Cramps during your period are common, but what about the ones that linger or appear *after* your flow has stopped? Many women dismiss post-period cramps as normal, assuming they’re just an extension of menstrual discomfort. However, persistent or recurring pain after menstruation can signal underlying conditions that deserve attention. Understanding the causes, recognizing red flags, and knowing how to respond can make a significant difference in your reproductive health and daily comfort.
Why Do Cramps Occur After Your Period Ends?
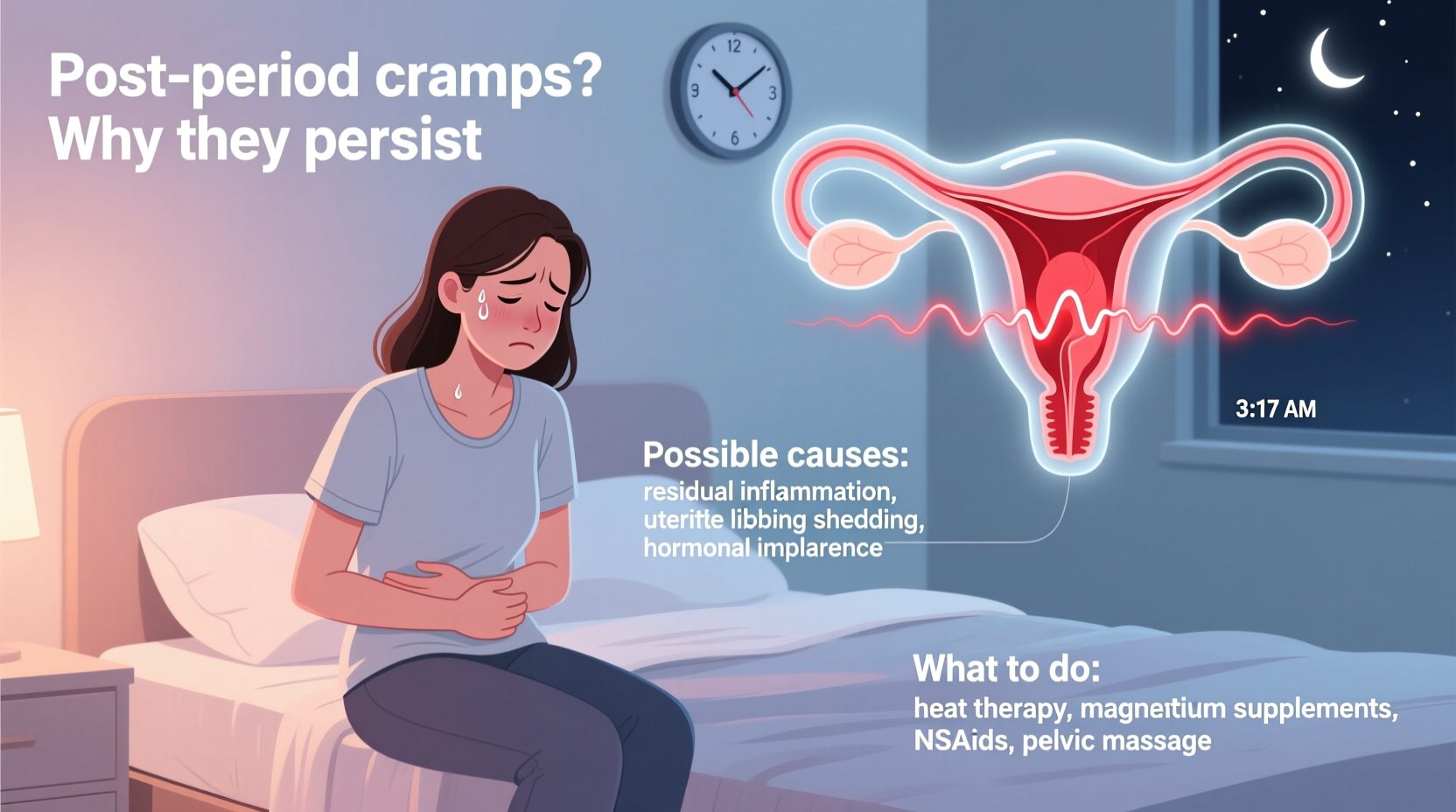
Menstrual cramps result from uterine contractions triggered by prostaglandins—hormone-like substances that help shed the uterine lining. While these typically subside as bleeding stops, some women continue to experience cramping due to physiological or pathological reasons.
One common cause is residual uterine activity. Even after menstruation, the uterus may continue contracting to expel any remaining tissue or regulate blood flow. These mild twinges are usually short-lived and not a cause for concern. However, if cramps intensify or persist beyond a few days, other factors may be at play.
Hormonal fluctuations don’t end with your period. The shift from the menstrual phase into the follicular phase involves changes in estrogen and progesterone levels, which can affect muscle tension and inflammation in the pelvic region. For some, this transition triggers discomfort resembling cramps.
Common Medical Causes of Post-Period Cramping
While occasional mild discomfort is normal, recurrent or severe post-period cramps may point to underlying gynecological conditions. Recognizing these can lead to earlier diagnosis and better management.
- Endometriosis: Tissue similar to the uterine lining grows outside the uterus, causing inflammation, scarring, and pain that often extends beyond menstruation.
- Adenomyosis: Endometrial tissue embeds into the muscular wall of the uterus, leading to heavy periods and deep, persistent cramping.
- Pelvic Inflammatory Disease (PID): Often caused by untreated infections like chlamydia or gonorrhea, PID leads to chronic pelvic pain, including after periods.
- Fibroids: Noncancerous growths in the uterus can cause pressure, bloating, and cramping at various points in the cycle.
- Ovulation Pain (Mittelschmerz): Some women feel one-sided lower abdominal pain around mid-cycle, which can be mistaken for post-period cramps.
“Persistent pelvic pain outside of menstruation should never be normalized. Conditions like endometriosis are frequently underdiagnosed because patients assume their pain is part of being a woman.” — Dr. Lena Torres, Gynecologist & Reproductive Health Specialist
When to Seek Medical Attention
Not all post-period cramps require urgent care, but certain symptoms warrant evaluation by a healthcare provider. Pain that interferes with daily activities, lasts more than two to three days after your period, or worsens over time should not be ignored.
| Symptom | May Be Normal | Warrants Medical Evaluation |
|---|---|---|
| Mild cramping lasting 1–2 days post-period | ✓ Yes | |
| Severe pain disrupting work or sleep | ✓ Yes | |
| Pain on one side only | Occasionally (ovulation) | If recurring or worsening |
| Fever or unusual discharge | ✓ Yes – possible infection | |
| Pain during intercourse or bowel movements | ✓ Yes – suggests endometriosis or adhesions |
Diagnostic Steps You Might Encounter
If you consult a doctor, expect a review of your menstrual history, a pelvic exam, and possibly imaging tests. Transvaginal ultrasound is commonly used to detect fibroids, cysts, or structural abnormalities. In cases where endometriosis is suspected, laparoscopy may be recommended for definitive diagnosis.
Natural and Medical Relief Options
Depending on the cause, treatment ranges from lifestyle adjustments to medical interventions. Start with conservative approaches, especially if your symptoms are mild.
Step-by-Step Guide to Managing Post-Period Cramps
- Apply Heat: Use a heating pad or hot water bottle on your lower abdomen for 15–20 minutes. Heat relaxes uterine muscles and improves blood flow.
- Stay Hydrated: Dehydration can increase muscle cramping. Drink plenty of water and herbal teas like chamomile or ginger.
- Try Anti-Inflammatory Foods: Incorporate omega-3-rich foods (salmon, flaxseeds), leafy greens, and berries while reducing processed sugars and trans fats.
- Practice Gentle Movement: Yoga poses like child’s pose or cat-cow stretch pelvic muscles and reduce tension.
- Consider Supplements: Magnesium, vitamin B1, and evening primrose oil have shown benefits in reducing menstrual-related pain.
- Use OTC Pain Relief: NSAIDs like ibuprofen block prostaglandin production, directly targeting cramp-causing chemicals.
- Consult a Specialist: If symptoms persist, schedule an appointment with a gynecologist for further evaluation.
Mini Case Study: Sarah’s Journey to Diagnosis
Sarah, a 32-year-old teacher, experienced cramps that started a few days after her period ended each month. She assumed it was normal until the pain began affecting her ability to teach. Over-the-counter painkillers provided minimal relief. After tracking her symptoms for three months, she noticed the pain coincided with bowel movements and sexual activity.
Her gynecologist ordered an ultrasound, which showed no fibroids, but based on her symptom pattern, referred her for a laparoscopy. She was diagnosed with stage III endometriosis. With hormonal treatment and minimally invasive surgery, Sarah’s post-period cramps resolved within six months. Her case underscores the importance of listening to your body and advocating for thorough evaluation.
Prevention Checklist
Use this checklist to reduce the likelihood and severity of post-period cramps:
- ✅ Track your cycle and symptoms monthly
- ✅ Maintain a balanced, anti-inflammatory diet
- ✅ Exercise regularly (even light walking helps)
- ✅ Manage stress through mindfulness or meditation
- ✅ Avoid smoking and excessive alcohol
- ✅ Schedule annual gynecological exams
- ✅ Seek help if pain disrupts your routine
Frequently Asked Questions
Can ovulation cause cramps after my period?
Yes. Ovulation typically occurs 10–14 days after your period starts and can cause mild to moderate cramping on one side of the lower abdomen. This pain, known as mittelschmerz, usually lasts a few hours to two days and is considered normal.
Is it normal to have cramps a week after my period?
Occasional mild discomfort may be due to ovulation or hormonal shifts. However, consistent or severe pain a week after your period should be evaluated, as it could indicate endometriosis, ovarian cysts, or other conditions.
Can birth control help with post-period cramps?
Yes. Hormonal contraceptives like combined oral pills, patches, or IUDs can regulate cycles, reduce prostaglandin production, and suppress conditions like endometriosis, significantly decreasing both menstrual and post-menstrual cramping.
Take Control of Your Pelvic Health
Post-period cramps aren’t something you must endure silently. While mild, short-lived discomfort can be part of your cycle, persistent or debilitating pain is not normal—and it’s not inevitable. By paying attention to your body, documenting symptoms, and seeking timely medical advice, you can uncover the root cause and access effective treatments. Whether through dietary changes, medication, or specialized care, relief is possible. Don’t let pain dictate your life. Prioritize your well-being, speak up about your symptoms, and take the first step toward lasting comfort.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?