Muscle twitching in the arm—also known as fasciculations—is a surprisingly common experience. Most people have felt that sudden, involuntary flicker beneath the skin at some point. While often harmless, persistent or worsening twitches can sometimes signal an underlying health issue. Understanding the difference between routine muscle activity and symptoms requiring medical attention is crucial for peace of mind and timely care.
This article explores the most frequent causes of arm muscle twitching, identifies red flags that warrant concern, and offers practical guidance on managing and monitoring symptoms.
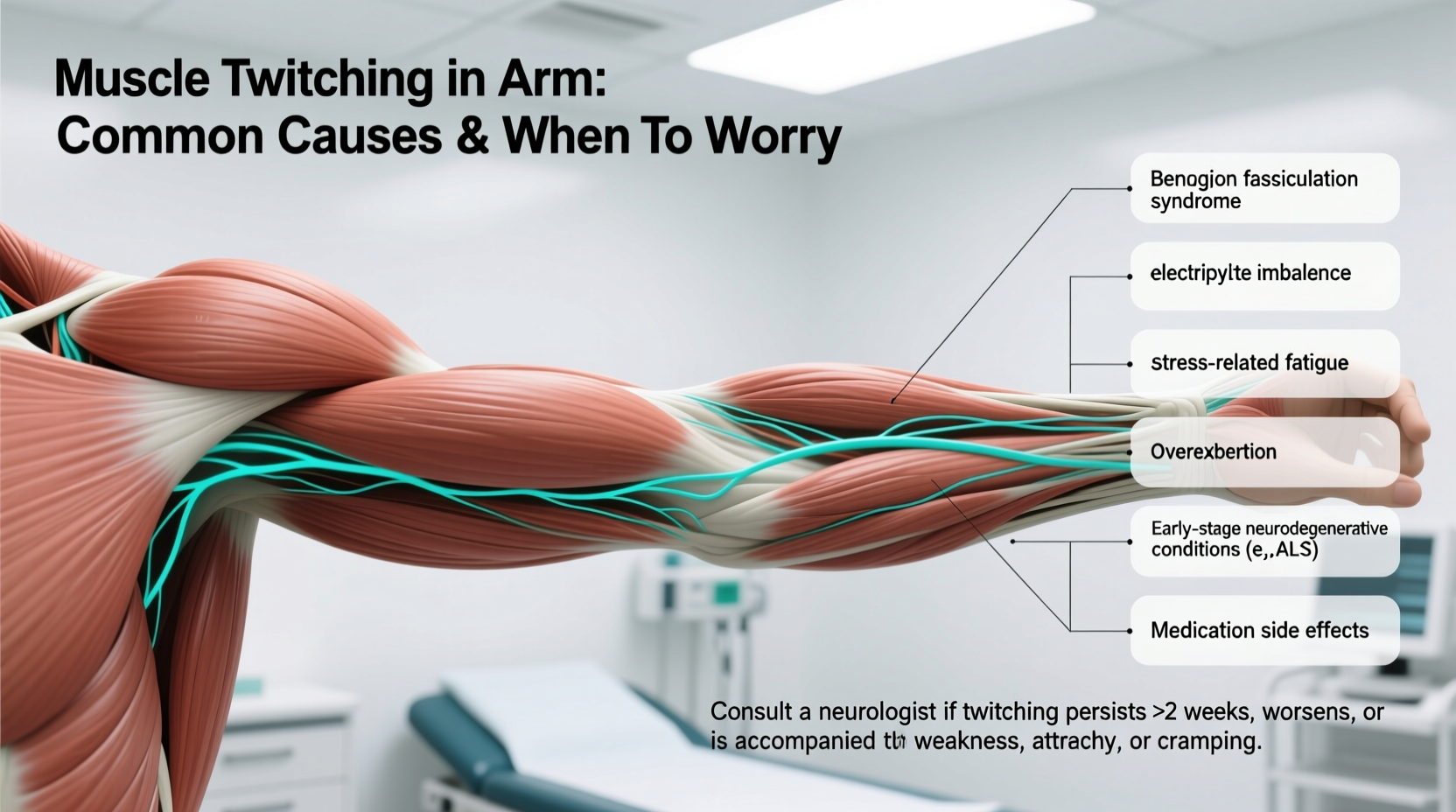
Common Causes of Arm Muscle Twitching
In most cases, muscle twitches in the arm are benign and temporary. They occur when small groups of muscle fibers contract spontaneously due to nerve signaling irregularities. These contractions are usually too weak to move the entire limb but are visible or palpable under the skin.
The following factors are among the most prevalent triggers:
- Stress and anxiety: Elevated cortisol levels from chronic stress can overstimulate the nervous system, leading to muscle irritability.
- Physical exertion: Intense or prolonged use of arm muscles, especially during weight training or repetitive tasks, may cause fatigue-related twitching.
- Caffeine and stimulants: Excessive intake of coffee, energy drinks, or certain medications can increase neuromuscular excitability.
- Sleep deprivation: Poor sleep disrupts electrolyte balance and nervous system regulation, contributing to spontaneous muscle activity.
- Nutritional deficiencies: Low levels of magnesium, calcium, potassium, or vitamin D impair normal muscle and nerve function.
- Dehydration: Fluid imbalance affects electrolyte concentrations, which are essential for proper nerve signaling.
When Muscle Twitching Is Not Normal: Warning Signs
While occasional twitching is typically nothing to worry about, certain patterns suggest the need for medical evaluation. Fasciculations become concerning when they are persistent, widespread, or accompanied by other neurological symptoms.
Red flags include:
- Twitching that lasts for weeks without improvement
- Spreading from one muscle group to others in the arm or body
- Visible muscle weakness or difficulty gripping objects
- Muscle atrophy (shrinking) noticeable over time
- Cramps that are severe or frequent
- Changes in coordination or fine motor skills
“Recurrent muscle twitching with weakness should never be ignored. It could indicate a motor neuron disorder like ALS, though far more commonly it’s related to stress or lifestyle factors.” — Dr. Alan Reyes, Neurologist, Massachusetts General Hospital
Differential Diagnosis: Conditions Linked to Persistent Twitching
Prolonged or progressive arm twitching may be associated with specific medical conditions. A healthcare provider evaluates these possibilities based on symptom history, physical examination, and diagnostic testing.
| Condition | Description | Associated Symptoms |
|---|---|---|
| Benign Fasciculation Syndrome (BFS) | Chronic muscle twitching without muscle damage or disease | Anxiety, fatigue, cramps; no weakness or atrophy |
| Peripheral Nerve Injury | Nerve compression (e.g., cubital or radial nerve) | Numbness, tingling, localized pain along nerve path |
| Multifocal Motor Neuropathy | Autoimmune condition affecting motor nerves | Progressive weakness, especially in hands; no sensory loss |
| Amyotrophic Lateral Sclerosis (ALS) | Neurodegenerative disease affecting motor neurons | Weakness, muscle wasting, difficulty speaking/swallowing |
| Thyroid Disorders | Hyperthyroidism increases metabolic and neuromuscular activity | Weight loss, rapid heartbeat, tremors, heat intolerance |
It's important to emphasize that ALS is extremely rare compared to benign causes. Most patients with isolated arm twitching do not have ALS, especially if there is no family history and no progression over several months.
Step-by-Step Guide to Assessing and Managing Arm Twitching
If you're experiencing muscle twitching in your arm, follow this structured approach to determine whether self-care is sufficient or professional help is needed.
- Track the pattern: Note when the twitching occurs, how long it lasts, and whether it spreads. Keep a journal for at least two weeks.
- Evaluate lifestyle factors: Assess caffeine intake, sleep quality, stress levels, hydration, and recent exercise routines.
- Adjust modifiable habits: Cut back on stimulants, aim for 7–8 hours of sleep, drink more water, and ensure balanced nutrition.
- Monitor for changes: Watch for new symptoms like weakness, numbness, or shrinking muscles.
- Consult a doctor if: Twitching persists beyond four weeks, worsens, or is accompanied by any red flag symptoms.
- Prepare for evaluation: Bring your symptom log to the appointment. Your doctor may order blood tests, EMG (electromyography), or nerve conduction studies.
Real-Life Example: When Lifestyle Changes Made the Difference
Mark, a 34-year-old software developer, began noticing frequent twitching in his right forearm after transitioning to remote work. He was drinking four cups of coffee daily, working late into the night, and rarely exercised. The twitching started intermittently but became nearly constant after three weeks.
Concerned, he consulted a neurologist who ruled out nerve compression and ALS through clinical assessment and EMG testing. Instead, Mark was diagnosed with stress-induced benign fasciculation syndrome. His doctor recommended reducing caffeine, establishing a regular sleep schedule, and incorporating magnesium supplements.
Within six weeks of making these changes, Mark’s twitching decreased significantly and eventually disappeared. His case illustrates how modern lifestyle pressures can manifest physically—and how targeted adjustments often resolve the issue without medication.
Frequently Asked Questions
Can dehydration cause muscle twitching in the arm?
Yes. Dehydration alters electrolyte levels such as sodium, potassium, and magnesium, all of which are critical for normal nerve-to-muscle communication. Even mild dehydration can trigger twitching, especially after exercise or in hot environments.
Is muscle twitching a sign of multiple sclerosis (MS)?
Not typically. While MS affects the central nervous system, it usually presents with sensory disturbances, vision problems, balance issues, or leg weakness—not isolated arm twitching. Fasciculations are more commonly linked to peripheral nerve or motor neuron conditions.
Should I see a neurologist for arm twitching?
You should consider seeing a neurologist if the twitching persists for more than a month, spreads to other areas, or is accompanied by weakness, atrophy, or functional impairment. For isolated, short-term twitching, primary care evaluation is often sufficient first.
Checklist: What to Do If You Experience Arm Twitching
- ✅ Monitor frequency and duration of twitching
- ✅ Reduce caffeine and alcohol intake
- ✅ Improve sleep hygiene (consistent bedtime, screen-free wind-down)
- ✅ Stay hydrated throughout the day
- ✅ Eat a balanced diet rich in magnesium (leafy greens, nuts, seeds) and potassium (bananas, potatoes, avocados)
- ✅ Manage stress through mindfulness, breathing exercises, or therapy
- ✅ Seek medical advice if twitching persists beyond 4 weeks or worsens
Conclusion: Listen to Your Body, But Don’t Panic
Muscle twitching in the arm is usually a fleeting and harmless occurrence tied to lifestyle factors like stress, fatigue, or diet. In the vast majority of cases, simple adjustments bring relief. However, persistent or progressive twitching—especially when paired with weakness or muscle loss—deserves medical attention to rule out neurological conditions.
By understanding the causes, recognizing warning signs, and taking proactive steps, you can respond wisely to your body’s signals. Don’t ignore persistent symptoms, but equally, don’t jump to worst-case conclusions without evidence.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?