Accurate body temperature measurement is essential for monitoring health, detecting illness early, and making informed decisions about medical care. Digital thermometers have replaced traditional mercury models in most homes due to their speed, precision, and safety. Yet, even the most advanced device delivers unreliable results if used incorrectly. Understanding the proper technique—whether for oral, rectal, axillary (underarm), or forehead readings—can make the difference between spotting a fever early and missing it entirely.
Understanding Your Digital Thermometer
Digital thermometers come in various types: oral, rectal, multi-use, temporal artery (forehead), and tympanic (ear). While some are designed for specific uses, many modern models are versatile with interchangeable probes or modes. Most operate on batteries and feature an easy-to-read digital display, beep signals when complete, and memory functions to store previous readings.
The key to accuracy lies not only in the device but also in how it’s used. Factors such as recent food or drink consumption, placement technique, environmental conditions, and even user anxiety can affect results. To get reliable data, follow standardized procedures based on the method of measurement.
Step-by-Step Guide to Taking Accurate Temperature Readings
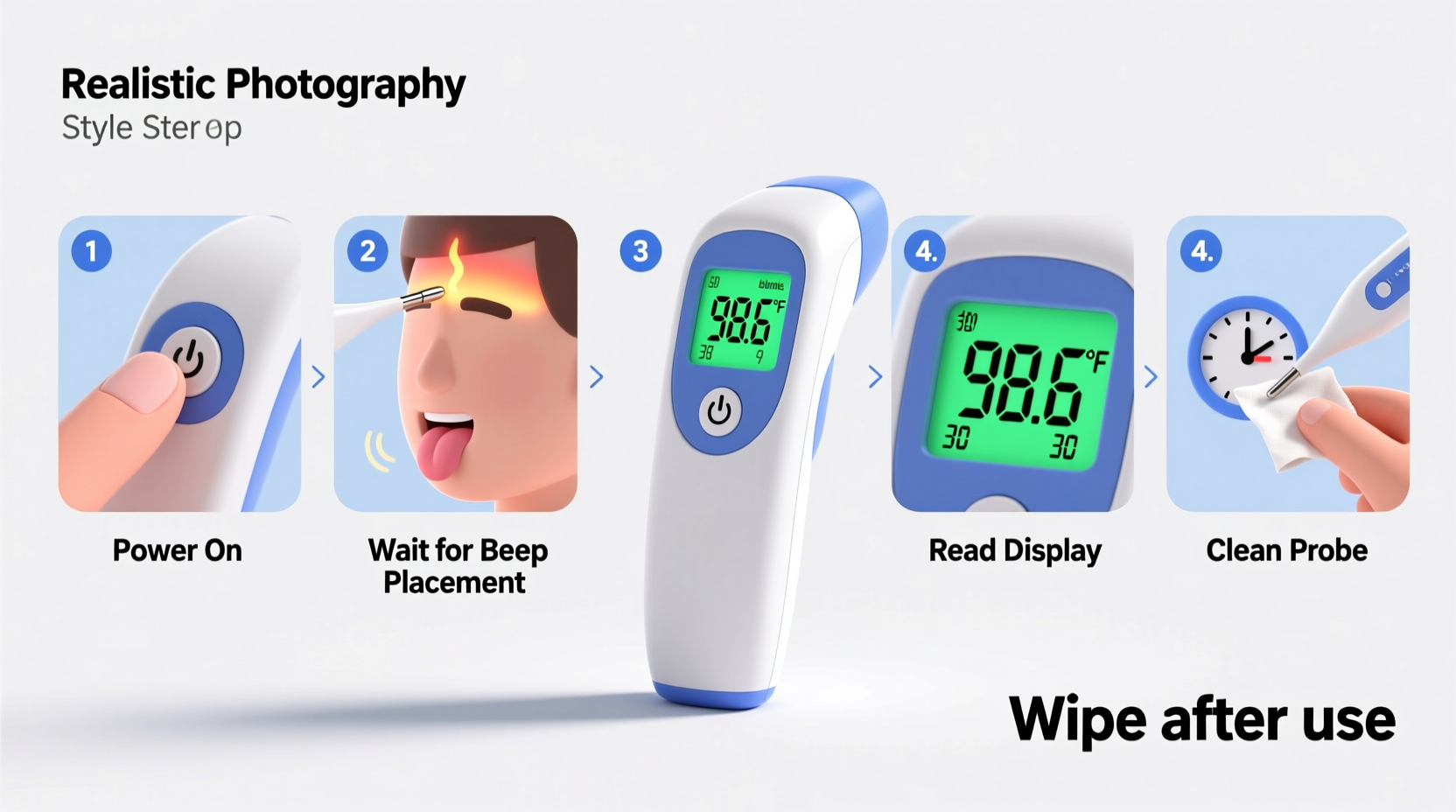
Follow this comprehensive sequence to ensure consistency and precision across different methods:
- Prepare the Thermometer: Turn it on and check that the battery is functional. Clean the probe with lukewarm water and mild soap or rubbing alcohol, then rinse and dry thoroughly.
- Choose the Measurement Site: Decide whether you're using oral, rectal, axillary, or forehead mode based on age, comfort, and clinical need.
- Wait After Eating or Drinking: For oral readings, wait at least 15–30 minutes after consuming hot or cold substances.
- Position Correctly: Place the thermometer tip under the tongue (oral), gently into the rectum (rectal), high in the armpit (axillary), or swipe across the forehead (temporal).
- Hold Steady Until Signal: Keep the mouth closed during oral measurements; hold babies still during rectal or axillary checks. Wait for the beep indicating completion.
- Read and Record: Note the temperature displayed. Some devices auto-save, but manual logging helps track trends over time.
- Clean After Use: Disinfect the probe again before storing, especially if shared among family members.
Best Practices by Measurement Type
| Method | Accuracy Level | Recommended For | Key Tips |
|---|---|---|---|
| Rectal | Very High | Infants and toddlers under 3 years | Lubricate tip; insert ½ to 1 inch; hold gently but firmly |
| Oral | High | Children over 4 and adults | Avoid talking; keep lips sealed; don’t eat/drink beforehand |
| Axillary (Armpit) | Moderate | Preliminary screening in all ages | Ensure skin is dry; press arm tightly against body |
| Temporal (Forehead) | High (when used correctly) | All ages, especially infants and sleeping patients | Swipe slowly across clean forehead; avoid hair or sweat |
| Tympanic (Ear) | High (with proper angle) | Children over 6 months | Pull ear back slightly; aim toward opposite eye; use clean lens cover |
Common Mistakes That Skew Results
- Using a dirty or improperly cleaned probe
- Taking an oral reading immediately after drinking coffee or ice water
- Not holding the thermometer long enough—removing it before the beep
- Placing the armpit thermometer over clothing instead of bare skin
- Failing to calibrate or replace weak batteries
- Using a forehead thermometer in a drafty or overheated room
“Even a slight deviation in placement can result in a 0.5°C to 1°C error—enough to misclassify a fever.” — Dr. Lena Patel, Pediatric Nurse Practitioner
When Accuracy Matters Most: A Real-Life Example
Six-month-old Noah had been fussy for two days. His parents noticed he was feeding less and seemed warm to the touch. They used a temporal thermometer and recorded 37.7°C (99.9°F)—a borderline result. Believing it wasn’t concerning, they waited another day. By morning, Noah was lethargic and running a high fever. At the pediatric clinic, a rectal reading revealed 39.4°C (103°F), confirming a serious infection requiring prompt treatment.
The initial forehead scan likely missed the true temperature due to residual sweat and quick swiping. This case highlights why precise methods matter, especially in young children whose immune systems respond rapidly. For infants under one year, rectal temperatures remain the gold standard when clinical decisions are needed.
Checklist: Ensuring Reliable Digital Thermometer Use
Use this checklist every time you take a temperature to maintain consistency:
- ✅ Clean the probe before and after each use
- ✅ Verify the battery is charged
- ✅ Select the correct mode (oral, rectal, etc.)
- ✅ Wait 15–30 minutes after eating/drinking (for oral)
- ✅ Position the thermometer correctly according to site guidelines
- ✅ Hold in place until the device beeps
- ✅ Record the exact temperature and time
- ✅ Store the thermometer in a clean, dry place away from direct sunlight
Expert Insights on Home Monitoring
Health professionals emphasize that while digital thermometers are user-friendly, interpretation requires context. A slightly elevated temperature may not always indicate illness, just as a normal reading doesn't rule out infection in immunocompromised individuals.
“Parents should focus on trends, not single numbers. Two readings of 38.3°C taken six hours apart are more telling than one isolated spike.” — Dr. Alan Zhou, Family Medicine Specialist
Additionally, experts recommend keeping a logbook or digital record, especially during illness outbreaks or post-vaccination periods. Tracking patterns allows caregivers and clinicians to assess progression and response to treatment.
Frequently Asked Questions
How do I know if my digital thermometer is accurate?
Test it by placing the probe in ice water (0°C / 32°F) or boiling water (100°C / 212°F at sea level). It should read within ±0.1–0.2°C of the expected value. Alternatively, compare it side-by-side with a calibrated clinical model.
Can I use the same thermometer for oral and rectal measurements?
You can, but only if it's clearly labeled and meticulously cleaned between uses. Ideally, maintain separate devices—one marked “oral,” another “rectal”—to eliminate contamination risks, especially in households with infants.
Why does my forehead thermometer give different readings each time?
Forehead thermometers are sensitive to ambient temperature, sweat, drafts, and scanning speed. Ensure the forehead is dry, the room is stable (16–40°C), and you follow the manufacturer’s swipe instructions exactly. Avoid taking readings right after coming indoors from extreme weather.
Final Thoughts: Precision Starts with Practice
Mastering how to use a digital thermometer goes beyond pressing a button—it involves preparation, proper technique, and awareness of influencing factors. Whether monitoring a child’s fever, tracking ovulation, or checking for signs of infection, accurate temperature data supports better health decisions. By following evidence-based steps, avoiding common errors, and validating results when necessary, you turn a simple tool into a powerful ally in maintaining wellness.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?