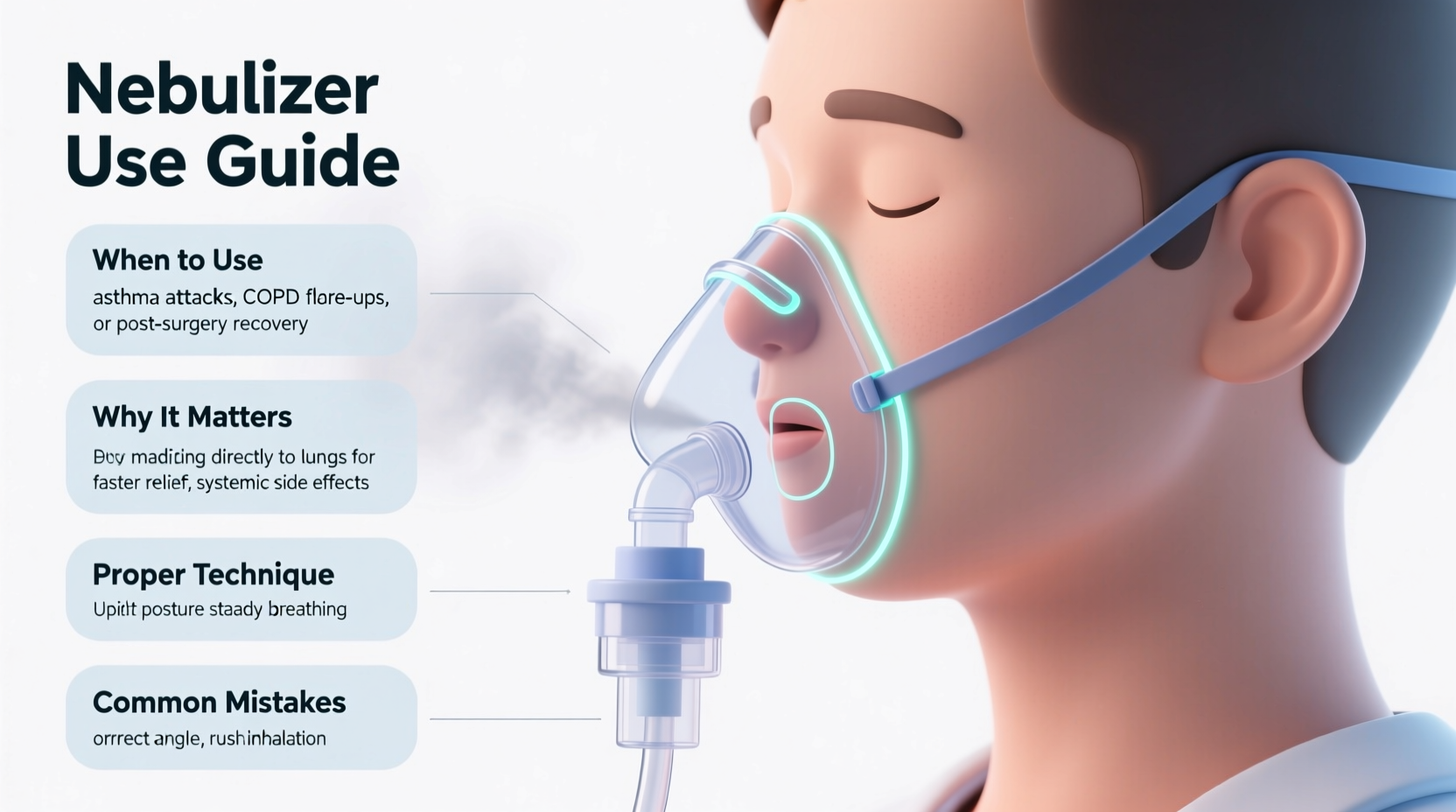
For individuals managing asthma, COPD, cystic fibrosis, or other chronic respiratory conditions, nebulizers are essential tools that deliver medication directly to the lungs in the form of a fine mist. While face masks are often used—especially with young children—the nebulizer mouthpiece is the preferred delivery method for most adults and older children. Understanding when and how to use it correctly can significantly impact treatment effectiveness, medication absorption, and long-term lung health.
Why the Mouthpiece Is the Preferred Option
The nebulizer mouthpiece delivers medication more efficiently than a face mask by ensuring a direct path from the device into the lungs. When you inhale through a mouthpiece, the aerosolized medicine travels straight down the trachea and into the bronchial tubes, minimizing loss to the surrounding air or deposition on facial skin and eyes.
Studies show that mouthpiece use results in up to 40% greater drug delivery to the lungs compared to masks. This means patients may achieve symptom relief faster and with lower doses, reducing the risk of side effects such as oral thrush or hoarseness linked to corticosteroid medications.
“Using a mouthpiece properly ensures deeper lung penetration and reduces systemic exposure to medication.” — Dr. Lena Torres, Pulmonologist and Respiratory Therapist Educator
When to Use a Nebulizer Mouthpiece
The decision to use a mouthpiece instead of a mask depends on age, coordination, and medical guidance. Here’s a breakdown of appropriate scenarios:
- Adults and children over 5 years old: Most can reliably seal their lips around the mouthpiece and breathe steadily through the mouth.
- Patients with facial hair or skin sensitivities: Masks may not seal well, leading to medication leakage. A mouthpiece avoids these issues.
- During acute flare-ups: Precise dosing via mouthpiece helps ensure adequate medication reaches constricted airways quickly.
- For maintenance therapy: Daily treatments benefit from consistent delivery methods, and mouthpieces support better technique over time.
Conversely, face masks remain necessary for infants, toddlers, or anyone unable to coordinate breathing with the device. However, even in these cases, transitioning to a mouthpiece as soon as developmentally feasible is strongly recommended.
Step-by-Step Guide to Proper Usage
Maximizing the benefits of your nebulizer treatment requires more than just attaching a mouthpiece. Follow this sequence for optimal results:
- Wash hands thoroughly before handling the nebulizer cup, tubing, or mouthpiece to prevent contamination.
- Assemble the device according to manufacturer instructions—attach the tubing to the compressor, connect the top piece with the mouthpiece, and add prescribed medication.
- Sit upright in a quiet space free from distractions. Avoid lying down, which restricts diaphragmatic movement.
- Place the mouthpiece between your teeth and close your lips tightly around it to create an airtight seal.
- Breathe slowly and deeply through your mouth. Inhale until your lungs feel full, then exhale gently. Avoid rapid, shallow breaths.
- Continue for the full duration (usually 5–15 minutes), pausing only if coughing occurs. Resume once breathing stabilizes.
- Rinse your mouth afterward, especially if using steroid-based medications, to reduce the risk of oral candidiasis.
- Clean the mouthpiece immediately after use with warm soapy water, rinse well, and allow to air-dry on a clean towel.
Common Mistakes That Reduce Effectiveness
Even with correct equipment, poor technique can undermine treatment. The following errors are frequently observed—and easily corrected:
| Mistake | Impact | Solution |
|---|---|---|
| Leaking seal (lips not closed) | Up to 30% medication loss | Practice lip closure; consider training with a mirror |
| Breathing through the nose | Medication deposits in nasal passages | Use a nose clip if needed; focus on mouth breathing |
| Shallow or rapid breathing | Reduced lung deposition | Use pursed-lip breathing: inhale 3 seconds, exhale 6 |
| Not cleaning the mouthpiece | Bacterial growth, infection risk | Wash daily; disinfect weekly with vinegar solution |
| Using while lying down | Incomplete inhalation, pooling in throat | Always sit upright during treatment |
Real-World Example: Improving Asthma Control
Carlos, a 34-year-old office worker with moderate persistent asthma, had been using a nebulizer with a face mask for years due to convenience. Despite daily treatments, he experienced frequent nighttime symptoms and required rescue inhalers 3–4 times per week.
During a routine pulmonology visit, his doctor noticed he was still using a mask despite being fully capable of using a mouthpiece. After switching to a mouthpiece and receiving coaching on slow, deep breathing techniques, Carlos reported significant improvement within two weeks. His nighttime awakenings dropped to once a month, and he reduced rescue inhaler use to less than twice weekly.
“I didn’t realize how much medicine I was wasting,” Carlos said. “Now I actually feel the medicine working deeper in my chest.”
Checklist: Are You Using Your Nebulizer Mouthpiece Correctly?
Use this quick checklist before each treatment to ensure maximum benefit:
- ✅ Washed hands before assembly
- ✅ Medication added correctly to nebulizer cup
- ✅ Sitting upright in a comfortable chair
- ✅ Lips sealed tightly around the mouthpiece
- ✅ Breathing in slowly and fully through the mouth
- ✅ Exhaling completely between breaths
- ✅ Completed full treatment duration
- ✅ Rinsed mouth after steroid medications
- ✅ Cleaned mouthpiece immediately post-use
Frequently Asked Questions
Can I use a mouthpiece if I have dentures?
Yes. Most people with dentures can use a mouthpiece effectively. Ensure a good lip seal and avoid biting down hard on the plastic tip. If discomfort occurs, consult your respiratory therapist for alternative options.
Is a mouthpiece better than an inhaler with a spacer?
Both are effective, but they serve different needs. Nebulizers with mouthpieces are ideal for high-dose medications, severe symptoms, or when coordination is difficult. Inhalers with spacers are faster and more portable. Your healthcare provider will recommend based on your condition and lifestyle.
What should I do if I start coughing during treatment?
Pause the session, take a few normal breaths, and resume once the cough subsides. Coughing can be a reaction to medication or rapid inhalation. Try slowing your breathing rate. If persistent, consult your doctor—adjustments to medication concentration or type may be needed.
Final Thoughts: Small Tool, Big Impact
The nebulizer mouthpiece may seem like a small, simple component of respiratory therapy—but its role is anything but minor. When used correctly, it enhances medication delivery, reduces waste, and supports better disease control. Whether you're managing a newly diagnosed condition or have relied on nebulized treatments for years, revisiting your technique can lead to meaningful improvements in comfort and outcomes.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?