A low white blood cell (WBC) count, also known as leukopenia, is more than just a number on a lab report—it can be an early signal of underlying health issues or immune system challenges. White blood cells are essential soldiers in the body’s defense against infections, and when their numbers drop below normal, your ability to fight off bacteria, viruses, and other pathogens may be compromised. While a single low reading isn’t always cause for alarm, persistent or severe reductions warrant attention. Understanding what drives this condition—and what steps you can take—empowers you to act proactively.
What Is a Normal WBC Count?
The typical range for white blood cells in adults is between 4,000 and 11,000 cells per microliter of blood. A count below 4,000 is generally considered low, though thresholds can vary slightly depending on the laboratory. Children often have higher baseline levels, and values fluctuate throughout the day due to stress, exercise, or illness.
It's important to interpret WBC results in context. A mildly low count in an otherwise healthy person may not require treatment, while a significantly reduced level in someone undergoing chemotherapy demands close monitoring. The type of white blood cell affected—neutrophils, lymphocytes, monocytes, eosinophils, or basophils—also influences clinical significance.
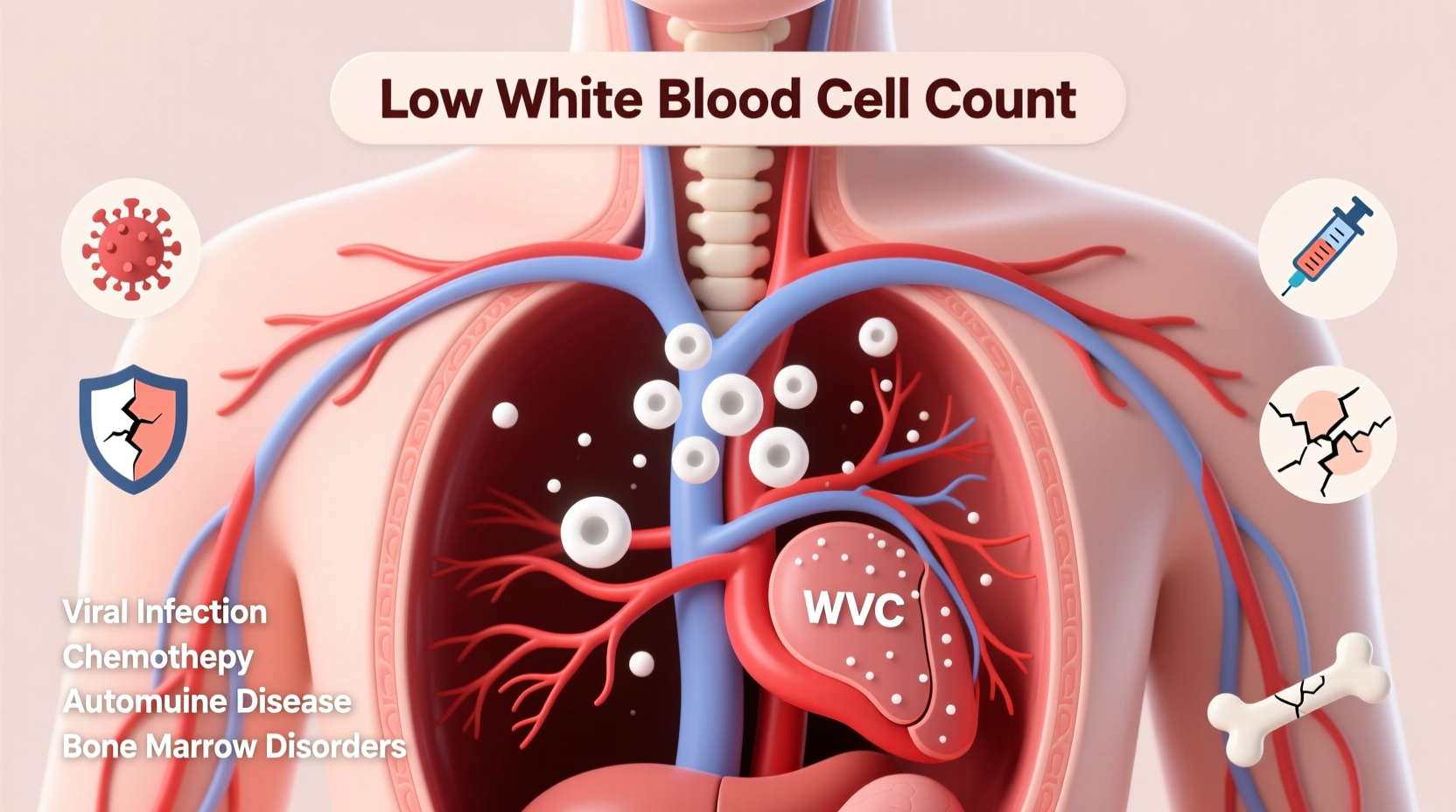
Common Causes of Low WBC Count
Leukopenia arises from a variety of sources, ranging from temporary conditions to chronic diseases. Identifying the root cause is crucial for appropriate management.
- Viral Infections: Conditions like influenza, HIV, hepatitis, and Epstein-Barr virus can temporarily suppress bone marrow activity, reducing WBC production.
- Bone Marrow Disorders: Diseases such as aplastic anemia, myelodysplastic syndromes, and leukemia interfere with the body’s ability to generate adequate blood cells.
- Autoimmune Conditions: Lupus and rheumatoid arthritis may lead the immune system to attack its own white blood cells.
- Nutritional Deficiencies: Lack of vitamin B12, folate, copper, or zinc impairs cellular development and immune function.
- Medications: Chemotherapy, certain antibiotics (like chloramphenicol), antipsychotics, and antithyroid drugs are known to lower WBC counts.
- Radiation Exposure: Therapeutic or environmental radiation damages rapidly dividing cells, including those in the bone marrow.
- Severe Infections: Overwhelming bacterial infections (e.g., sepsis) can deplete WBCs faster than they’re produced.
“Not all low WBC counts indicate serious disease, but they should never be ignored—especially if accompanied by recurrent infections.” — Dr. Alan Reyes, Hematologist at Boston General Hospital
Recognizing Symptoms and Risks
Many people with mild leukopenia experience no symptoms at all. However, when WBC levels fall significantly, signs of weakened immunity become apparent. These include:
- Frequent or prolonged infections (e.g., sinusitis, urinary tract infections)
- Fever without obvious cause
- Slow healing of cuts or wounds
- Mouth ulcers or sore throat
- Fatigue and general malaise
The greatest risk associated with low WBC count is susceptibility to opportunistic infections. Neutropenia—a subtype involving low neutrophil levels—is particularly concerning because neutrophils are the first responders to bacterial threats. When absolute neutrophil count (ANC) drops below 500/μL, the risk of life-threatening infection increases sharply.
| ANC Level (cells/μL) | Risk Category | Clinical Implication |
|---|---|---|
| >1,500 | Normal | No increased infection risk |
| 1,000–1,500 | Mild Neutropenia | Slight risk increase |
| 500–1,000 | Moderate Neutropena | Moderate infection risk |
| <500 | Severe Neutropenia | High risk; requires protective measures |
Diagnosis and Evaluation Process
If a routine CBC reveals a low WBC count, further investigation typically follows. Your healthcare provider will likely consider your medical history, medications, recent illnesses, and symptoms before ordering additional tests.
- Repeat CBC with Differential: Confirms whether the initial result was a transient dip or a consistent trend.
- Peripheral Blood Smear: Allows visual assessment of cell morphology to detect abnormalities.
- Vitamin Levels: Checks for deficiencies in B12, folate, and other nutrients critical for hematopoiesis.
- Infection Screening: Tests for HIV, hepatitis, tuberculosis, or other chronic infections.
- Bone Marrow Biopsy: Reserved for cases where malignancy or marrow failure is suspected.
Genetic testing may also be indicated in rare inherited disorders affecting blood cell production, such as Kostmann syndrome.
Mini Case Study: Maria’s Unexplained Fatigue
Maria, a 42-year-old teacher, visited her primary care physician after experiencing repeated colds over three months and persistent fatigue. Her CBC showed a WBC count of 3,200/μL with low neutrophils. Further evaluation revealed she had been taking methimazole for hyperthyroidism. The medication was identified as the likely culprit. After switching to an alternative treatment under supervision, her WBC levels normalized within six weeks, and her energy returned. This case highlights how medications can subtly impact immune markers—and why reviewing drug regimens is essential.
Supporting Healthy WBC Levels Naturally
While medical treatment depends on the underlying cause, lifestyle and dietary choices can support immune resilience and optimal blood cell production.
Key strategies include:
- Eating a balanced diet high in leafy greens, lean proteins, nuts, seeds, and citrus fruits
- Maintaining adequate hydration to support circulation and detoxification
- Managing stress through mindfulness, yoga, or regular physical activity
- Avoiding unnecessary antibiotics and limiting alcohol intake
- Practicing good hygiene to reduce infection burden on the immune system
Checklist: Daily Habits to Support Immune Health
- ✅ Eat at least five servings of colorful vegetables and fruits
- ✅ Get 7–8 hours of quality sleep each night
- ✅ Engage in moderate exercise (e.g., brisk walking) for 30 minutes most days
- ✅ Wash hands regularly, especially during cold and flu season
- ✅ Review medications annually with your doctor for potential side effects
- ✅ Schedule annual blood work to monitor trends
Frequently Asked Questions
Can stress cause a low white blood cell count?
Yes, chronic psychological stress can dysregulate the immune system and suppress bone marrow activity over time. Elevated cortisol levels have been linked to reduced lymphocyte counts and impaired immune surveillance.
Is a low WBC count dangerous during pregnancy?
Pregnancy can slightly lower WBC counts due to hemodilution, but significant drops should be evaluated. Some autoimmune conditions that affect WBCs may flare during pregnancy and require specialized care.
Do I need treatment if my WBC is only slightly low?
Not necessarily. If you’re asymptomatic and the reduction is mild, your doctor may recommend monitoring rather than intervention. Treatment is usually reserved for those with symptoms, recurrent infections, or very low counts.
Conclusion: Taking Charge of Your Immune Health
Understanding what a low WBC count means goes beyond interpreting a lab value—it involves recognizing patterns in your health, evaluating lifestyle factors, and partnering with your healthcare provider. Whether the cause is temporary or points to a deeper issue, early awareness gives you the advantage. Don’t dismiss subtle signs like frequent infections or unexplained fatigue. With informed decisions and proactive habits, you can support your immune system and maintain better long-term health.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?