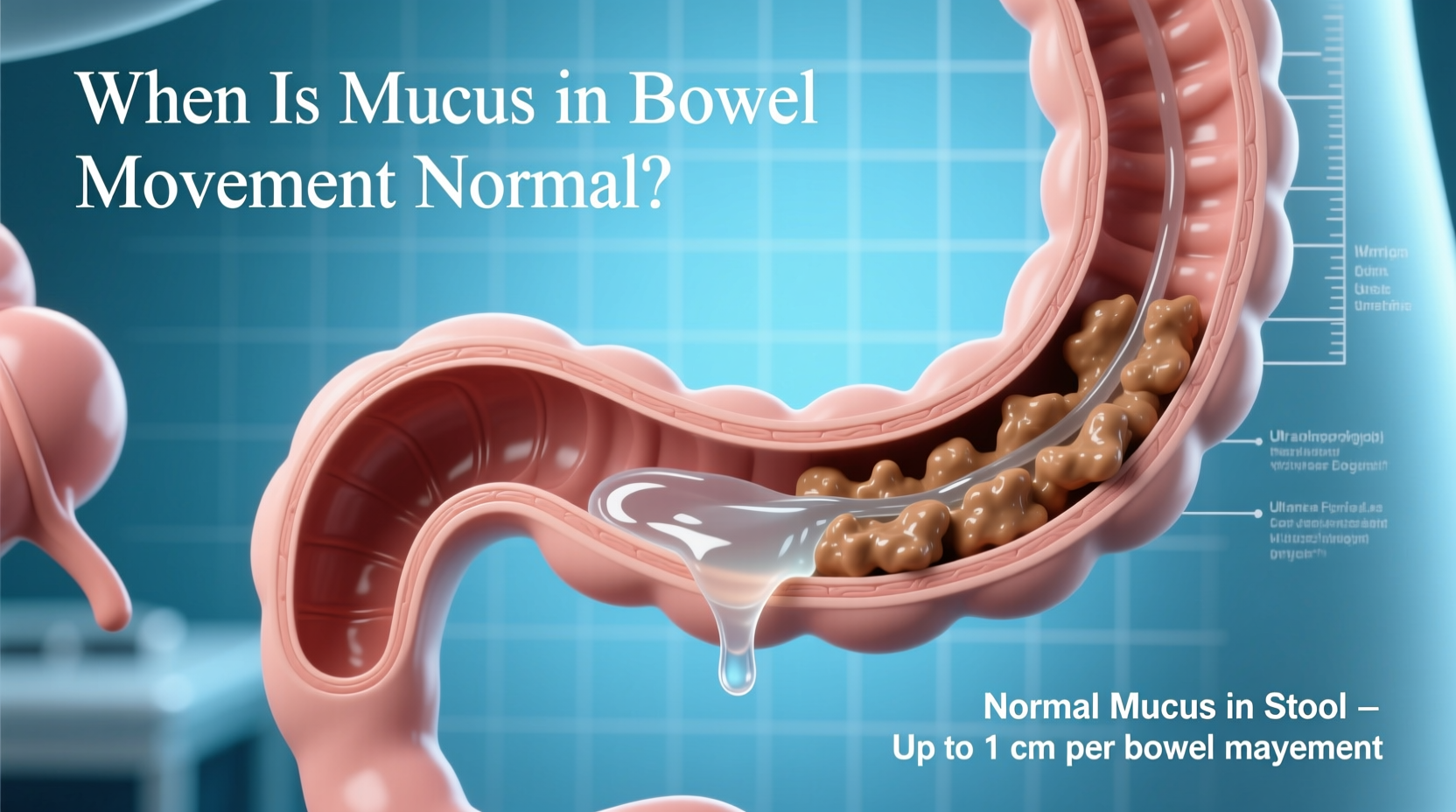
Mucus in the stool is something many people notice from time to time and often dismiss—until it becomes frequent or is accompanied by other symptoms. While small amounts of mucus are a natural part of healthy digestion, changes in color, quantity, or consistency can signal underlying issues. Understanding what’s normal versus what warrants medical attention helps prevent unnecessary worry and ensures timely care when needed.
The digestive tract naturally produces mucus to lubricate the intestines and help stool pass smoothly. It’s typically clear or white and not easily noticeable. However, when mucus becomes visible in your bowel movements—especially if it's yellow, green, bloody, or excessive—it may point to inflammation, infection, or chronic gastrointestinal conditions.
What Is Mucus and Why Does the Gut Produce It?
Mucus is a slippery, gel-like substance made primarily of water, glycoproteins, and electrolytes. In the gastrointestinal tract, it serves several critical functions:
- Lubricates the intestinal lining to ease stool passage
- Protects the gut wall from digestive enzymes and harmful bacteria
- Supports the growth of beneficial gut microbiota
- Traps pathogens before they invade deeper tissues
The large intestine and rectum contain specialized cells called goblet cells that secrete mucus continuously. Under normal conditions, this mucus mixes with stool but remains largely invisible. When production increases or the gut lining becomes irritated, more mucus may be expelled during defecation.
Common Causes of Visible Mucus in Stool
Visible mucus isn’t always a sign of disease. Several benign and temporary factors can increase mucus production:
- Dietary changes: High-fiber foods like raw vegetables or legumes can stimulate mucus secretion.
- Minor infections: Viral gastroenteritis (stomach flu) may temporarily increase mucus as the gut heals.
- Dehydration: Concentrated stools can irritate the colon, prompting excess mucus.
- Anal fissures or hemorrhoids: These conditions can produce mucus along with blood or discomfort.
- Stress: Emotional stress impacts gut motility and can alter mucus production.
In most cases, these causes resolve on their own within a few days without treatment.
When Mucus Signals a Health Concern
Persistent or abnormal mucus should not be ignored, especially when paired with other symptoms. Conditions associated with increased or discolored mucus include:
- Irritable Bowel Syndrome (IBS): Many IBS patients report mucus in stool, particularly during flare-ups involving diarrhea or constipation.
- Inflammatory Bowel Disease (IBD): Crohn’s disease and ulcerative colitis cause chronic gut inflammation, leading to mucus, pus, and blood in stool.
- Bacterial or parasitic infections: Pathogens like Salmonella, Shigella, or C. difficile trigger immune responses that increase mucus.
- Intestinal obstruction: Partial blockages can cause mucus buildup behind the site of obstruction.
- Colorectal cancer: While rare as an isolated symptom, persistent mucus with unexplained weight loss or changes in bowel habits requires evaluation.
“While occasional mucus is normal, consistent visibility—especially with pain, bleeding, or weight loss—warrants investigation.” — Dr. Lena Patel, Gastroenterologist, Cleveland Clinic
Color and Consistency: What They Reveal
The appearance of mucus provides clues about its origin and significance. Use this guide to interpret what you see:
| Appearance | Possible Meaning | Action Recommended |
|---|---|---|
| Clear or white, small amount | Normal physiological mucus | No action needed |
| Yellow or green mucus | Possible infection or IBD | Monitor; consult if persistent |
| Streaked with red or maroon | Blood mixed with mucus—could be hemorrhoids, IBD, or polyps | Seek medical evaluation |
| Large amounts, jelly-like | Parasitic infection (e.g., amoebiasis) or IBS-D | See a doctor for testing |
| Associated with severe cramping | Acute infection or inflammatory condition | Urgent assessment advised |
Mini Case Study: Recognizing a Chronic Condition
Sarah, a 34-year-old teacher, began noticing slimy, pale-yellow streaks in her stool after a bout of food poisoning. At first, she assumed it was residual irritation. But over three months, the mucus persisted and was accompanied by abdominal cramps and urgent diarrhea. She also reported fatigue and unexplained joint pain.
After visiting her primary care physician, Sarah was referred to a gastroenterologist. A colonoscopy revealed inflammation in her colon consistent with ulcerative colitis. Early recognition of persistent mucus helped lead to a timely diagnosis and effective treatment plan involving medication and dietary adjustments. Today, Sarah manages her condition well and rarely sees mucus in her stool.
Her experience underscores the importance of tracking symptoms beyond isolated incidents and seeking help when patterns emerge.
Step-by-Step Guide: What to Do If You Notice Mucus
If mucus appears in your bowel movements, follow this practical timeline to determine next steps:
- Day 1–3: Observe and document – Note frequency, color, and any accompanying symptoms (pain, fever, blood, diarrhea).
- Days 4–7: Evaluate diet and stress – Eliminate potential triggers like spicy foods, dairy, or high-FODMAP items. Stay hydrated.
- Week 2: Monitor persistence – If mucus continues beyond a week despite lifestyle adjustments, consider a doctor visit.
- Week 3+: Seek professional evaluation – Especially if symptoms worsen or include weight loss, fever, or bloody stool.
- Testing phase – Your doctor may order stool tests, blood work, or endoscopic exams to rule out infection or IBD.
Checklist: When to See a Doctor About Mucus in Stool
Use this checklist to assess whether medical consultation is necessary:
- ☑ Mucus persists for more than two weeks
- ☑ Mucus is bloody, dark, or foul-smelling
- ☑ You experience unexplained weight loss
- ☑ Abdominal pain or cramping accompanies bowel movements
- ☑ Diarrhea or constipation lasts over seven days
- ☑ Family history of IBD or colorectal cancer
- ☑ Fever, fatigue, or joint pain develops
Frequently Asked Questions
Is it normal to have mucus in stool every day?
A tiny amount of clear or white mucus daily is normal. However, consistently visible mucus—especially if clumpy, colored, or increasing—is not typical and should be evaluated.
Can dehydration cause mucus in stool?
Indirectly, yes. Dehydration leads to harder stools that can irritate the colon lining, triggering increased mucus production as a protective response.
Does IBS cause mucus without blood?
Yes. Irritable bowel syndrome commonly presents with mucus in stool, particularly in the diarrhea-predominant type (IBS-D). Blood should never be considered a normal part of IBS and requires further investigation.
Conclusion: Listen to Your Body, Act with Confidence
Mucus in bowel movements ranges from a routine bodily function to a potential warning sign. The key lies in context—how much, how often, and what else is happening in your body. Most episodes are fleeting and benign, especially when tied to diet or minor illness. But when mucus becomes a regular companion to your bathroom visits, it’s time to listen closely.
Early awareness and proactive communication with a healthcare provider can make all the difference in managing both temporary discomfort and long-term conditions. Don’t minimize persistent changes. Your digestive health is a vital part of overall well-being—and paying attention today can prevent complications tomorrow.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?