Sleep is non-negotiable for health, yet millions struggle to get enough of it. Melatonin, a popular over-the-counter sleep aid, is often the first line of defense against insomnia or irregular sleep schedules. But what happens when melatonin stops working—or never worked at all? You're not alone. Many people report that melatonin doesn’t help them fall asleep, stay asleep, or feel rested in the morning. The issue isn’t always with the supplement itself—it’s often how, when, or why it’s being used. Understanding the root causes behind melatonin’s ineffectiveness is key to restoring restful sleep.
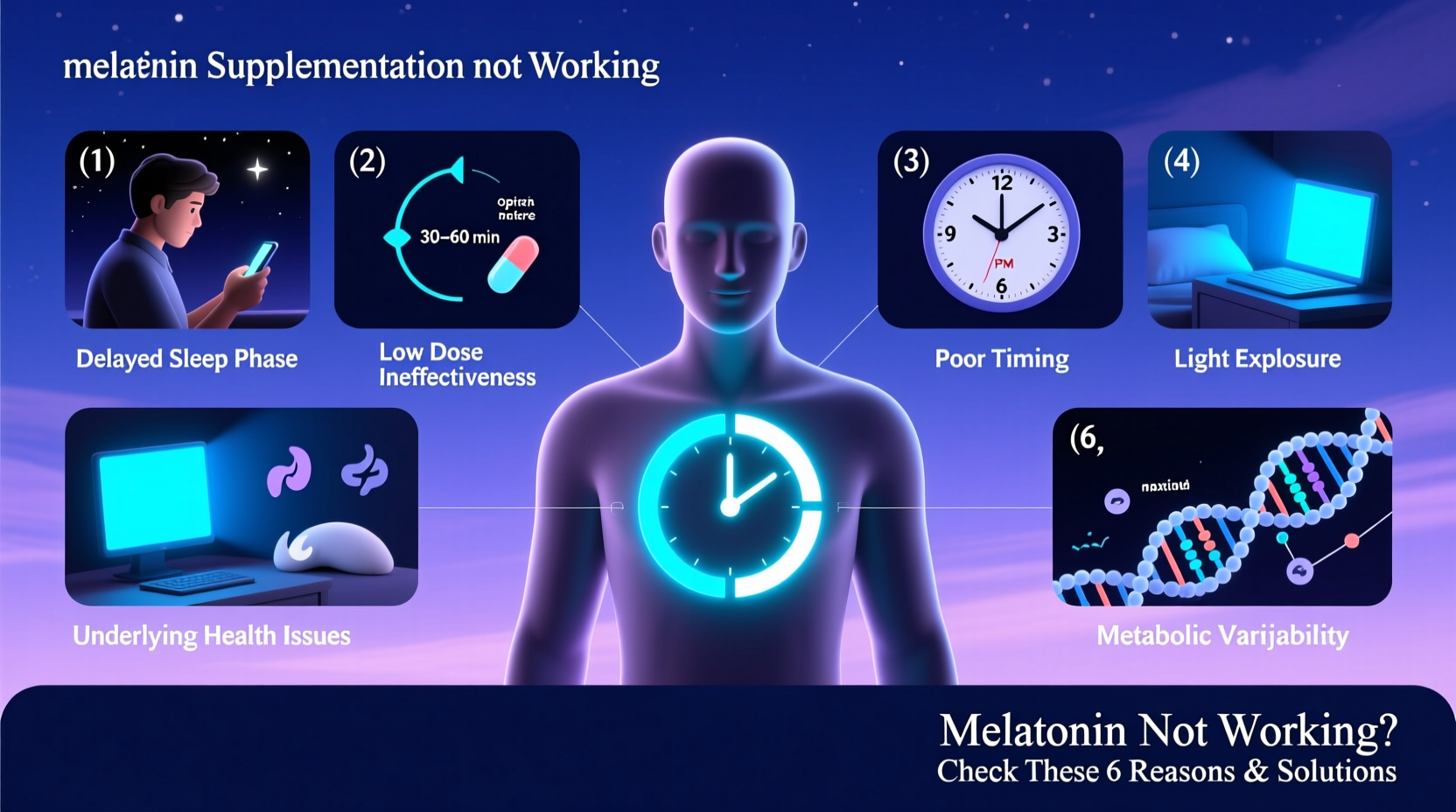
Why Melatonin Might Not Be Working for You
Melatonin is a hormone naturally produced by the pineal gland in response to darkness. It signals to your body that it’s time to wind down. Supplemental melatonin aims to boost these levels artificially, especially useful for jet lag, shift work, or occasional sleeplessness. However, its effectiveness depends on multiple factors—timing, dosage, underlying health conditions, and lifestyle habits.
If melatonin isn’t delivering results, it's likely due to one or more of the following common issues:
- Taking it at the wrong time
- Using too high or too low a dose
- Underlying sleep disorders like sleep apnea or circadian rhythm misalignment
- Poor sleep hygiene (e.g., screen exposure before bed)
- Developing tolerance from long-term use
- Interactions with medications or other supplements
- Non-sleep-related fatigue (e.g., stress, depression, chronic illness)
The Timing Trap: When You Take Melatonin Matters Most
One of the most frequent reasons melatonin fails is improper timing. Taking it too early or too late disrupts your natural circadian rhythm rather than supporting it.
The ideal window is 30 to 60 minutes before bedtime. But if you’re trying to adjust your sleep schedule—like shifting from night owl to early riser—you may need to take it earlier, such as 2 hours before your desired sleep onset.
Dosage: More Isn't Better
Many assume that if 1 mg doesn’t work, 5 or 10 mg will. This is a misconception. Research shows that doses above 1–3 mg offer little additional benefit and can actually worsen sleep quality.
Excess melatonin can lead to next-day grogginess, vivid dreams, or even rebound insomnia. The body only needs a small signal to initiate sleep—not a flood of hormones.
“Most adults respond well to 0.5 to 1 mg of melatonin. Higher doses can desensitize receptors over time.” — Dr. Rebecca Robbins, Sleep Scientist, Harvard Medical School
| Dosage (mg) | Best For | Risks |
|---|---|---|
| 0.3 – 0.5 | Maintenance, sensitive individuals | May be too low for some |
| 1 – 2 | General use, occasional insomnia | Minimal side effects |
| 3 – 10 | Jet lag, shift work (short-term) | Grogginess, hormonal imbalance |
Underlying Sleep Disorders Are Often Overlooked
Melatonin helps regulate sleep timing but does not treat structural sleep problems. If you have obstructive sleep apnea, restless legs syndrome, or chronic insomnia, melatonin alone won’t resolve the core issue.
For example, someone with undiagnosed sleep apnea may fall asleep with melatonin but still wake up exhausted due to breathing interruptions throughout the night. In such cases, melatonin masks the symptom without addressing the cause.
Mini Case Study: Sarah’s Story
Sarah, a 42-year-old teacher, took 5 mg of melatonin nightly for six months. She fell asleep faster but woke up multiple times and felt drained each morning. After a sleep study, she was diagnosed with moderate sleep apnea. Once she started using a CPAP machine, her sleep improved dramatically—even without melatonin.
This highlights a critical point: melatonin is not a cure-all. Persistent poor sleep despite supplementation warrants medical evaluation.
How to Fix It: A Step-by-Step Guide to Restoring Melatonin Effectiveness
If melatonin has stopped working or never worked, don’t give up. Follow this evidence-based protocol to reset your system and improve sleep naturally.
- Stop taking melatonin for 5–7 days. This allows your body to recalibrate natural production.
- Establish a consistent sleep schedule. Go to bed and wake up at the same time every day, even on weekends.
- Limit blue light after 8 PM. Use night mode on devices or wear blue-light-blocking glasses.
- Create a dark sleeping environment. Use blackout curtains and cover electronic lights.
- Reintroduce melatonin at 0.5–1 mg. Take it 30–60 minutes before bed, only if needed.
- Avoid alcohol and caffeine after 2 PM. Both interfere with melatonin signaling.
- Get morning sunlight exposure. 10–15 minutes upon waking helps regulate your internal clock.
Lifestyle Factors That Undermine Melatonin
No supplement can overcome poor sleep hygiene. Common habits that sabotage melatonin include:
- Scrolling on phones or watching TV in bed
- Eating heavy meals late at night
- Inconsistent bedtimes
- High stress or anxiety levels
- Exercising too close to bedtime
Your environment sends stronger signals to your brain than any pill. Darkness triggers melatonin release; artificial light suppresses it. Even a quick glance at your phone during a nighttime bathroom trip can interrupt this process.
Checklist: Optimize Your Sleep Environment
- ✅ Keep bedroom temperature between 60–67°F (15–19°C)
- ✅ Use blackout curtains or a sleep mask
- ✅ Remove TVs, laptops, and phones from the bedroom
- ✅ Install red or amber nightlights for nighttime navigation
- ✅ Use white noise or earplugs if noise is an issue
When to See a Doctor
If you’ve optimized timing, dosage, and lifestyle—and still struggle with sleep—consult a healthcare provider. Chronic insomnia, daytime fatigue, or snoring could indicate conditions requiring specialized treatment.
Additionally, certain medications (like beta-blockers, antidepressants, or corticosteroids) can interfere with melatonin production. A doctor can assess whether your regimen needs adjustment.
FAQ
Can you become resistant to melatonin?
While true resistance is rare, long-term high-dose use may lead to reduced sensitivity. Taking breaks and using the lowest effective dose helps maintain responsiveness.
Is it safe to take melatonin every night?
Short-term use (up to 3 months) is generally safe for most adults. Long-term nightly use should be discussed with a healthcare provider, especially in older adults or those with immune conditions.
Why do I wake up at 3 AM even with melatonin?
This could be due to cortisol spikes, blood sugar fluctuations, or fragmented sleep architecture. Melatonin helps with sleep onset but not necessarily sleep maintenance. Consider adding glycine or addressing stress-related awakenings.
Conclusion
Melatonin not working doesn’t mean your sleep is beyond repair—it means it’s time to look deeper. The solution often lies not in higher doses, but in smarter habits, proper timing, and identifying hidden barriers to rest. By treating melatonin as a tool within a broader sleep strategy—not a standalone fix—you can reclaim natural, restorative sleep.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?