Suddenly feeling your heart race, flutter, or pound unexpectedly can be alarming—especially when the sensation doesn’t go away. While occasional palpitations are common and often harmless, persistent or prolonged episodes may signal an underlying health issue. Understanding what might be causing your symptoms, how they’re evaluated by medical professionals, and when it’s time to take action can make a critical difference in your long-term well-being.
Palpitations that won’t stop can stem from a range of factors, including lifestyle habits, emotional stress, or more serious cardiac conditions. The key is not to panic—but also not to ignore the signs. This guide breaks down the science behind persistent palpitations, outlines the diagnostic process, and helps you recognize red flags that demand immediate attention.
Common Causes of Persistent Palpitations
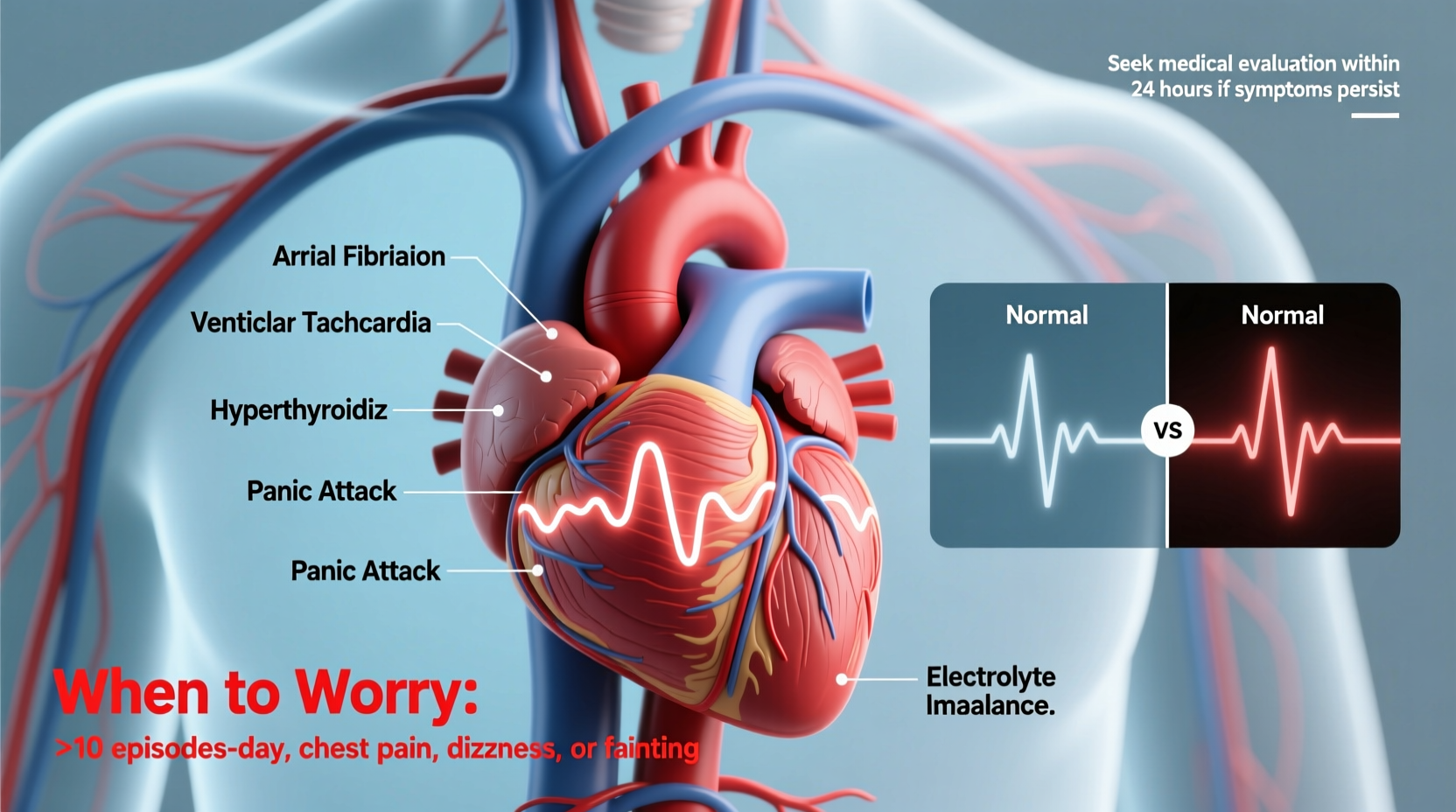
When your heart beats rapidly, skips a beat, or feels like it’s pounding out of rhythm for minutes—or even hours—it’s essential to consider potential triggers. Some causes are benign and reversible; others require prompt medical evaluation.
- Caffeine, nicotine, and stimulants: Coffee, energy drinks, tobacco, and certain medications (like decongestants) can overstimulate the nervous system, increasing heart rate and triggering palpitations.
- Anxiety and panic attacks: Emotional stress activates the body’s fight-or-flight response, releasing adrenaline that speeds up the heart. In some cases, this can create a feedback loop where the sensation of palpitations increases anxiety, which worsens the symptoms.
- Hormonal changes: Fluctuations during pregnancy, menstruation, perimenopause, or thyroid disorders (such as hyperthyroidism) can affect heart rhythm.
- Dehydration and electrolyte imbalances: Low levels of potassium, magnesium, or sodium disrupt the electrical signals that coordinate heartbeats.
- Arrhythmias: Conditions like atrial fibrillation, supraventricular tachycardia (SVT), or ventricular tachycardia cause abnormal heart rhythms that may persist without treatment.
- Heart disease: Structural issues such as valve problems, heart failure, or prior heart attacks increase the risk of sustained arrhythmias.
- Medications and supplements: Some asthma inhalers, antidepressants, and herbal products (e.g., ephedra, bitter orange) have cardiovascular side effects.
How Doctors Diagnose Persistent Palpitations
If your palpitations won’t stop or recur frequently, a healthcare provider will aim to determine whether the cause is cardiac or non-cardiac. Diagnosis typically involves a combination of patient history, physical examination, and targeted testing.
- Medical history review: Your doctor will ask about the frequency, duration, and pattern of your palpitations, along with associated symptoms like dizziness, chest pain, or shortness of breath.
- Physical exam: Listening to your heart, checking your pulse, and assessing blood pressure can reveal irregularities or signs of underlying conditions.
- Electrocardiogram (ECG/EKG): This quick test records your heart’s electrical activity. If done during an episode, it can identify specific arrhythmias.
- Event or Holter monitor: Since palpitations aren’t always present during a clinic visit, you may wear a portable ECG device for 24–48 hours (Holter) or up to 30 days (event monitor) to capture intermittent episodes.
- Echocardiogram: An ultrasound of the heart assesses structure and function, ruling out valve disease or weakened heart muscle.
- Blood tests: These check for anemia, thyroid dysfunction, electrolyte imbalances, or cardiac enzymes if a heart attack is suspected.
- Stress test: Monitoring your heart during exercise helps uncover rhythm issues triggered by physical exertion.
“Not all palpitations are dangerous, but persistent ones deserve investigation. We’ve diagnosed life-threatening arrhythmias in patients who initially dismissed their symptoms as stress.” — Dr. Lena Patel, Cardiologist, Massachusetts General Hospital
When to Worry: Red Flags That Require Immediate Attention
Most palpitations resolve on their own and are not emergencies. However, certain warning signs indicate a potentially serious condition requiring urgent care.
| Symptom | Possible Implication | Action Required |
|---|---|---|
| Chest pain or pressure | Possible heart attack or ischemia | Call emergency services immediately |
| Shortness of breath | Heart failure or pulmonary issue | Seek urgent evaluation |
| Dizziness or fainting | Low blood pressure or dangerous arrhythmia | Do not drive; get medical help now |
| Heart rate over 120 bpm at rest | Tachycardia, possibly SVT or AFib | Contact doctor or go to ER if prolonged |
| Symptoms lasting more than 30 minutes | Sustained arrhythmia | Seek medical assessment promptly |
Mini Case Study: Recognizing a Silent Threat
Sarah, a 42-year-old teacher, began experiencing heart flutters after switching to a new cold medication. At first, she assumed it was anxiety. But when the palpitations lasted over two hours and were accompanied by lightheadedness, she visited urgent care. An ECG revealed supraventricular tachycardia (SVT). After receiving intravenous adenosine, her rhythm normalized. Further testing showed no structural heart disease, but she was advised to avoid stimulant-containing medications. Sarah’s case highlights how seemingly minor triggers can unmask latent arrhythmias—and why timely evaluation matters.
What You Can Do: A Step-by-Step Guide to Managing Symptoms
If you're experiencing ongoing palpitations, taking structured steps can help clarify the issue and reduce risk.
- Stop and assess: Sit down, breathe slowly, and note the time. Check if you’ve recently consumed caffeine, alcohol, or taken new medications.
- Try vagal maneuvers: If you suspect SVT, techniques like bearing down (as if having a bowel movement) or applying cold water to your face may help reset your heart rhythm.
- Monitor your pulse: Count your heartbeats per minute. A consistently high rate (over 100 bpm at rest) warrants medical follow-up.
- Eliminate obvious triggers: Avoid caffeine, nicotine, alcohol, and stressful situations until symptoms resolve.
- Seek medical evaluation: Schedule an appointment with your primary care physician or cardiologist, especially if episodes are frequent or worsening.
- Follow through on testing: Complete recommended diagnostics to rule out serious conditions.
Frequently Asked Questions
Can dehydration cause palpitations that won’t stop?
Yes. Dehydration reduces blood volume and alters electrolyte balance, both of which can trigger or prolong palpitations. Rehydrating with water or oral rehydration solutions often helps relieve symptoms, especially after intense exercise or illness.
Is it safe to exercise if I have frequent palpitations?
It depends on the cause. Some arrhythmias are provoked by exercise and require caution. Others are better tolerated. Always consult your doctor before resuming or starting an exercise program if you experience recurrent palpitations.
Can anxiety mimic serious heart problems?
Absolutely. Panic attacks often include rapid heartbeat, chest tightness, and shortness of breath—symptoms that closely resemble heart conditions. However, only a proper medical evaluation can distinguish between psychological and cardiac causes. Never assume it’s “just anxiety” without being assessed.
Final Thoughts: Don’t Ignore What Your Heart Is Telling You
Your heart’s rhythm is a vital sign—one that communicates the state of your overall health. While many causes of persistent palpitations are manageable or temporary, dismissing them outright can be risky. Whether it's adjusting your lifestyle, managing stress, or undergoing a thorough cardiac workup, taking action protects your long-term heart health.
If your palpitations won’t stop, don’t wait for them to escalate. Track your symptoms, eliminate known triggers, and seek professional guidance. Early intervention can prevent complications and provide peace of mind.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?