Muscle twitching—those sudden, involuntary flickers beneath the skin—is something nearly everyone experiences at some point. Often harmless and fleeting, these twitches can occur in the eyelid, calf, thumb, or even across the chest. While most are benign and resolve on their own, persistent or widespread twitching may signal underlying health concerns. Understanding what triggers muscle spasms and recognizing red flags can help you decide when to seek medical advice.
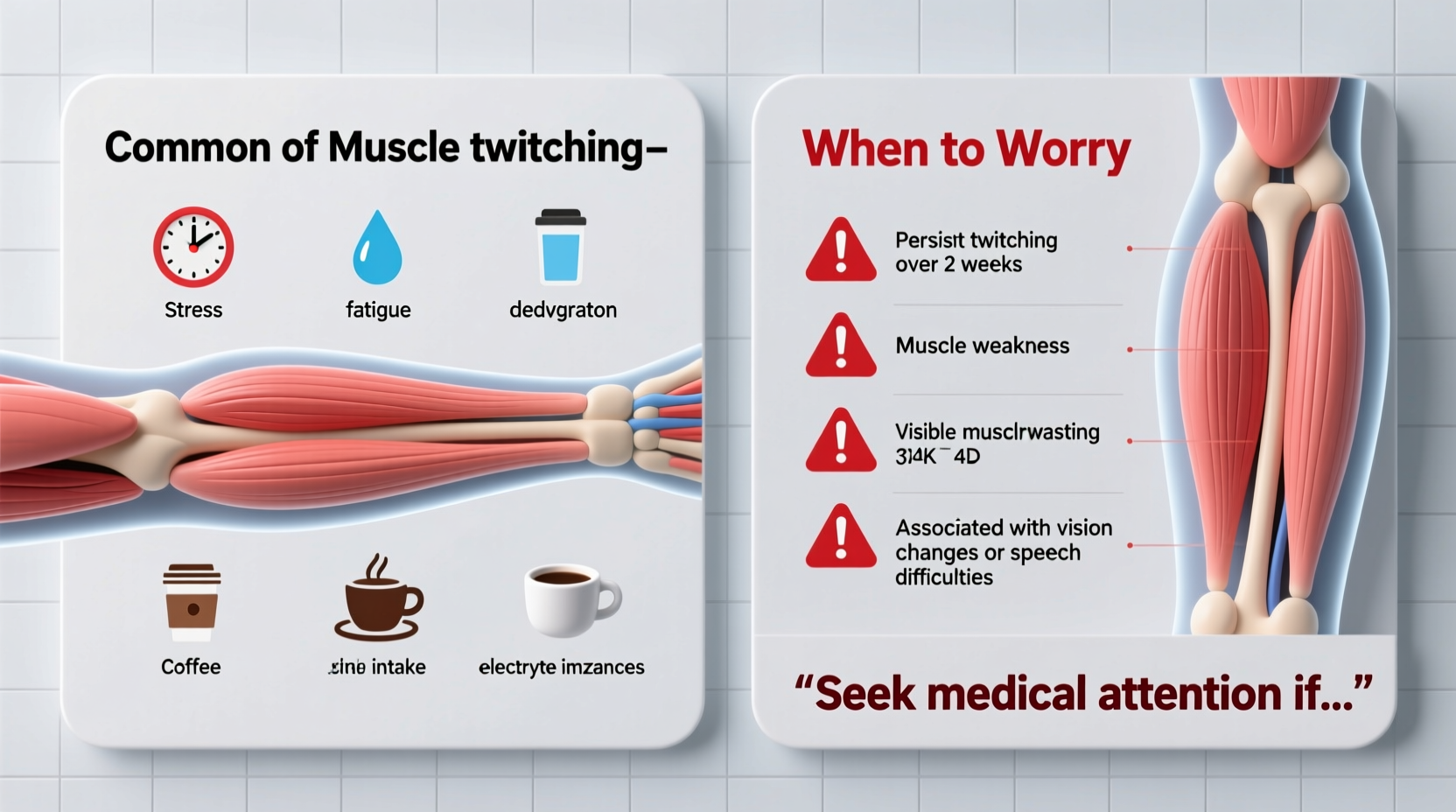
What Causes Muscle Twitching?
Muscle twitches, medically known as fasciculations, result from spontaneous contractions of small groups of muscle fibers. These contractions are triggered by nerve signals firing erratically. Although they’re usually temporary and painless, several factors can increase their frequency or duration.
- Stress and anxiety: Elevated cortisol levels affect nervous system function, increasing nerve excitability.
- Caffeine intake: High consumption of coffee, energy drinks, or stimulants can overstimulate motor neurons.
- Physical fatigue: Overuse of muscles during exercise or repetitive tasks leads to localized twitching.
- Sleep deprivation: Poor sleep disrupts electrolyte balance and neural regulation.
- Nutrient deficiencies: Low levels of magnesium, calcium, potassium, or vitamin D impair muscle and nerve function.
- Dehydration: Electrolyte imbalances reduce the threshold for nerve firing.
When Is Muscle Twitching Normal?
Benign fasciculation syndrome (BFS) accounts for many cases of chronic but non-dangerous twitching. It commonly affects otherwise healthy individuals and is often linked to stress, fatigue, or excessive stimulant use. Twitches in this category tend to be:
- Limited to one or two muscle groups
- Intermittent rather than constant
- Not accompanied by weakness, atrophy, or numbness
- Unchanged or improved with rest and hydration
For example, an office worker pulling late nights might develop eyelid twitching due to screen strain and poor sleep. Once they resume a regular sleep schedule and cut back on afternoon lattes, the twitching typically resolves within days.
Mini Case Study: Office Worker with Eyelid Twitching
Sarah, a 34-year-old project manager, began experiencing persistent left eyelid twitching after a high-pressure workweek. She was sleeping five hours per night, drinking three energy drinks daily, and skipping meals. After consulting her doctor, she was advised to improve sleep hygiene, reduce caffeine, and supplement with magnesium. Within ten days, the twitching stopped completely. No neurological abnormalities were found—her case exemplifies how lifestyle factors alone can trigger noticeable neuromuscular symptoms.
Red Flags: When to Worry About Muscle Twitching
While most twitching is harmless, certain patterns warrant medical evaluation. Persistent, spreading, or asymmetric muscle activity could indicate neurological conditions such as:
- Peripheral neuropathy
- Multifocal motor neuropathy
- Multiple sclerosis (MS)
- ALS (amyotrophic lateral sclerosis)
“Recurrent twitching without clear cause, especially when paired with weakness or muscle loss, should never be ignored. Early neurological assessment improves outcomes.” — Dr. Alan Reyes, Neurologist, Massachusetts General Hospital
Key warning signs include:
| Symptom | May Be Benign | Potential Concern |
|---|---|---|
| Duration | Seconds to minutes, occasional | Hours-long episodes or continuous |
| Location | Single area (e.g., eyelid) | Spreading to multiple limbs |
| Muscle strength | No change | Noticeable weakness or cramping |
| Atrophy | Absent | Visible muscle shrinkage |
| Progression | Stable or improving | Worsening over weeks/months |
Step-by-Step Guide to Managing and Evaluating Twitching
If you're experiencing muscle twitching, follow this structured approach to determine whether it's likely benign or requires further investigation:
- Track the pattern: Note when and where twitching occurs, its duration, and any triggers (e.g., after caffeine or intense workouts).
- Adjust lifestyle factors: Aim for 7–9 hours of sleep, reduce stimulants, stay hydrated, and eat balanced meals rich in electrolytes.
- Supplement wisely: Consider magnesium glycinate (200–400 mg/day) or a B-complex vitamin, especially if diet is inconsistent.
- Monitor for progression: If twitching persists beyond 2–3 weeks despite changes, consult a healthcare provider.
- Seek neurology referral if: You observe weakness, difficulty gripping objects, slurred speech, or muscle wasting.
Common Misconceptions About Muscle Twitching
One major misconception is equating all muscle twitching with ALS. While ALS does involve fasciculations, it almost always presents with additional symptoms such as progressive weakness, difficulty swallowing, or muscle atrophy. Isolated twitching without functional decline is extremely unlikely to be ALS.
Another myth is that twitching always indicates low calcium. While hypocalcemia can cause spasms, magnesium deficiency is far more common in otherwise healthy adults and often overlooked.
Checklist: What to Do If You Have Frequent Muscle Twitching
- ✅ Evaluate your caffeine and alcohol intake
- ✅ Assess sleep quality and duration
- ✅ Increase water and electrolyte-rich foods (bananas, spinach, nuts)
- ✅ Try magnesium supplementation under guidance
- ✅ Rule out medication side effects (e.g., corticosteroids, diuretics)
- ✅ Watch for new symptoms: weakness, numbness, coordination issues
- ✅ Schedule a doctor’s visit if twitching spreads or worsens
Frequently Asked Questions
Can dehydration cause muscle twitching?
Yes. Dehydration alters sodium, potassium, and magnesium levels, which are critical for normal nerve signaling. Even mild fluid deficits can trigger twitching, especially during or after exercise.
Is muscle twitching a sign of MS or ALS?
It can be—but only in combination with other neurological symptoms. ALS typically involves progressive muscle weakness and atrophy alongside twitching. MS-related twitching is less common and usually accompanied by vision problems, numbness, or balance issues. Isolated twitching is not diagnostic of either condition.
How long should I wait before seeing a doctor about muscle twitching?
If twitching lasts more than three weeks, spreads to multiple areas, or is associated with weakness, fatigue, or muscle loss, see a physician. Earlier evaluation is recommended if you have a family history of neurological disorders.
Conclusion: Know Your Body, Trust Your Instincts
Muscle twitching is overwhelmingly common and usually harmless. In most cases, simple adjustments to sleep, diet, and stress levels lead to resolution. However, the nervous system communicates through subtle signals—and persistent changes deserve attention. Don’t dismiss symptoms just because twitching is common, but also don’t panic at every flicker. Equip yourself with knowledge, track your symptoms objectively, and consult a professional when patterns suggest something deeper.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?