For many women, the expectation is that menstrual cycles will become lighter and more predictable with age—especially as menopause approaches. However, a growing number report the opposite: their periods are becoming heavier, more painful, or irregular later in life. This shift can be alarming, disruptive, and at times debilitating. Understanding why this happens and knowing how to respond is crucial for long-term health and quality of life.
While some degree of change is normal due to hormonal fluctuations, worsening periods are not something to ignore. They may signal underlying conditions that require medical attention. This article explores the science behind increasingly difficult periods in midlife, outlines key causes, and provides practical steps for managing symptoms effectively.
Why Periods May Worsen After 35
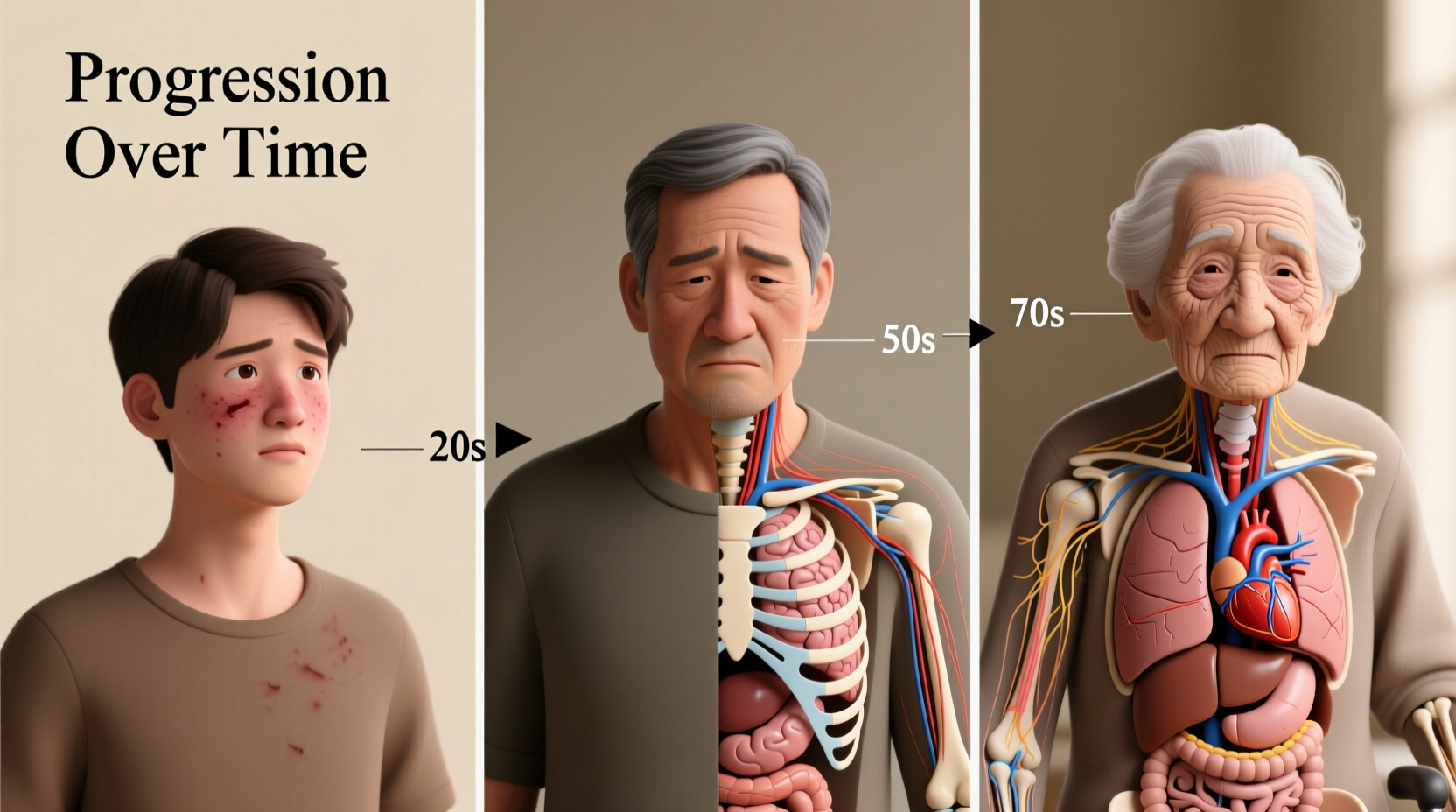
The reproductive system undergoes significant shifts starting in the late 30s and 40s, primarily due to perimenopause—the transitional phase leading up to menopause. During this time, estrogen and progesterone levels fluctuate unpredictably, disrupting cycle regularity and flow intensity. But hormonal changes alone don’t explain every case of worsening menstruation.
Several physiological and lifestyle-related factors contribute:
- Hormonal imbalance: Rising estrogen relative to progesterone can lead to a thicker uterine lining, resulting in heavier bleeding.
- Fibroids and polyps: These non-cancerous growths become more common with age and often cause heavy or prolonged periods.
- Endometriosis progression: Symptoms may intensify over time if left untreated.
- Weight gain: Increased body fat can elevate estrogen production, exacerbating menstrual flow.
- Thyroid disorders: Hypothyroidism is linked to heavier, longer periods.
- Medications: Blood thinners or certain antidepressants may increase bleeding.
Common Conditions Linked to Worsening Menstrual Symptoms
As women age, the risk of developing gynecological conditions increases. Many of these directly impact period severity.
Uterine Fibroids
Fibroids are muscular tumors in the uterine wall. Up to 70% of women develop them by age 50. While often asymptomatic, they can cause:
- Heavy menstrual bleeding (soaking through pads hourly)
- Pelvic pressure or pain
- Frequent urination
Adenomyosis
This condition occurs when endometrial tissue grows into the muscular wall of the uterus. It leads to an enlarged uterus, severe cramping, and heavy periods. Symptoms typically peak between ages 40–50.
Endometrial Polyps
Polyps are growths attached to the inner wall of the uterus. They can cause irregular bleeding and heavier flows. Risk increases with age, obesity, and high blood pressure.
Perimenopausal Hormonal Swings
Inconsistent ovulation during perimenopause means progesterone isn't released regularly. Without progesterone to balance estrogen, the endometrium builds excessively, then sheds erratically—leading to unpredictable, heavy bleeding.
“Many women assume worsening periods are just part of aging. But persistent heavy bleeding isn’t normal at any age and warrants evaluation.” — Dr. Linda Chen, OB-GYN and Reproductive Health Specialist
When to Seek Medical Help
Not all period changes require intervention, but certain red flags should prompt a visit to your healthcare provider:
| Symptom | Action Needed? | Notes |
|---|---|---|
| Soaking through a pad or tampon every hour for 2+ hours | Yes – urgent | Possible hemorrhage; could indicate fibroids or coagulation disorder |
| Periods lasting longer than 7 days | Yes | May lead to iron deficiency anemia |
| Severe pain interfering with daily activities | Yes | Could signal endometriosis or adenomyosis |
| Bleeding between periods or after sex | Yes | Requires ruling out polyps or cancer |
| Mild irregularity without excessive flow | Monitor | Common in perimenopause; track for patterns |
Step-by-Step Guide to Managing Worsening Periods
If your periods are becoming more difficult, follow this structured approach to identify causes and reduce discomfort.
- Document Your Cycle: Use a calendar or app to log start/end dates, flow intensity, pain level (1–10), and associated symptoms like fatigue or bloating.
- Schedule a Gynecological Exam: Include a pelvic ultrasound to check for fibroids, polyps, or structural issues.
- Get Blood Work: Test for anemia (low hemoglobin), thyroid function (TSH), and hormone levels if indicated.
- Discuss Treatment Options: Based on diagnosis, consider medications, minimally invasive procedures, or lifestyle adjustments.
- Implement Daily Support Strategies: Focus on nutrition, stress reduction, and gentle exercise to stabilize hormones.
Effective Treatments and Lifestyle Adjustments
Treatment depends on the underlying cause, but several options offer significant relief.
Medical Interventions
- Hormonal IUD (e.g., Mirena): Reduces or stops heavy bleeding in up to 90% of users within 6 months.
- Oral Progesterone: Prescribed during perimenopause to regulate cycles and prevent endometrial overgrowth.
- GnRH Agonists: Temporarily shrink fibroids before surgery.
- Minimally Invasive Surgery: Hysteroscopic removal of polyps or myomectomy for fibroids.
- Endometrial Ablation: Destroys the uterine lining to reduce or eliminate future periods (not for those wanting future pregnancy).
Lifestyle Modifications
- Exercise Regularly: Moderate activity helps regulate hormones and reduce inflammation.
- Reduce Alcohol and Caffeine: Both can worsen breast tenderness and disrupt sleep during hormonal shifts.
- Manage Stress: Chronic stress elevates cortisol, which interferes with progesterone production.
- Optimize Sleep: Aim for 7–9 hours nightly. Poor sleep amplifies hormonal imbalances.
Nutritional Support
Diet plays a critical role in hormonal health. Prioritize:
- Omega-3 fatty acids (salmon, flaxseeds) to reduce inflammation
- Cruciferous vegetables (broccoli, kale) to support estrogen metabolism
- Whole grains for stable blood sugar and reduced insulin spikes
- Adequate hydration to prevent bloating and support circulation
Real-Life Example: Sarah’s Journey
Sarah, 46, had always experienced mild periods. Over two years, her cycles became erratic—sometimes skipping months, then returning with extreme heaviness. She once soaked through four super tampons in two hours and was diagnosed with iron-deficiency anemia during a routine check-up.
After an ultrasound revealed multiple fibroids and a thickened endometrial lining, her doctor recommended a hormonal IUD. Within three months, her bleeding decreased significantly. Combined with dietary changes and weekly yoga, Sarah regained energy and no longer feared her next cycle.
Her experience underscores the importance of early assessment. “I thought it was just aging,” she said. “But treatment gave me my life back.”
Checklist: What to Do If Your Periods Are Getting Worse
- ☑ Track your symptoms for at least two full cycles
- ☑ Schedule a gynecologist appointment
- ☑ Request a transvaginal ultrasound
- ☑ Ask for blood tests (CBC, TSH, ferritin)
- ☑ Evaluate treatment options based on diagnosis
- ☑ Adjust diet and exercise habits to support hormonal balance
- ☑ Consider therapy or mindfulness practices for stress management
Frequently Asked Questions
Can periods really get worse with age?
Yes. Although menopause eventually ends menstruation, the years leading up to it—perimenopause—often involve worsening symptoms due to hormonal fluctuations and increased risk of fibroids, polyps, or adenomyosis.
Is heavy bleeding dangerous?
Chronic heavy bleeding can lead to iron-deficiency anemia, causing fatigue, dizziness, and heart strain. In rare cases, acute hemorrhage requires emergency care. Always seek help if you’re soaking through protection quickly or feeling faint.
Will I need a hysterectomy?
Not necessarily. Most women find relief through less invasive treatments like hormonal IUDs, medication, or outpatient procedures. Hysterectomy is typically reserved for severe cases unresponsive to other therapies.
Take Control of Your Cycle and Your Health
Worsening periods are not an inevitable part of aging. While hormonal shifts are natural, debilitating symptoms are not. By paying attention to your body, seeking timely medical evaluation, and making informed choices about treatment and lifestyle, you can regain control and improve your well-being.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?