A sudden or gradual swelling on one side of the vulva can be alarming. While it’s often due to benign, treatable conditions, it can sometimes signal an infection or a more serious underlying issue. Understanding the possible causes, recognizing associated symptoms, and knowing when to see a healthcare provider are essential for maintaining reproductive health and peace of mind.
The vulva includes the external genital organs—labia majora, labia minora, clitoris, and vaginal opening. Swelling limited to one side may point to localized irritation, trauma, infection, or cyst formation. Most cases resolve with proper care, but certain red flags warrant prompt medical evaluation.
Common Causes of One-Sided Vulvar Swelling
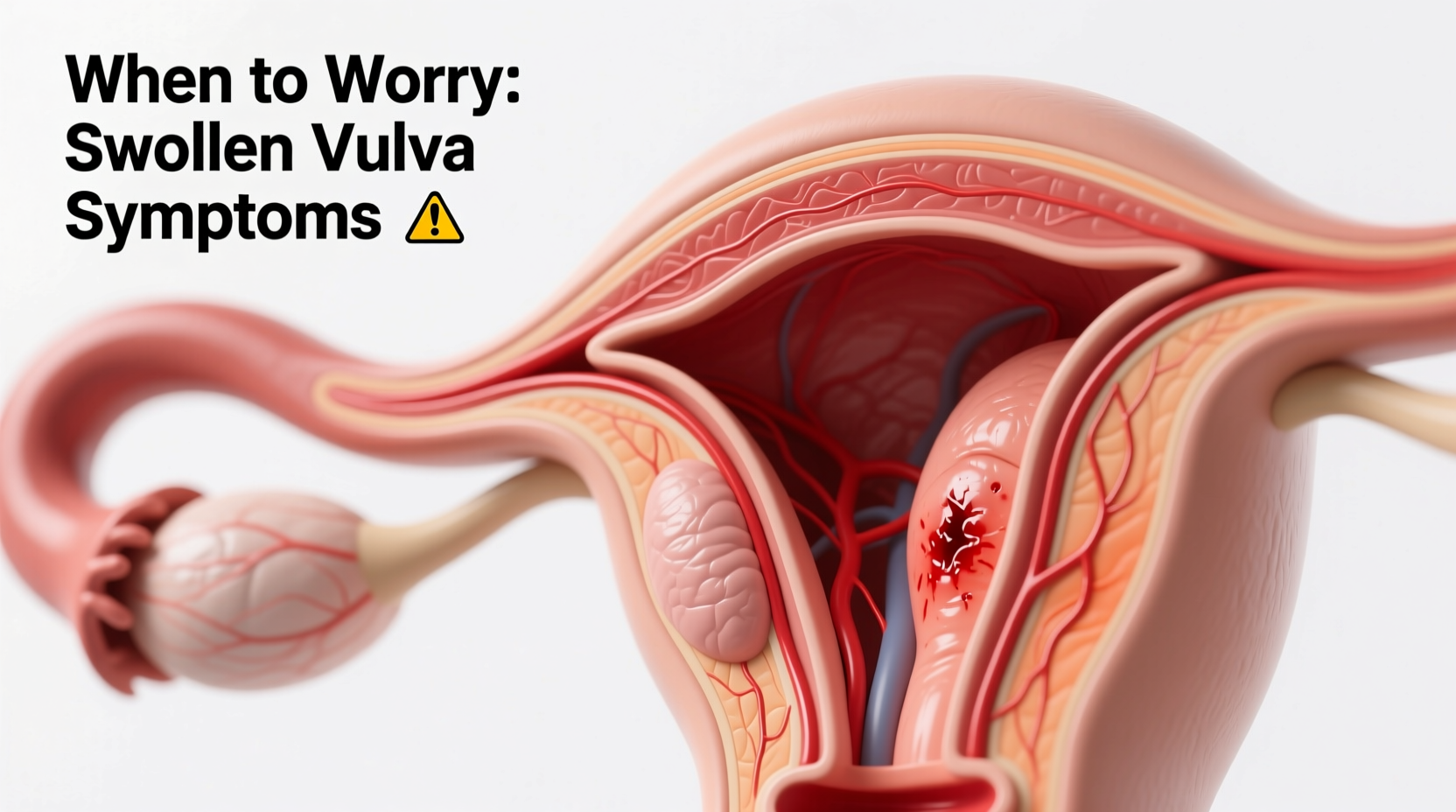
Swelling on one side of the vulva is rarely random. It typically stems from a physical or biological trigger affecting a specific area. The most frequent causes include:
- Bartholin’s cyst or abscess: The Bartholin’s glands, located near the vaginal opening, produce lubricating fluid. If the duct becomes blocked, a painless cyst can form. If infected, it turns into a tender, red, pus-filled abscess—often causing noticeable unilateral swelling.
- Skene’s duct cyst: Less common, but similar in mechanism, these small cysts arise near the urethra and may swell on one side.
- Folliculitis or ingrown hair: Shaving, waxing, or friction can cause inflammation of a hair follicle, leading to a small, painful bump that mimics swelling.
- Genital herpes (HSV-2): An initial outbreak may present as painful blisters, swelling, and tenderness on one side, often accompanied by flu-like symptoms.
- Bacterial vaginosis or yeast infection: While typically bilateral, severe inflammation from these infections can appear more pronounced on one side due to anatomical variation.
- Allergic reaction or contact dermatitis: Exposure to soaps, detergents, lubricants, or sanitary products can cause localized swelling, itching, and redness.
- Trauma or injury: Friction from sex, exercise, or tight clothing can lead to bruising or edema in one labial area.
- Benign growths or lipomas: Non-cancerous fatty lumps can develop slowly under the skin and may be mistaken for swelling.
Symptoms That Accompany Swelling
The nature of accompanying symptoms helps differentiate between minor irritation and conditions requiring treatment. Pay attention to:
- Pain or tenderness (mild vs. severe)
- Redness, warmth, or visible pus
- Itching or burning sensation
- Fever or chills (suggests systemic infection)
- Difficulty walking, sitting, or urinating
- Open sores, blisters, or ulcers
- Changes in vaginal discharge
- Swollen lymph nodes in the groin
For example, a Bartholin’s abscess typically causes throbbing pain, redness, and difficulty sitting. In contrast, an allergic reaction may produce intense itching without fever or pus. Herpes lesions often begin with tingling before progressing to painful ulcers.
“Unilateral vulvar swelling should never be ignored if it’s painful, worsening, or associated with fever. These signs suggest infection or obstruction needing clinical assessment.” — Dr. Lena Patel, OB-GYN Specialist
When to Worry: Red Flags and Warning Signs
Most cases of vulvar swelling are not emergencies, but some symptoms require urgent medical attention. Seek care promptly if you experience:
- Severe pain or rapid enlargement of the swollen area
- Fever above 100.4°F (38°C), indicating possible infection
- Pus drainage or foul odor from the site
- Inability to urinate or walk comfortably
- Open sores or ulcerations that don’t heal within a week
- Swelling persists beyond 3–5 days despite self-care
- History of sexually transmitted infections (STIs) or new sexual partner
Untreated abscesses can rupture spontaneously or spread infection. Delayed care for conditions like herpes or STI-related inflammation may increase transmission risk or lead to complications such as scarring or chronic pain.
Diagnosis and Medical Evaluation
A healthcare provider will perform a pelvic exam to assess the location, size, and characteristics of the swelling. They may also:
- Take a swab to test for STIs (e.g., gonorrhea, chlamydia, HSV)
- Check vaginal pH and discharge for signs of bacterial vaginosis or yeast
- Order blood tests if systemic illness is suspected
- Recommend ultrasound in rare cases to rule out deep tissue involvement or tumors
In postmenopausal individuals, any new vulvar mass requires thorough evaluation to exclude malignancy, although cancer is a rare cause of one-sided swelling.
Step-by-Step Guide to Initial Care at Home
For mild, non-painful swelling without fever or discharge, conservative measures may help reduce discomfort while monitoring progression:
- Apply warm compresses: Use a clean cloth soaked in warm water for 10–15 minutes, 3–4 times daily. This encourages drainage in cysts and soothes inflammation.
- Wear loose, breathable cotton underwear: Reduce friction and moisture buildup.
- Avoid irritants: Stop using scented soaps, douches, or fragranced laundry detergents.
- Practice gentle hygiene: Rinse with lukewarm water only; pat dry, don’t rub.
- Take over-the-counter pain relief: Ibuprofen or acetaminophen can ease discomfort.
- Monitor changes daily: Track size, color, pain level, and new symptoms.
If improvement occurs within 2–3 days, continued home care may suffice. Lack of improvement or worsening warrants a clinic visit.
Treatment Options Based on Cause
Medical treatment depends on the diagnosis:
| Condition | Treatment Approach | Notes |
|---|---|---|
| Bartholin’s cyst (small, asymptomatic) | Warm soaks, observation | May resolve without intervention |
| Bartholin’s abscess | Incision & drainage, possible Word catheter placement | Antibiotics if infection is confirmed |
| Herpes outbreak | Antiviral medication (e.g., acyclovir) | Reduces duration and severity |
| Bacterial vaginosis | Metronidazole or clindamycin | Oral or topical formulations |
| Yeast infection | Antifungal cream or oral fluconazole | Confirm diagnosis before use |
| Allergic dermatitis | Topical hydrocortisone, elimination of irritant | Avoid steroid creams long-term |
Mini Case Study: Recognizing an Abscess Early
Sophie, a 28-year-old teacher, noticed a tender lump on her right labia after a weekend hike. She initially dismissed it as chafing. Over two days, the area grew larger, redder, and extremely painful—especially when sitting. She developed a low-grade fever and felt unwell. Concerned, she visited her gynecologist, who diagnosed a Bartholin’s abscess. After minor surgical drainage and antibiotics, her symptoms resolved within a week. Sophie later realized that early warm compresses might have helped, but timely medical care prevented complications.
Her case illustrates how a seemingly minor issue can escalate quickly—and why monitoring symptoms matters.
Prevention Checklist
Reduce your risk of recurrent swelling with these practical steps:
- ✅ Practice safe sex and get regular STI screenings
- ✅ Use fragrance-free, hypoallergenic personal care products
- ✅ Avoid shaving too closely or frequently in the genital area
- ✅ Change out of wet swimsuits or workout clothes promptly
- ✅ Maintain good vulvar hygiene without over-cleaning
- ✅ Stay hydrated and support immune health through balanced nutrition
FAQ
Can a swollen vulva be a sign of cancer?
Rarely. Vulvar cancer usually presents as a persistent lump, ulcer, or area of thickened, discolored skin that doesn’t heal. It’s more common in older women and those with HPV history. Any lesion lasting longer than a few weeks should be evaluated.
Is it normal for one side to be larger than the other?
Yes. Natural asymmetry is common in vulvar anatomy. However, sudden or painful swelling differs from baseline anatomy and should be assessed if new or changing.
Can hormonal changes cause vulvar swelling?
Indirectly. Hormonal fluctuations during menstruation, pregnancy, or menopause can increase tissue sensitivity and fluid retention, potentially exacerbating existing irritation or cyst formation—but they rarely cause isolated swelling alone.
Conclusion
One side of vulva swollen—while unsettling—is often due to manageable conditions like cysts, infections, or irritation. Awareness of symptoms, timely self-care, and knowing when to seek help are key to effective resolution. Don’t downplay persistent pain, fever, or changes in appearance. Your body sends signals for a reason. Trust your instincts, prioritize your health, and consult a medical professional when in doubt.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?