Painful urination—also known medically as dysuria—is a symptom that affects millions of people each year, regardless of age or gender. While often dismissed as minor discomfort, it can signal underlying health conditions ranging from infections to chronic diseases. Recognizing the causes, associated symptoms, and knowing when to consult a healthcare provider is essential for timely treatment and prevention of complications.
Dysuria typically presents as a burning, stinging, or sharp sensation during or immediately after urination. For some, the pain may be mild and fleeting; for others, it can be severe enough to disrupt daily activities. Understanding what might be behind this discomfort empowers individuals to take informed action.
Common Causes of Painful Urination
The urinary tract is complex, and pain during urination can stem from various sources. The most frequent causes include infections, inflammation, irritants, and structural abnormalities.
- Urinary Tract Infections (UTIs): Bacterial infections in the bladder (cystitis) or urethra are among the leading causes, especially in women. Escherichia coli (E. coli) is the most common pathogen.
- Sexually Transmitted Infections (STIs): Chlamydia, gonorrhea, and herpes can cause urethral inflammation and painful urination, often accompanied by discharge or sores.
- Vaginal Infections: Yeast infections and bacterial vaginosis can irritate the external genital area, leading to discomfort during urination.
- Prostatitis: In men, inflammation of the prostate gland can result in painful urination, pelvic pain, and difficulty starting or maintaining a urine stream.
- Bladder Stones or Kidney Stones: As stones pass through the urinary tract, they can cause intense pain, including during urination.
- Chemical Irritants: Soaps, douches, spermicides, and certain laundry detergents may trigger irritation, particularly in sensitive individuals.
- Medications: Some drugs, like cyclophosphamide (used in chemotherapy), can irritate the bladder lining.
- Interstitial Cystitis (IC): A chronic condition causing bladder pressure, pain, and frequent, urgent urination without infection.
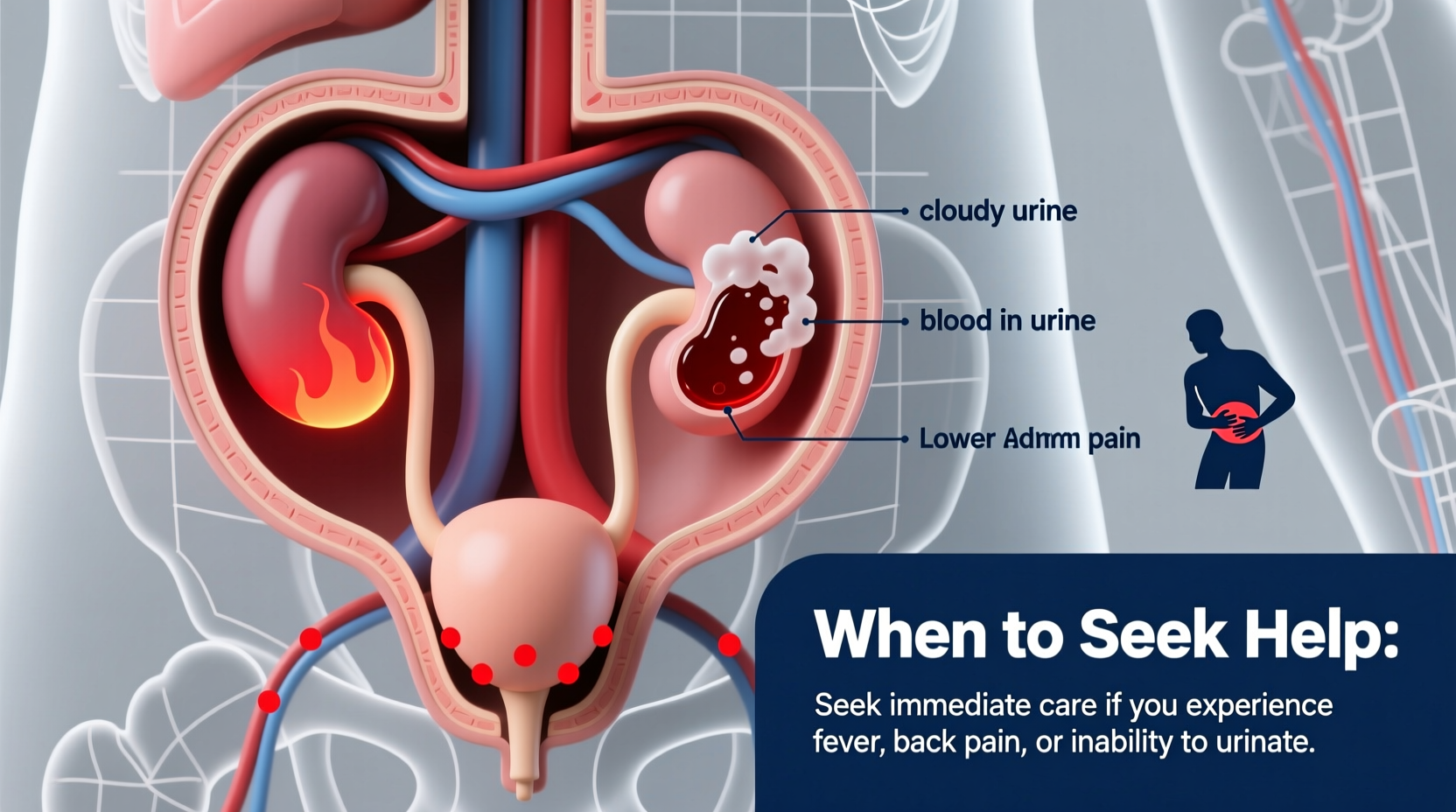
Symptoms That Accompany Painful Urination
While pain during urination is the primary symptom, it rarely occurs in isolation. Associated signs can help pinpoint the underlying cause:
- Frequent urge to urinate, even with little output
- Cloudy, dark, bloody, or foul-smelling urine
- Lower abdominal or pelvic pain
- Fever or chills (suggesting systemic infection)
- Genital discharge or sores
- Pain during sexual intercourse
- Difficulty starting or maintaining urine flow (especially in men)
In children, symptoms may be less specific. Look for increased crying during urination, new onset bedwetting, or unexplained irritability.
When to Seek Medical Help
Not every instance of painful urination requires emergency care, but certain red flags demand prompt medical evaluation. Delaying treatment can lead to complications such as kidney infections, infertility (in cases of untreated STIs), or chronic pelvic pain.
“Persistent dysuria, especially with fever or back pain, should never be ignored. It could indicate a kidney infection, which requires immediate antibiotics.” — Dr. Lena Patel, Urologist and Clinical Instructor at Boston Medical Center
Seek medical attention if you experience any of the following:
- Pain lasting more than 24–48 hours without improvement
- Fever above 100.4°F (38°C)
- Pain in the lower back or flank (indicative of kidney involvement)
- Blood in the urine (hematuria)
- Nausea or vomiting alongside urinary symptoms
- Known exposure to a sexually transmitted infection
- Pregnancy with new-onset urinary pain
High-Risk Groups Needing Immediate Evaluation
| Group | Risk Factors | Recommended Action |
|---|---|---|
| Pregnant individuals | Increased UTI risk; untreated infections can lead to preterm labor | See a provider within 24 hours |
| Men over 50 | Higher likelihood of prostate issues or obstruction | Urgent urological assessment |
| People with diabetes | Greater susceptibility to severe infections | Early testing and treatment |
| Children under 5 | UTIs may present atypically; risk of kidney damage | Pediatric evaluation required |
Diagnosis and Treatment Approaches
A healthcare provider will begin with a detailed history and physical exam. Diagnostic steps often include:
- Urinalysis: Tests for white blood cells, red blood cells, nitrites, and bacteria.
- Urine Culture: Identifies specific bacteria and guides antibiotic selection.
- STI Testing: Swabs or urine tests for chlamydia, gonorrhea, and other pathogens.
- Imaging: Ultrasound or CT scan if kidney stones or structural issues are suspected.
- Cystoscopy: In recurrent cases, a scope may examine the urethra and bladder lining.
Treatment depends on the diagnosis:
- Antibiotics for bacterial infections (UTIs, STIs)
- Antivirals for herpes-related dysuria
- Pain relievers and bladder-coating agents for interstitial cystitis
- Surgical intervention for stones or obstructions
Prevention Strategies and Daily Habits
While not all causes of painful urination are preventable, many risks can be reduced through consistent lifestyle choices.
📋 Prevention Checklist:- Drink 6–8 glasses of water daily
- Urinate soon after sexual activity
- Wipe front to back (especially in women)
- Avoid douching and scented feminine products
- Use condoms during sexual activity
- Wear cotton underwear and avoid tight-fitting pants
- Limit intake of bladder irritants (caffeine, alcohol, spicy foods)
Mini Case Study: Sarah’s Experience
Sarah, a 29-year-old teacher, began experiencing a burning sensation while urinating after a weekend trip. She initially assumed it was due to dehydration but noticed increasing urgency and cloudy urine over two days. By day three, she developed a low-grade fever and lower back pain. She visited her clinic, where a urinalysis confirmed a UTI with early signs of kidney involvement (pyelonephritis). Prompt antibiotic treatment prevented hospitalization. Her doctor emphasized hydration and post-sex voiding as preventive measures moving forward.
This case highlights how quickly a simple UTI can escalate—and why early intervention matters.
Frequently Asked Questions
Can stress cause painful urination?
Stress doesn’t directly cause dysuria, but it can worsen conditions like interstitial cystitis or weaken the immune system, making infections more likely. Stress-related muscle tension in the pelvic floor may also contribute to urinary discomfort.
Is painful urination always a sign of an infection?
No. While infections are common, other causes include chemical irritation, trauma, allergies, or chronic conditions like IC. A proper diagnosis requires clinical evaluation.
Can men get UTIs too?
Yes, though less common than in women. When men develop UTIs, they are more likely to have an underlying issue such as an enlarged prostate, kidney stones, or a structural abnormality requiring further investigation.
Take Control of Your Urinary Health
Painful urination is more than just a temporary annoyance—it’s your body’s way of signaling that something needs attention. Whether it’s a simple irritation or a sign of a deeper issue, listening to your symptoms and acting promptly can prevent long-term consequences. Don’t normalize discomfort. Stay hydrated, practice good hygiene, and seek medical advice when needed. Your urinary health is a vital part of your overall well-being.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?