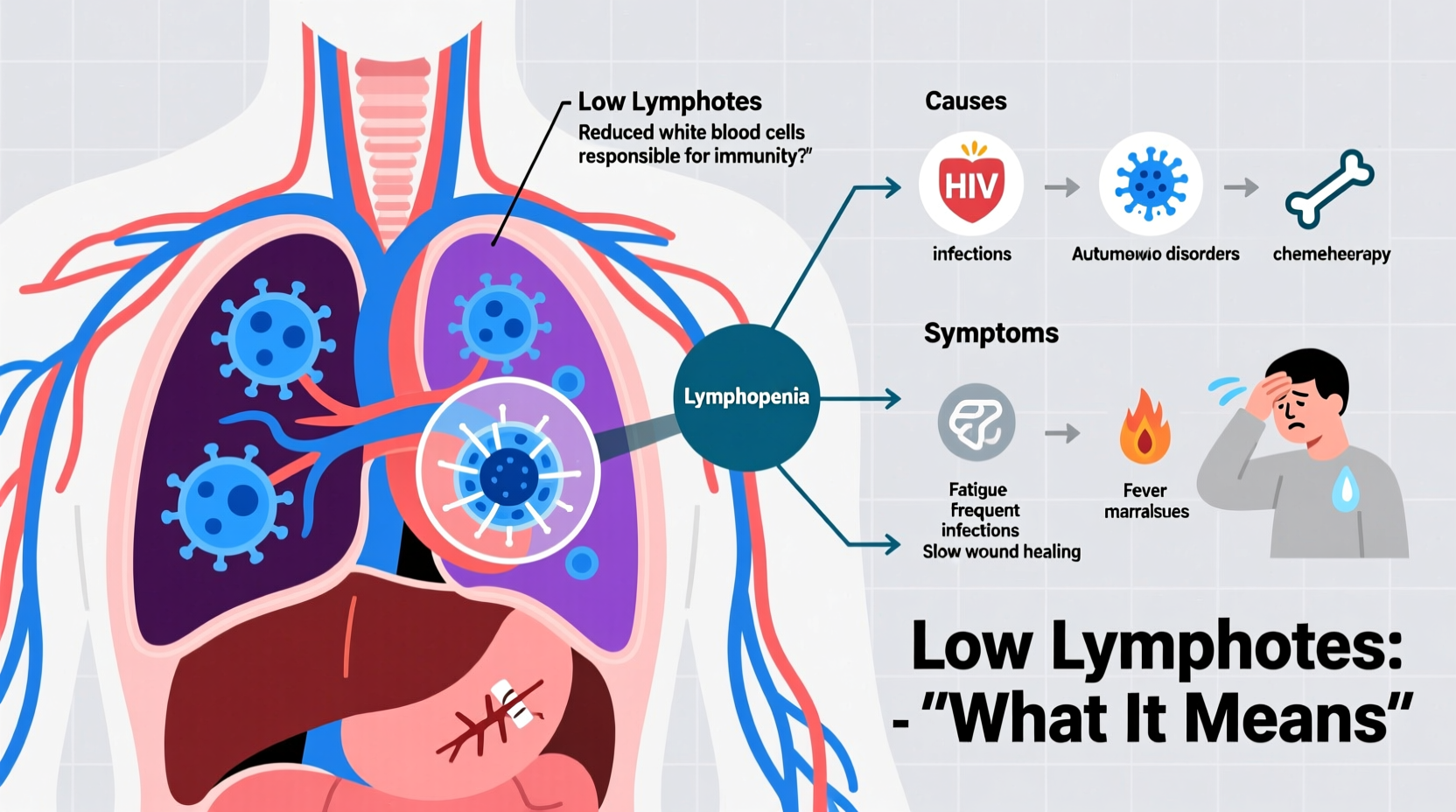
Lymphocytes are a type of white blood cell crucial to your body’s defense system. They include B cells, T cells, and natural killer (NK) cells, each playing distinct roles in identifying and destroying pathogens like viruses, bacteria, and abnormal cells. When a blood test reveals low lymphocyte levels—a condition known as lymphocytopenia—it can signal an underlying health issue affecting your immune function. While occasional fluctuations are normal, persistently low counts may increase susceptibility to infections and warrant medical evaluation.
What Are Lymphocytes and Why Do They Matter?
Lymphocytes form the backbone of adaptive immunity. B cells produce antibodies that target specific invaders, while T cells either coordinate immune responses or directly attack infected cells. NK cells act as rapid responders to viral infections and cancerous cells. A healthy adult typically has between 1,000 and 4,800 lymphocytes per microliter of blood. Values below this range are classified as low, though exact thresholds vary slightly by lab.
Because these cells are central to immune surveillance, their deficiency can compromise the body's ability to respond effectively to threats. This doesn’t always cause immediate symptoms but may manifest through recurrent or severe infections over time.
Common Causes of Low Lymphocytes
Lymphocytopenia arises from diverse factors, ranging from temporary stressors to chronic diseases. Understanding potential causes helps contextualize results and guides further investigation.
- Infections: Acute viral infections like influenza, hepatitis, or HIV can temporarily suppress lymphocyte production. HIV specifically targets CD4+ T cells, leading to progressive decline.
- Autoimmune Disorders: Conditions such as lupus or rheumatoid arthritis may trigger immune-mediated destruction of lymphocytes.
- Nutritional Deficiencies: Severe lack of protein, zinc, or vitamins like B12 and folate impairs immune cell synthesis.
- Chronic Diseases: Kidney failure, liver cirrhosis, and certain cancers—especially those involving bone marrow—can disrupt lymphocyte generation.
- Medications: Chemotherapy, corticosteroids, and immunosuppressants used post-transplant or for autoimmune conditions often reduce lymphocyte counts.
- Stress and Trauma: Physical stress from surgery, burns, or intense psychological strain can transiently lower levels via hormonal shifts.
- Genetic Conditions: Rare disorders like DiGeorge syndrome impair lymphocyte development from birth.
“Lymphopenia isn't a diagnosis itself—it's a clue. The key is uncovering why the numbers are down.” — Dr. Alan Reyes, Hematologist & Immunology Specialist
Symptoms and What They Indicate
Low lymphocytes often go unnoticed until complications arise. Unlike conditions with overt warning signs, lymphocytopenia typically presents indirectly. Key indicators include:
- Frequent infections (e.g., sinusitis, bronchitis, pneumonia)
- Slow healing of wounds or persistent cold sores
- Unexplained fevers or fatigue
- Swollen lymph nodes (in some cases, despite low circulating cells)
- Opportunistic infections in severe cases (e.g., fungal esophagitis, pneumocystis pneumonia)
The absence of symptoms doesn’t rule out concern, especially if risk factors like long-term steroid use or chemotherapy are present. Conversely, mild reductions may resolve spontaneously after illness recovery.
When to Be Concerned
A single low reading isn’t necessarily alarming. However, consistent low counts across multiple CBC tests, especially below 1,000/μL, merit deeper assessment. Levels under 500/μL significantly increase infection risk and require prompt follow-up.
| Lymphocyte Count (per μL) | Interpretation | Action Recommended |
|---|---|---|
| 1,000 – 4,800 | Normal range | No action needed |
| 500 – 1,000 | Mild lymphopenia | Monitor; evaluate lifestyle and medications |
| 200 – 500 | Moderate deficiency | Medical workup advised |
| Below 200 | Severe lymphopenia | Urgent evaluation required |
Diagnostic Process and Next Steps
If your CBC shows low lymphocytes, your physician will likely recommend additional tests to determine the root cause. These may include:
- Differential count: Breakdown of T cells, B cells, and NK cells to identify which subset is affected.
- HIV testing: Essential given its direct impact on CD4+ lymphocytes.
- Autoimmune panels: To check for lupus, rheumatoid arthritis, or other connective tissue diseases.
- Nutritional markers: Serum levels of vitamin B12, folate, zinc, and albumin.
- Bone marrow biopsy: In rare cases where production defects are suspected.
Imaging studies or referrals to specialists—such as immunologists or hematologists—are common next steps depending on initial findings.
Mini Case Study: Recognizing Hidden Immune Dysfunction
Sarah, a 42-year-old teacher, visited her primary care provider after enduring four respiratory infections within six months. Each required antibiotics, and recovery took longer than usual. Her CBC revealed a lymphocyte count of 780/μL. Further testing uncovered undiagnosed lupus, confirmed through positive ANA and anti-dsDNA antibodies. With proper treatment using hydroxychloroquine and immune modulation, her lymphocyte levels gradually normalized over nine months, and infection frequency dropped significantly.
This case illustrates how recurrent illness can be the first sign of immune imbalance—and how timely diagnosis transforms outcomes.
Managing and Supporting Immune Health
Treatment depends entirely on the underlying cause. There is no universal fix for low lymphocytes, but supportive strategies can strengthen resilience.
Do’s and Don’ts for Immune Support
| Do | Don't |
|---|---|
| Eat a balanced diet rich in lean protein, fruits, vegetables, and whole grains | Skip meals or rely on processed foods lacking nutrients |
| Practice good hygiene—handwashing, avoiding sick contacts | Ignore vaccination schedules (e.g., flu, pneumococcal) |
| Get 7–8 hours of quality sleep nightly | Smoke or consume excessive alcohol |
| Follow prescribed treatments for chronic conditions | Self-medicate with supplements without medical advice |
Checklist: Actions to Take After a Low Lymphocyte Diagnosis
- ✔️ Review all current medications with your doctor
- ✔️ Schedule follow-up CBC in 4–6 weeks to monitor trends
- ✔️ Request targeted tests based on symptoms (e.g., HIV, autoimmune markers)
- ✔️ Assess dietary intake and consider nutritional screening
- ✔️ Minimize exposure to infectious environments (e.g., crowded spaces during flu season)
- ✔️ Discuss vaccination status, including annual flu and updated COVID-19 boosters
Frequently Asked Questions
Can stress cause low lymphocytes?
Yes. Chronic physical or emotional stress elevates cortisol, which suppresses lymphocyte production and function. Short-term stress may cause temporary drops, but levels usually rebound once the stressor resolves.
Is low lymphocyte count dangerous?
It depends on severity and duration. Mild, transient decreases pose minimal risk. However, sustained or severe lymphocytopenia increases vulnerability to infections and may indicate serious underlying disease, requiring medical attention.
Can I boost my lymphocytes naturally?
You cannot directly “boost” lymphocyte counts like turning a switch, but supporting overall immune health helps optimize function. Focus on adequate sleep, balanced nutrition, regular exercise, and managing chronic conditions. Always consult a healthcare provider before starting supplements.
Conclusion: Taking Control of Your Immune Health
Discovering low lymphocytes can be unsettling, but it’s often the first step toward better health. Whether due to medication, illness, or lifestyle factors, identifying the cause empowers informed decisions. Most importantly, early awareness allows intervention before complications arise. Work closely with your healthcare provider, stay vigilant about recurring infections, and prioritize foundational wellness habits.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?