The apical pulse is one of the most reliable indicators of cardiac function, offering clinicians direct insight into the heart’s rhythm, rate, and strength. Unlike peripheral pulses, which can be influenced by vascular resistance or poor circulation, the apical pulse reflects actual ventricular contractions. Accurately locating it is essential for diagnosing arrhythmias, monitoring patients with cardiovascular conditions, and ensuring precise assessments—especially in infants, elderly individuals, and those with weak peripheral pulses.
Despite its importance, many healthcare providers, especially students and new practitioners, struggle with consistent apical pulse identification. This guide breaks down the process into clear, actionable steps, equipping you with the knowledge and confidence to perform accurate heart assessments every time.
Why the Apical Pulse Matters
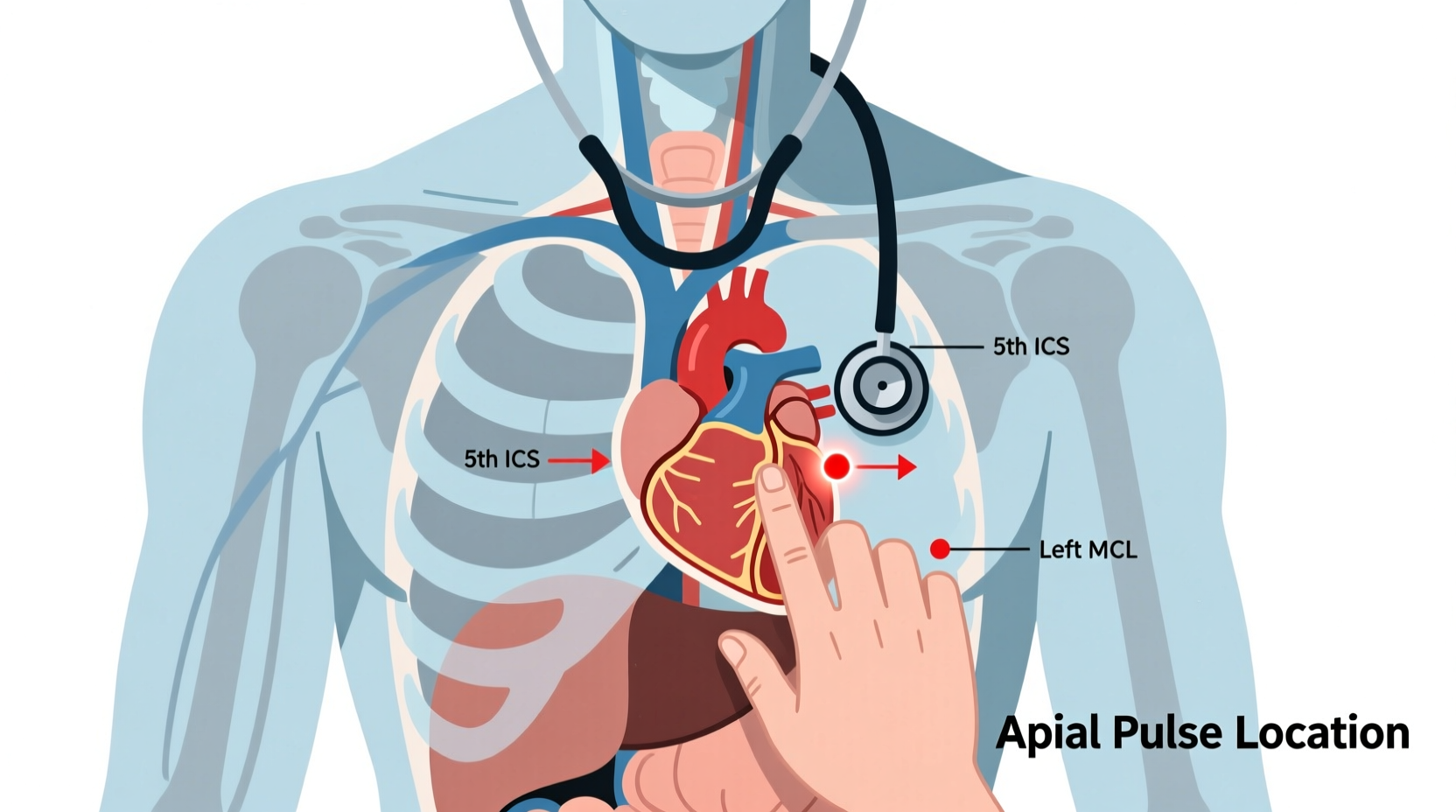
The apical pulse is auscultated at the apex of the heart, typically using a stethoscope over the left fifth intercostal space at the midclavicular line. It provides a more accurate representation of heart rate than radial or carotid pulses, particularly when discrepancies exist between electrical activity (seen on ECG) and mechanical output (palpable beats).
In clinical practice, apical pulse assessment is standard for:
- Evaluating irregular rhythms such as atrial fibrillation
- Monitoring infants and young children whose peripheral pulses are difficult to palpate
- Assessing patients on cardiac medications like digoxin, where heart rate must be precisely measured before administration
- Detecting pulse deficits—when the apical rate exceeds the radial rate, indicating ineffective contractions
“Apical pulse assessment remains the gold standard for heart rate evaluation in symptomatic bradycardia or tachycardia.” — Dr. Linda Harper, Cardiac Nurse Educator, Johns Hopkins School of Nursing
Step-by-Step Guide to Locating the Apical Pulse
Follow these seven key steps to consistently locate and assess the apical pulse with precision.
- Prepare the patient and environment: Ensure the patient is lying comfortably in a supine or semi-Fowler’s position. The room should be quiet to allow for clear auscultation. Expose the chest area while maintaining privacy.
- Identify anatomical landmarks: Locate the sternum, then find the angle of Louis (the bump at the second rib). Slide your fingers laterally to feel the second intercostal space. Count down to the fifth intercostal space along the left midclavicular line—the typical location of the apex beat.
- Position the stethoscope correctly: Use the diaphragm of the stethoscope for high-frequency sounds like S1 and S2. Place it firmly but gently over the identified point. Avoid placing it directly over ribs, which can distort sound transmission.
- Auscultate systematically: Listen for at least 30 seconds if the rhythm is regular; extend to a full minute if irregular. Focus on identifying the “lub-dub” pattern: S1 (closure of mitral and tricuspid valves) marks ventricular systole and corresponds to the apical impulse.
- Count the heart rate accurately: For regular rhythms, multiply the number of beats in 30 seconds by two. For irregular rhythms, count for a full 60 seconds to capture variability.
- Assess rhythm and quality: Note whether the rhythm is regular, regularly irregular, or irregularly irregular. Evaluate the intensity and symmetry of heart sounds. Diminished S1 may suggest conduction abnormalities or reduced contractility.
- Compare with peripheral pulse: Simultaneously palpate the radial pulse while listening apically to detect any pulse deficit—a sign of inefficient cardiac output.
Common Challenges and How to Overcome Them
Even experienced clinicians encounter obstacles when assessing the apical pulse. Body habitus, lung disease, and patient positioning can all interfere with accuracy.
| Challenge | Cause | Solution |
|---|---|---|
| Inaudible or faint sounds | Obesity, emphysema, pleural effusion | Use the bell of the stethoscope; reposition patient left lateral; ensure stethoscope seal |
| Incorrect landmark identification | Anatomical variation, breast tissue interference | Prioritize bony landmarks; displace breast tissue upward and laterally when necessary |
| Confusing respiratory sounds with heart sounds | Wheezing, crackles, or patient movement | Ask patient to hold breath briefly; differentiate timing relative to cardiac cycle |
| Misidentifying S1 and S2 | High-pitched lung sounds, valve pathology | Palpate carotid pulse simultaneously—S1 coincides with carotid upstroke |
Practical Tips for Consistent Accuracy
- Always warm the stethoscope before placing it on the skin to prevent muscle tensing or patient discomfort.
- Practice landmark identification daily during clinical rotations—even on healthy volunteers—to build tactile memory.
- Use a clock with a second hand or digital timer to ensure accurate counting intervals.
- Document findings clearly: include rate, rhythm, presence of murmur, and any pulse deficit observed.
- Reassess after interventions such as medication administration or positional changes.
Real-World Example: Detecting a Pulse Deficit
Nurse Elena was conducting a routine assessment on Mr. Thompson, a 72-year-old man admitted for fatigue and shortness of breath. His radial pulse was 88 bpm and irregular. When she auscultated the apical pulse, she counted 110 beats per minute—also irregular. Recognizing the 22-beat discrepancy, she immediately notified the physician.
An ECG confirmed atrial fibrillation with rapid ventricular response. The pulse deficit explained his symptoms of low perfusion. Thanks to her accurate apical assessment, the care team initiated rate control therapy promptly, preventing further complications.
Essential Checklist for Apical Pulse Assessment
Use this checklist before every apical pulse evaluation to ensure thoroughness and consistency:
- ✅ Patient positioned comfortably (supine or left lateral)
- ✅ Chest exposed with dignity preserved
- ✅ Stethoscope warmed and functioning properly
- ✅ Landmarks identified using bony references
- ✅ Diaphragm placed at left fifth intercostal space, midclavicular line
- ✅ Heart rate counted for full 60 seconds if rhythm is irregular
- ✅ Rhythm classified (regular, irregular, etc.)
- ✅ Peripheral pulse compared to detect deficit
- ✅ Findings documented clearly in patient record
Frequently Asked Questions
How long should I listen to the apical pulse?
For a regular rhythm, listen for at least 30 seconds and multiply by two. For an irregular rhythm, listen for a full 60 seconds to ensure accuracy. This prevents underestimation or overestimation due to beat-to-beat variability.
Can I use my fingers instead of a stethoscope?
No. The apical impulse (or point of maximal impulse, PMI) can sometimes be palpated, but true apical pulse assessment requires auscultation to hear S1 and S2. Palpation alone cannot distinguish subtle rhythm changes or confirm mechanical contraction timing.
What does a displaced apical pulse indicate?
A PMI located beyond the midclavicular line or in a higher intercostal space may indicate cardiac enlargement, left ventricular hypertrophy, or conditions like cardiomyopathy. Always report a displaced impulse for further diagnostic evaluation.
Conclusion: Mastering Precision in Cardiac Care
Locating the apical pulse is more than a technical skill—it's a foundational element of competent cardiovascular assessment. With deliberate practice, attention to anatomy, and consistent technique, you can significantly improve diagnostic accuracy and patient outcomes. Whether you're a nursing student, paramedic, or seasoned clinician, refining this skill enhances your ability to detect life-threatening conditions early and provide evidence-based care.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?