Mucus is a slippery, colorless substance produced by the lining of the intestines to keep the colon moist and lubricated. A small amount of mucus in stool is normal and often goes unnoticed. However, when mucus becomes visible—appearing as jelly-like streaks or coating the stool—it can signal an underlying issue. While occasional mucus may not be cause for alarm, persistent or excessive amounts, especially when accompanied by other symptoms, should prompt further evaluation.
Understanding the causes, associated conditions, and warning signs can help you determine when mucus in stool is a minor digestive hiccup or a symptom requiring medical attention.
What Causes Mucus in Stool?
The digestive tract naturally produces mucus to protect the intestinal lining and aid in the smooth passage of stool. Increased visibility of mucus typically results from irritation, inflammation, or infection in the gastrointestinal (GI) tract. Common causes include:
- Irritable Bowel Syndrome (IBS): People with IBS often report increased mucus, especially during flare-ups involving diarrhea or constipation.
- Infections: Bacterial (e.g., Salmonella, Shigella), viral, or parasitic infections can inflame the gut lining, leading to excess mucus production.
- Inflammatory Bowel Disease (IBD): Conditions like Crohn’s disease and ulcerative colitis involve chronic inflammation of the GI tract, often resulting in mucus, pus, and blood in stool.
- Anal fissures or hemorrhoids: These conditions can cause mucus leakage due to irritation near the rectum.
- Dietary factors: Certain foods, artificial sweeteners, or food intolerances (like lactose intolerance) may trigger mucus production in sensitive individuals.
- Intestinal obstruction or polyps: Growths or blockages can stimulate localized mucus secretion.
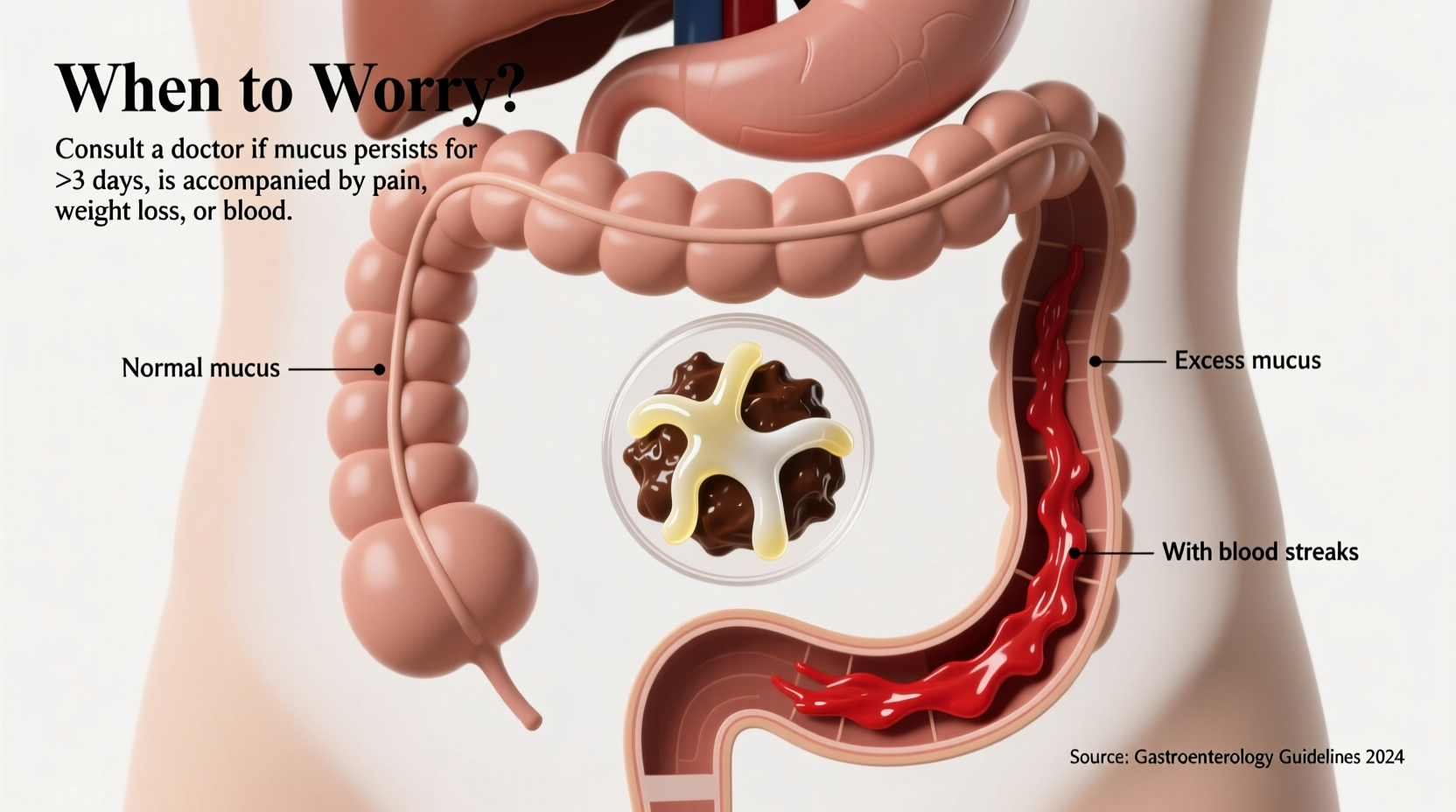
When Is Mucus in Stool a Cause for Concern?
Occasional, minimal mucus without other symptoms is usually harmless. However, certain red flags suggest a more serious condition. Seek medical advice if you experience:
- Consistent or increasing mucus over several days
- Blood or pus mixed with mucus
- Abdominal pain, cramping, or bloating
- Unexplained weight loss
- Fever or chills
- Diarrhea lasting more than two days
- Changes in bowel habits (e.g., alternating constipation and diarrhea)
“Visible mucus in stool isn’t always dangerous, but when combined with pain, bleeding, or systemic symptoms, it warrants investigation.” — Dr. Lena Patel, Gastroenterologist
Common Conditions Linked to Excess Mucus
Several digestive disorders are frequently associated with noticeable mucus in stool. Understanding these can guide early detection and management.
Inflammatory Bowel Disease (IBD)
Ulcerative colitis primarily affects the colon and rectum, causing ulcers that produce mucus, pus, and blood. Crohn’s disease can affect any part of the GI tract and may lead to mucus due to inflammation and fistulas.
Irritable Bowel Syndrome (IBS)
While IBS doesn’t cause structural damage, it alters bowel motility and sensitivity. Mucus is common, particularly in the diarrhea-predominant type (IBS-D).
Infections and Gastroenteritis
Bacterial or parasitic infections such as Campylobacter, Giardia, or C. difficile can inflame the intestinal lining, increasing mucus production. These are often accompanied by acute diarrhea, nausea, and fever.
Colorectal Cancer
Though rare as a sole symptom, persistent mucus—especially with blood, weight loss, or changes in stool caliber—can be an early sign of colorectal tumors. Polyps or malignant growths may secrete mucus or cause irritation.
| Condition | Typical Symptoms | Mucus Characteristics |
|---|---|---|
| IBS | Cramping, bloating, gas, alternating bowel habits | Clear or white, often stringy |
| Ulcerative Colitis | Bloody diarrhea, urgency, fatigue | Bloody mucus, frequent, urgent bowel movements |
| Gastroenteritis | Acute diarrhea, vomiting, fever | Watery stool with mucus, sudden onset |
| Hemorrhoids | Itching, pain, bleeding during bowel movements | Clear mucus on toilet paper or stool surface |
Step-by-Step: What to Do If You Notice Mucus in Stool
If you observe mucus in your stool, follow this practical timeline to assess whether intervention is needed:
- Day 1–2: Observe and record – Note the color, amount, and consistency of mucus. Track diet, bowel frequency, and any additional symptoms.
- Day 3–4: Evaluate for improvement – If mucus decreases and no new symptoms arise, it may have been temporary (e.g., from a mild infection or dietary change).
- Day 5+: Persistent or worsening symptoms – If mucus continues or worsens, especially with pain, blood, or fever, contact a healthcare provider.
- Seek immediate care if: You see significant blood, severe abdominal pain, high fever, or signs of dehydration (dizziness, dry mouth, reduced urination).
- Prepare for your appointment: Bring a symptom log, list of medications, and family history of GI conditions.
Mini Case Study: Recognizing Early Signs of Ulcerative Colitis
Sarah, a 34-year-old teacher, began noticing jelly-like mucus in her stool after a stressful work period. Initially dismissing it as stress-related, she later experienced urgency, cramps, and traces of blood. Over three weeks, symptoms worsened, affecting her sleep and daily routine. She visited a gastroenterologist who ordered a colonoscopy. The diagnosis was mild ulcerative colitis. With medication and dietary adjustments, Sarah regained control within two months. Her case highlights how early recognition of mucus—especially with other symptoms—can lead to timely treatment and prevent complications.
How to Support Gut Health and Reduce Mucus Production
While treating underlying conditions is essential, lifestyle and dietary choices play a key role in maintaining a healthy gut lining and minimizing irritation.
- Stay hydrated: Water helps maintain mucosal integrity and supports regular bowel movements.
- Eat fiber-rich foods: Fruits, vegetables, whole grains, and legumes nourish beneficial gut bacteria.
- Avoid processed foods and additives: Emulsifiers and preservatives in packaged foods may disrupt the gut barrier.
- Limit alcohol and caffeine: Both can irritate the GI tract and increase mucus secretion in sensitive individuals.
- Manage stress: Chronic stress impacts gut motility and immune function. Techniques like mindfulness, yoga, or breathing exercises can help.
“The gut is highly responsive to lifestyle. Even small, consistent changes in diet and stress reduction can significantly improve symptoms.” — Dr. Rafael Mendez, Integrative Medicine Specialist
FAQ
Is clear mucus in stool always a problem?
No. Small amounts of clear or white mucus are normal. It only becomes concerning if it’s frequent, increases in volume, or appears with pain, blood, or other symptoms.
Can food allergies cause mucus in stool?
Yes. Food sensitivities (e.g., to dairy, gluten, or soy) can trigger intestinal inflammation and mucus production. Elimination diets under medical supervision may help identify triggers.
Should I get a colonoscopy just for mucus in stool?
Not necessarily. A colonoscopy is typically recommended if mucus is persistent and accompanied by risk factors like age over 50, family history of colon cancer, or other GI symptoms. Your doctor will decide based on your full clinical picture.
Checklist: When to See a Doctor About Mucus in Stool
- ☑ Mucus present for more than 3–5 days
- ☑ Blood or pus in stool
- ☑ Abdominal pain or cramping
- ☑ Unexplained weight loss
- ☑ Fever or chills
- ☑ Change in bowel habits lasting over a week
- ☑ Personal or family history of IBD or colon cancer
Conclusion
Seeing mucus in your stool can be unsettling, but it’s not always a sign of something serious. The body uses mucus as a protective mechanism, and occasional visibility is normal. However, when mucus becomes a regular occurrence or appears with other troubling symptoms, it’s a signal to pay closer attention. By understanding the potential causes—from IBS and infections to more serious conditions like IBD or colorectal issues—you empower yourself to take timely action. Don’t ignore persistent changes in your bowel health. Early consultation with a healthcare provider can lead to accurate diagnosis, effective treatment, and long-term digestive wellness.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?