Choosing between a Physician Assistant (PA) and a Nurse Practitioner (NP) isn’t just a matter of professional preference—it impacts education paths, clinical autonomy, scope of practice, and even patient care philosophy. As demand for advanced healthcare providers grows, understanding the distinctions between PAs and NPs becomes essential for aspiring clinicians, patients, and healthcare administrators alike. While both roles deliver high-quality medical care, their training models, licensing frameworks, and day-to-day responsibilities differ in meaningful ways.
Understanding the Core Models: Medical vs. Nursing
The fundamental difference between PAs and NPs lies in their educational foundation. PAs are trained under the medical model, similar to physicians. Their curriculum emphasizes disease pathology, diagnosis, and treatment through a biomedically focused lens. This model prioritizes standardized protocols and close collaboration with supervising physicians, although the degree of supervision varies by state.
In contrast, NPs follow the nursing model, which integrates disease management with a holistic emphasis on prevention, wellness, and patient education. Rooted in nursing theory, this approach often places greater focus on long-term health outcomes, patient advocacy, and continuity of care—especially in primary care settings.
“PAs are educated as generalists first, trained to adapt across specialties. NPs often specialize early, building deep expertise in areas like family health, pediatrics, or acute care.” — Dr. Linda Chen, Director of Clinical Education, Johns Hopkins PA Program
Education and Training Pathways Compared
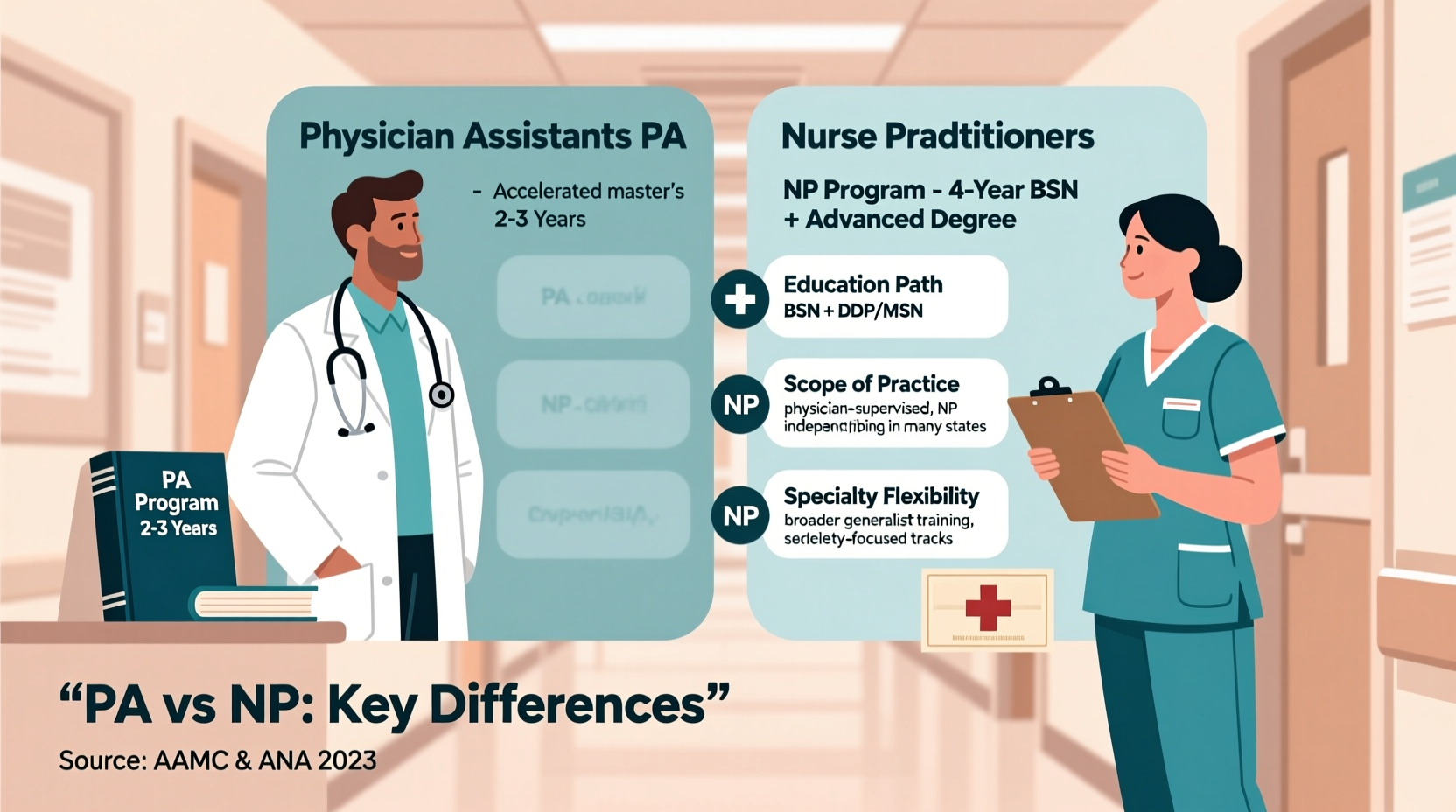
Becoming a PA typically requires a master’s degree from an accredited PA program, which takes about 27–30 months following a bachelor’s degree. Most applicants have prior healthcare experience—such as EMTs, paramedics, or medical assistants—and complete rigorous coursework in anatomy, pharmacology, and clinical medicine, followed by over 2,000 hours of clinical rotations across multiple disciplines including surgery, internal medicine, psychiatry, and emergency care.
NPs also earn a master’s or doctoral degree (MSN or DNP), but their path begins with a nursing degree (BSN). After becoming a registered nurse (RN), they pursue advanced training in a specific population focus—family, pediatric, psychiatric, etc. Clinical hours are concentrated within that specialty, resulting in deeper longitudinal experience in one area.
Scope of Practice and Autonomy
One of the most debated aspects of the PA vs. NP discussion is autonomy. In many states, NPs can practice independently, prescribe medications, and even open their own clinics without physician oversight. States like California, New York, and Texas still require collaborative agreements, but the national trend favors full practice authority for NPs.
PAs, on the other hand, are required by law to practice under a formal agreement with a supervising physician. However, this does not mean PAs are less capable. In practice, the supervisory relationship is often more about documentation than daily oversight. Many PAs function autonomously in rural or underserved areas while maintaining a legal collaborative link to a physician.
The key distinction is philosophical: PAs are trained as team-based providers who collaborate closely with physicians, whereas NPs are increasingly recognized as independent providers within the healthcare system.
Key Differences at a Glance
| Aspect | Physician Assistant (PA) | Nurse Practitioner (NP) |
|---|---|---|
| Educational Model | Medical model (physician-led) | Nursing model (patient-centered) |
| Entry Requirement | Bachelor’s + healthcare experience | BSN + RN license |
| Program Length | ~2.5 years (master’s) | 2–4 years (post-BSN) |
| Clinical Rotations | Broad, across multiple specialties | Focused within chosen population |
| Licensing Exam | PANCE (NCCPA) | Specialty-specific (e.g., FNP-BC) |
| Prescriptive Authority | Yes, in all states | Yes, with varying restrictions |
| Practice Autonomy | Requires collaborative agreement | Full practice authority in 27+ states |
| Specialty Flexibility | High—easy transitions between fields | Moderate—requires certification per specialty |
Why Choose a Physician Assistant?
Despite growing autonomy for NPs, many clinicians and healthcare systems continue to favor PAs for several strategic reasons. First, PAs are trained as generalists, making them highly adaptable. A PA working in dermatology can transition into cardiothoracic surgery with minimal retraining—a flexibility that benefits hospitals managing staffing needs across departments.
Second, the PA model aligns well with team-based care. In fast-paced environments like emergency medicine or surgical subspecialties, PAs integrate seamlessly into physician-led teams. Their training emphasizes rapid decision-making, procedural skills, and diagnostic acumen—all critical in acute care settings.
Third, for individuals who want to enter advanced practice faster, the PA route often offers a more direct path. Without needing to become an RN first, candidates can move straight from undergraduate studies into PA school, shortening the timeline to clinical practice.
Real-World Scenario: The Rural Health Clinic Dilemma
In a small clinic in Montana, administrators faced a staffing crisis. They needed someone who could manage chronic diseases, assist in minor procedures, and step in during emergencies. Two candidates applied: a Family Nurse Practitioner (FNP) and a PA with ER and internal medicine experience.
The FNP brought strong patient education skills and a history of managing diabetes and hypertension in community clinics. The PA offered broader procedural experience, including suturing, joint injections, and emergency stabilization. Ultimately, the clinic chose the PA because of their versatility and ability to support multiple providers across shifting demands.
This case illustrates a common reality: in dynamic or resource-limited settings, the PA’s generalist training and team-oriented mindset offer distinct advantages.
Step-by-Step Guide to Deciding Between PA and NP
- Assess your clinical interests: Do you prefer deep specialization (e.g., women’s health, pediatrics) or rotating across specialties?
- Evaluate your background: Are you already an RN? If so, the NP path may be more efficient. If not, PA school might be a faster entry point.
- Consider your desired work environment: Do you thrive in autonomous primary care roles or in collaborative, fast-paced specialty teams?
- Research state regulations: Check whether your target state allows full practice authority for NPs or requires supervision for PAs.
- Shadow both professionals: Spend time with a PA and an NP in different settings to observe their workflows and interactions.
- Reflect on philosophy: Are you driven by disease-focused treatment or holistic, preventive care?
Frequently Asked Questions
Can PAs specialize after graduation?
Yes. While PAs are trained as generalists, they commonly specialize through on-the-job training, fellowships, or postgraduate programs in areas like orthopedics, cardiology, or emergency medicine. Certification is not always required, though many pursue specialty credentials for career advancement.
Do PAs earn less than NPs?
Salaries are generally comparable, with median annual earnings between $120,000 and $135,000 depending on specialty and location. PAs in surgical subspecialties often earn more than NPs in primary care, but NPs in high-demand areas or with doctorates may match or exceed PA salaries.
Is PA school harder to get into than NP school?
Admission competitiveness varies, but PA programs typically have lower acceptance rates (around 20%) due to limited seats and high applicant volume. Most require significant hands-on patient care experience (2,000+ hours), making entry highly selective. NP programs often accept RNs with less direct experience, though top-tier programs remain competitive.
Final Considerations and Action Steps
The choice between becoming a PA or an NP should align with your personal values, career goals, and preferred model of care. Neither role is inherently superior—each fills vital niches in modern healthcare. PAs bring adaptability, procedural competence, and seamless integration into physician teams. NPs contribute deep patient relationships, preventive focus, and increasing independence in practice.
If you're considering a career in advanced practice, take concrete steps now: gain clinical experience, speak with mentors, and shadow providers in both roles. Attend informational sessions at PA and NP programs. Your decision doesn’t just shape your career—it influences how you’ll impact patients for decades to come.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?