In high-pressure healthcare environments, nurses are frontline defenders against infectious diseases. Personal protective equipment (PPE) is not just a requirement—it’s a lifeline. Yet, even experienced professionals can make errors in selection, donning, doffing, or disposal. This guide provides actionable insights into the proper use of PPE, grounded in clinical best practices and real-world application. The goal is simple: protect yourself, your patients, and your team.
Understanding the Core Components of PPE
PPE encompasses several key items designed to create barriers between healthcare workers and infectious agents. Each component serves a specific function and must be used appropriately based on the situation.
- Gloves: Protect hands from direct contact with blood, bodily fluids, and contaminated surfaces.
- Masks and Respirators: Surgical masks block large droplets; N95 respirators filter airborne particles when properly fitted.
- Gowns: Prevent contamination of skin and clothing during procedures involving fluid exposure.
- Face Shields and Goggles: Shield eyes, nose, and mouth from splashes and sprays.
- Head and Shoe Covers: Used in high-risk isolation units or surgical settings to minimize cross-contamination.
The choice of PPE depends on the mode of transmission risk—contact, droplet, or airborne—and the nature of patient interaction. Misuse or underuse compromises safety; overuse strains supply chains and increases waste.
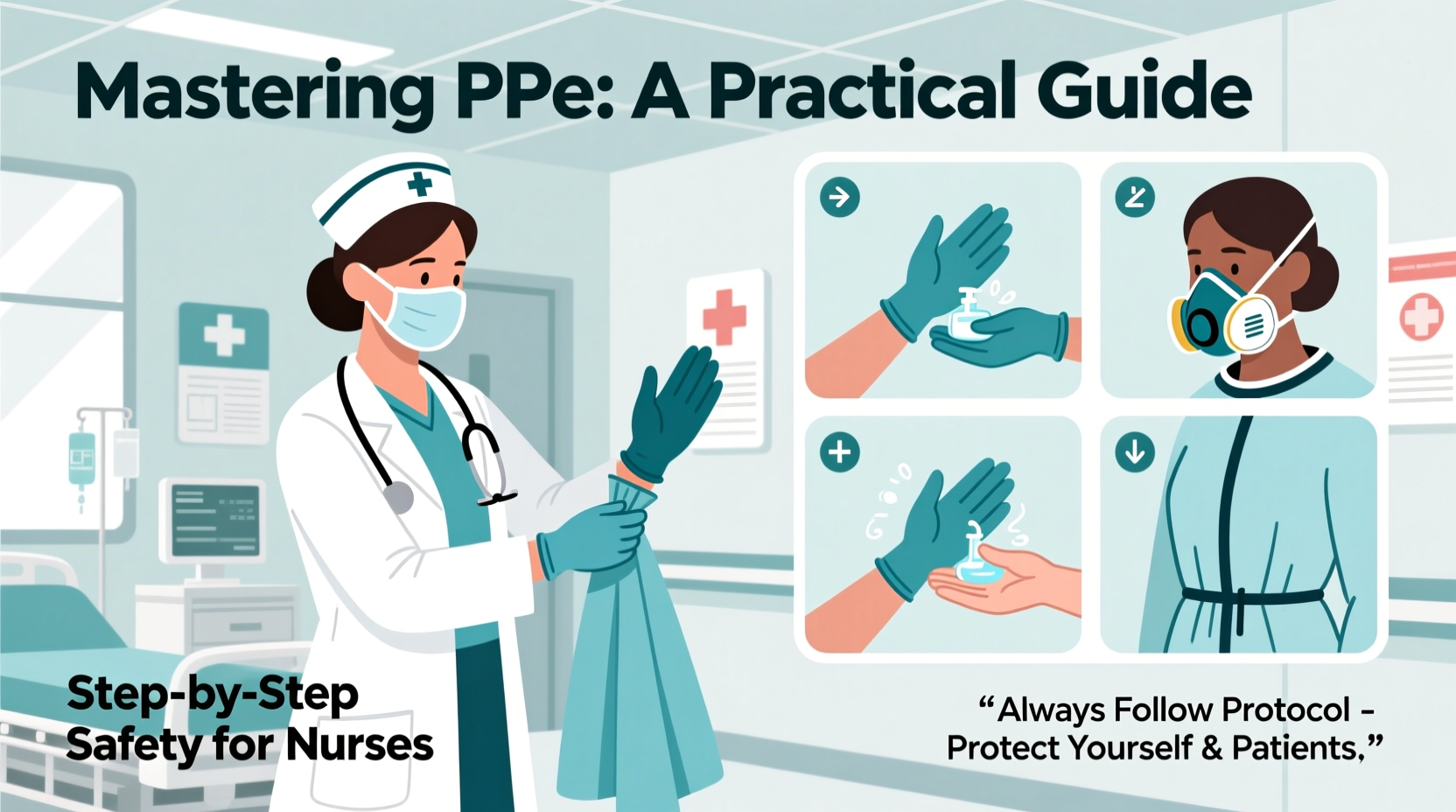
Step-by-Step Guide to Donning and Doffing PPE
Correct sequence matters. Errors during donning (putting on) or doffing (removing) PPE are among the most common causes of self-contamination. Follow this evidence-based protocol:
- Hand hygiene: Wash hands thoroughly with soap and water or use alcohol-based sanitizer.
- Gown: Put on the gown first, securing ties at neck and waist. Ensure it fully covers torso and arms.
- Mask/Respirator: Place over nose and mouth. Mold nose clip and secure straps behind head. Perform a seal check if using an N95.
- Goggles/Face Shield: Adjust to cover eyes completely without gaps.
- Gloves: Slide gloves over cuffs of the gown to ensure no skin is exposed.
When leaving the patient area, doffing follows the reverse order to minimize contamination:
- Gloves: Peel off from wrist, turning inside out. Discard immediately.
- Gown: Unfasten ties, peel away from neck and shoulders, rolling down so the outside surface folds inward. Discard carefully.
- Hand hygiene: Clean hands after removing gloves and gown.
- Goggles/Face Shield: Remove by handling only the straps or sides. If reusable, clean according to protocol.
- Mask/Respirator: Remove by ear loops or ties—never touch the front. Discard safely.
- Final hand hygiene: Wash hands again thoroughly.
This process should be practiced regularly, especially during orientation and annual training. Simulation drills improve muscle memory and reduce panic in emergencies.
Common Mistakes and How to Avoid Them
Even seasoned nurses can fall into habits that compromise protection. Awareness is the first step toward correction.
| Mistake | Risk | Prevention Strategy |
|---|---|---|
| Touching face while wearing gloves | Transfers pathogens to mucous membranes | Train to keep hands below chin unless adjusting PPE intentionally |
| Reusing disposable PPE | Increases contamination risk | Follow facility policy strictly—no reuse of single-use items |
| Inadequate seal check on N95 | Allows unfiltered air intake | Perform user seal check every time; re-fit test annually |
| Doffing mask by the front | Contaminates hands | Always remove by straps or ties |
| Wearing PPE outside designated zones | Spreads contamination to clean areas | Remove PPE before exiting patient rooms or isolation units |
“PPE is only as effective as the person wearing it. Technique trumps equipment.” — Dr. Linda Chen, Infection Control Specialist, Johns Hopkins Hospital
Real-World Scenario: A Close Call in the ICU
During a surge in respiratory infections, Nurse Elena responded to a code blue in Room 7—a patient later confirmed positive for tuberculosis. In the rush, she quickly grabbed a surgical mask instead of an N95. She entered the room, assisted with intubation, and remained for 20 minutes before realizing her error.
Post-event, she reported the incident through her hospital’s safety channel. She underwent TB screening and was placed on prophylactic treatment. The event triggered a unit-wide refresher on airborne precautions and led to color-coded bins near entrances indicating required PPE levels.
This case underscores two truths: human error happens, but systems must support recovery. Clear signage, peer accountability, and non-punitive reporting cultures are essential to safety.
Essential PPE Checklist for Nurses
Use this checklist daily, especially when working in high-risk or unfamiliar units:
- ✅ Confirm patient’s isolation status before entry
- ✅ Select appropriate PPE based on transmission risk
- ✅ Inspect PPE for tears, defects, or moisture damage
- ✅ Perform hand hygiene before donning
- ✅ Follow correct donning sequence
- ✅ Conduct N95 seal check (if applicable)
- ✅ Avoid touching face or adjusting PPE mid-task
- ✅ Doff in correct order, avoiding contact with contaminated surfaces
- ✅ Dispose of PPE in designated waste containers
- ✅ Perform final hand hygiene immediately after removal
- ✅ Report any breaches or exposures promptly
Frequently Asked Questions
Can I use a surgical mask instead of an N95 when one is unavailable?
Surgical masks do not provide adequate protection against airborne pathogens like TB or measles. They block droplets but not fine aerosols. If an N95 is required and unavailable, notify your supervisor immediately. Use alternative engineering controls (e.g., negative pressure rooms) and limit staff exposure until proper respirators are available.
How often should I be fit-tested for an N95 respirator?
OSHA and CDC recommend annual fit testing. Additional testing is required if there are significant changes in facial structure (weight gain/loss, dental work, facial surgery) or if you notice difficulty achieving a seal.
Is it safe to modify PPE for comfort, like cutting holes in gowns or wearing makeup under masks?
No. Altering PPE invalidates its protective integrity. Makeup, facial hair, or jewelry under masks can break the seal and increase exposure risk. Maintain clean-shaven faces for respirator use and avoid accessories that interfere with fit.
Conclusion: Commitment to Safety Starts with You
Mastering PPE isn’t about memorizing rules—it’s about cultivating a mindset of vigilance, precision, and responsibility. Every time you put on gloves or adjust a face shield, you’re making a silent promise: to care safely, act professionally, and lead by example. Infection prevention is a shared mission, and nurses are its backbone.
Review protocols, participate in drills, speak up when something seems off, and mentor new staff. Your attention to detail doesn’t just protect you—it safeguards entire care teams and vulnerable patients.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?