Ozempic, generically known as semaglutide, has gained widespread attention not only for its effectiveness in managing type 2 diabetes but also for its role in significant weight loss. Marketed by Novo Nordisk, the injectable medication mimics a hormone that regulates blood sugar and appetite. While many patients report improved glycemic control and substantial weight reduction, growing concerns have emerged about its potential downsides. Like any powerful medication, Ozempic comes with a range of possible adverse effects—some mild, others serious. Understanding these risks is essential for anyone considering or currently using the drug.
Common Side Effects: What Most Users Experience
The most frequently reported side effects of Ozempic are gastrointestinal in nature. These typically occur during the initial weeks of treatment as the body adjusts to the medication.
- Nausea
- Vomiting
- Diarrhea
- Constipation
- Abdominal pain
- Decreased appetite
- Indigestion
These symptoms often subside over time, especially if the dosage is increased gradually. However, for some individuals, gastrointestinal discomfort persists and can significantly impact quality of life. Starting at a lower dose (0.25 mg weekly) and titrating slowly helps reduce the severity of these reactions.
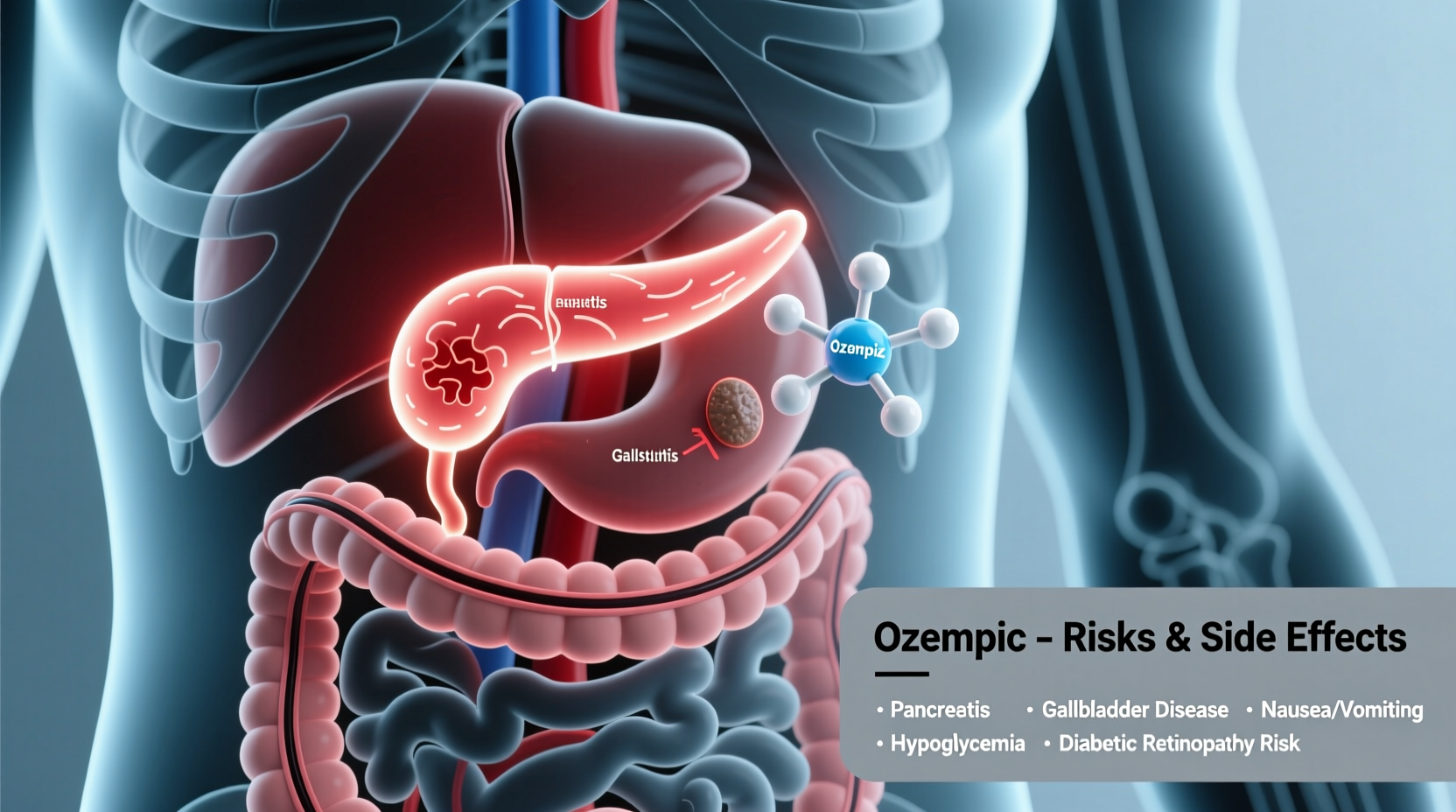
Serious Risks: Conditions That Require Medical Attention
Beyond common digestive issues, Ozempic carries several rare but severe risks. These require immediate medical evaluation and may influence whether the drug is appropriate for certain individuals.
Pancreatitis
Inflammation of the pancreas has been reported in clinical trials and post-marketing surveillance. Symptoms include persistent, severe abdominal pain that may radiate to the back, accompanied by vomiting. Patients with a history of pancreatitis should use Ozempic cautiously, if at all.
Thyroid C-Cell Tumors
Animal studies have shown an increased risk of thyroid C-cell tumors with semaglutide. While human relevance remains uncertain, the FDA mandates a black box warning: Ozempic should not be used in patients with a personal or family history of medullary thyroid carcinoma (MTC) or those with Multiple Endocrine Neoplasia syndrome type 2 (MEN 2).
“GLP-1 receptor agonists like Ozempic show remarkable metabolic benefits, but we must remain vigilant for rare but serious complications such as pancreatitis and potential thyroid malignancies.” — Dr. Alan F. Peppercorn, Endocrinologist, Boston Medical Center
Gallbladder Disease
Rapid weight loss, whether from surgery or medications like Ozempic, increases the risk of gallstones. Some users develop cholecystitis (inflamed gallbladder), sometimes requiring surgical removal. Symptoms include upper right abdominal pain, fever, and jaundice.
Hypoglycemia (Low Blood Sugar)
While Ozempic alone rarely causes hypoglycemia, the risk increases when combined with other diabetes medications like insulin or sulfonylureas. Signs include dizziness, sweating, confusion, and shakiness. Patients on combination therapy should monitor glucose levels closely.
Emerging Concerns: Gastroparesis and “Ozempic Belly”
One of the more controversial side effects linked to Ozempic is delayed gastric emptying, which can lead to gastroparesis—a condition where the stomach takes too long to empty its contents. While Ozempic intentionally slows digestion to promote fullness, in some cases, this effect becomes chronic and problematic.
Patients have reported ongoing nausea, bloating, early satiety, and reflux lasting months—even after discontinuing the drug. Social media is filled with anecdotal reports of “Ozempic belly,” describing persistent abdominal distension despite weight loss elsewhere.
Though definitive causal links are still under investigation, the FDA has acknowledged reports of gastrointestinal motility disorders in users of GLP-1 medications. A 2023 study published in *JAMA Internal Medicine* noted a higher incidence of gastroparesis among GLP-1 users compared to non-users, warranting further research.
Cardiovascular and Kidney Considerations
On a positive note, Ozempic has demonstrated cardiovascular benefits in patients with type 2 diabetes and existing heart disease, reducing the risk of major adverse cardiac events. However, fluid loss from vomiting or diarrhea can lead to dehydration, which may strain the kidneys—especially in older adults or those with pre-existing renal conditions.
Dehydration can result in acute kidney injury, particularly if oral intake is poor. Patients are advised to maintain adequate fluid intake and monitor for signs of dehydration: dry mouth, reduced urination, dizziness, or fatigue.
Psychological and Lifestyle Impacts
While not a direct pharmacological side effect, the rapid weight loss associated with Ozempic can have psychological consequences. Some users report changes in body image, disordered eating patterns, or emotional dependence on the medication for self-worth.
Additionally, once treatment stops, many people regain weight quickly—sometimes surpassing their original weight. This rebound effect can lead to frustration, low motivation, and a cycle of starting and stopping the medication.
Mini Case Study: Sarah’s Experience with Ozempic
Sarah, a 47-year-old teacher with type 2 diabetes, started Ozempic to improve her blood sugar control. Within three months, she lost 25 pounds and felt energized. But by month five, she began experiencing severe nausea and bloating after meals. Despite lowering her dose, symptoms persisted. An endoscopy revealed delayed gastric emptying consistent with gastroparesis. After discontinuing Ozempic, it took nearly six months for her digestive function to return to normal. Sarah now advocates for better patient education about long-term GI risks.
Who Should Avoid Ozempic?
Certain individuals should not use Ozempic due to heightened risks. The following table outlines contraindications and high-risk groups.
| Group | Reason to Avoid or Use Caution |
|---|---|
| History of medullary thyroid cancer or MEN 2 | Black box warning due to tumor risk in animal studies |
| Severe gastrointestinal disease (e.g., gastroparesis) | Ozempic can worsen motility issues |
| Pregnant or planning pregnancy | Not recommended; limited safety data |
| Children under 18 | Not approved for pediatric use |
| Individuals with a history of pancreatitis | May increase recurrence risk |
Step-by-Step Guide: Monitoring Your Health on Ozempic
- Start Low, Go Slow: Begin with the lowest dose (0.25 mg) for four weeks before increasing.
- Track Symptoms: Keep a daily log of nausea, bowel habits, appetite, and energy levels.
- Stay Hydrated: Drink water throughout the day, especially if experiencing vomiting or diarrhea.
- Schedule Regular Checkups: Visit your doctor every 3–6 months to assess kidney function, blood sugar, and overall well-being.
- Watch for Red Flags: Seek emergency care for severe abdominal pain, difficulty breathing, or signs of allergic reaction.
- Plan for Discontinuation: Discuss a tapering strategy with your provider if stopping the medication.
Frequently Asked Questions
Can Ozempic cause permanent digestive damage?
There is no conclusive evidence that Ozempic causes permanent damage in most people. However, cases of prolonged gastroparesis have been reported, and recovery can take months. Long-term effects are still being studied.
Is it safe to use Ozempic just for weight loss if I don’t have diabetes?
Ozempic is FDA-approved for type 2 diabetes, not obesity. For weight loss, the higher-dose version, Wegovy (also semaglutide), is approved. Using Ozempic off-label for weight loss is common but should be medically supervised due to risks.
What happens when you stop taking Ozempic?
Many people regain weight after stopping, especially if lifestyle changes aren’t maintained. Appetite returns, and metabolism may slow. Gradual tapering under medical supervision is recommended to manage symptoms and prevent sudden shifts in blood sugar.
Conclusion: Weighing Benefits Against Risks
Ozempic offers transformative benefits for many people with type 2 diabetes and obesity-related conditions. Yet, its growing popularity should not overshadow the real and sometimes serious risks involved. From gastrointestinal distress to rare but dangerous complications like pancreatitis and thyroid tumors, informed decision-making is crucial.
The key lies in personalized medicine—working closely with a healthcare provider to assess individual risk factors, monitor side effects, and adjust treatment as needed. Medication should complement, not replace, sustainable lifestyle changes.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?