Dizziness is a sensation that most people experience at some point in their lives. It can feel like spinning, lightheadedness, unsteadiness, or a sense of floating. While occasional dizziness may be harmless—triggered by standing too quickly or skipping a meal—recurrent or sudden episodes without clear cause should not be ignored. Understanding what drives random dizziness helps distinguish between benign triggers and potentially serious underlying conditions.
This article explores the most common causes of episodic dizziness, identifies red flags that warrant medical attention, and provides practical guidance on managing symptoms effectively.
Understanding the Types of Dizziness
Not all dizziness is the same. The way it presents often points to different origins:
- Vertigo: A spinning sensation, as if the room is moving. Often linked to inner ear issues.
- Lightheadedness: Feeling faint or woozy, typically due to blood pressure drops or dehydration.
- Disequilibrium: Loss of balance, especially when walking. Common in older adults or neurological conditions.
- Nonspecific dizziness: A vague feeling of disorientation or mental fogginess, sometimes tied to anxiety or medication side effects.
Pinpointing the type helps healthcare providers narrow down possible causes and recommend appropriate tests.
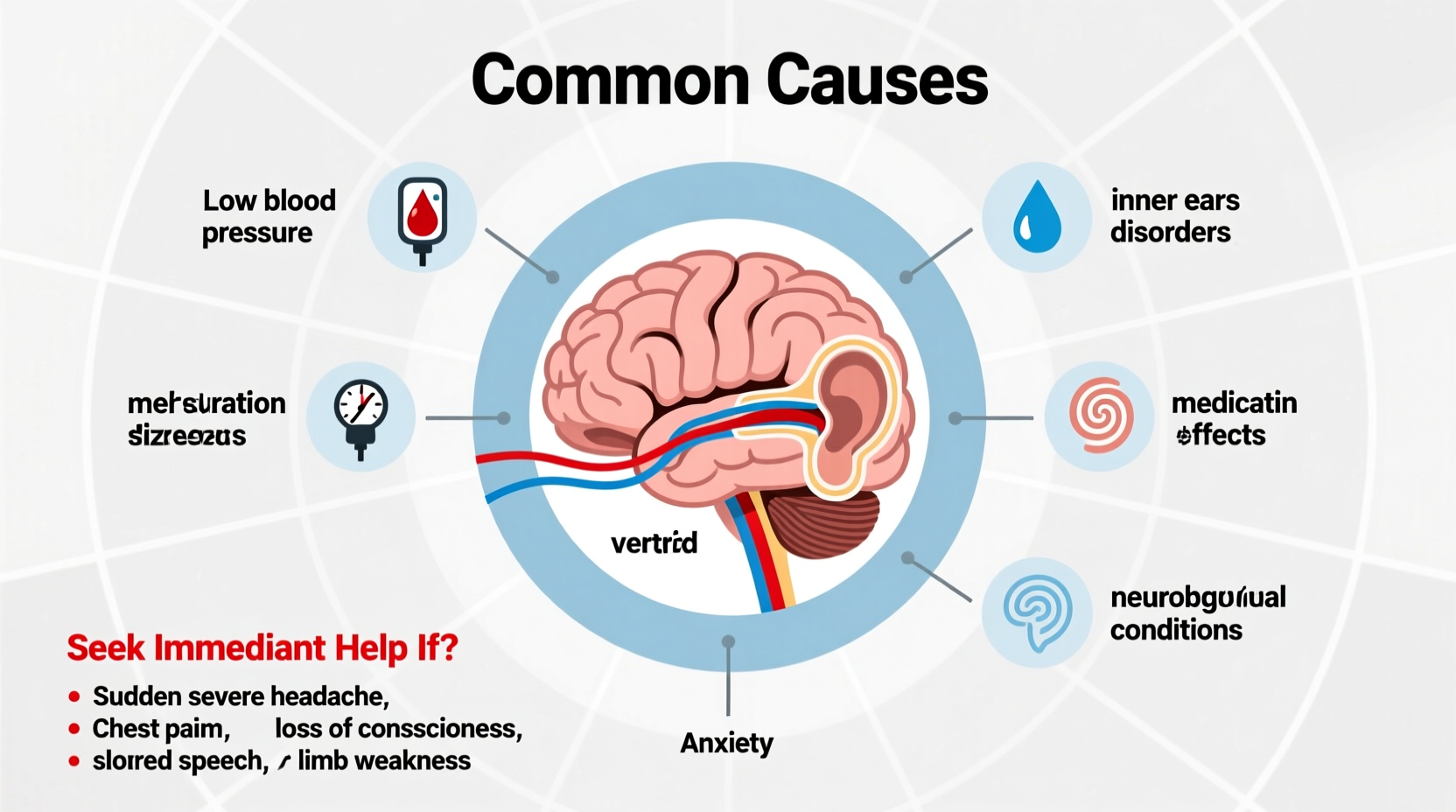
Common Causes of Random Dizziness
Episodic dizziness arises from a range of physiological and environmental factors. Below are the most frequent contributors:
Inner Ear Disorders
The inner ear plays a crucial role in balance. Conditions affecting this system often lead to vertigo:
- BPPV (Benign Paroxysmal Positional Vertigo): Triggered by changes in head position, such as rolling over in bed. Caused by displaced calcium crystals in the ear canals.
- Meniere’s Disease: Characterized by vertigo, hearing loss, tinnitus, and ear fullness. Episodes can last hours.
- Labyrinthitis or Vestibular Neuritis: Inflammation of the inner ear or vestibular nerve, often following a viral infection.
Cardiovascular Issues
Problems with blood flow to the brain can cause lightheadedness or near-fainting:
- Orthostatic Hypotension: A sudden drop in blood pressure upon standing. Common in older adults or those on blood pressure medications.
- Arrhythmias: Irregular heart rhythms reduce cardiac output, leading to inadequate brain perfusion.
- Reduced Blood Flow: Conditions like carotid artery stenosis or transient ischemic attacks (TIAs) may present with dizziness as an early sign.
Neurological Factors
While less common, certain neurological disorders contribute to imbalance:
- Migraine-Associated Vertigo: Dizziness occurring before, during, or after a migraine, even without head pain.
- Multiple Sclerosis: Can affect the central nervous system pathways involved in balance.
- Brainstem or Cerebellar Lesions: Tumors or strokes in these areas disrupt coordination and spatial awareness.
Medications and Toxins
Over 100 commonly prescribed drugs list dizziness as a side effect:
- Antihypertensives
- Antidepressants
- Sedatives and anticonvulsants
- Some antibiotics (e.g., aminoglycosides)
Alcohol, recreational drugs, and even excessive caffeine can also impair balance.
Psychological Triggers
Anxiety, panic attacks, and chronic stress frequently manifest physically:
- Hyperventilation reduces carbon dioxide levels, causing lightheadedness.
- Persistent worry can heighten bodily awareness, making normal sensations feel alarming.
In some cases, individuals develop chronic subjective dizziness—a condition where non-specific dizziness persists long after an initial trigger has resolved.
“Dizziness is one of the top three reasons adults visit primary care physicians. Yet, fewer than half receive a definitive diagnosis during the first consultation.” — Dr. Rebecca Nguyen, Neurotologist
When to Seek Medical Help: Red Flags
Most dizziness resolves on its own. However, certain symptoms indicate the need for prompt evaluation:
| Symptom | Possible Implication | Action Required |
|---|---|---|
| Sudden onset with severe intensity | Possible stroke or hemorrhage | Seek emergency care immediately |
| Chest pain or palpitations | Cardiac arrhythmia or heart attack | Call emergency services |
| Difficulty speaking, vision changes, limb weakness | Signs of stroke (especially posterior circulation) | Immediate ER evaluation |
| Fever, neck stiffness, confusion | Possible meningitis or encephalitis | Urgent hospital assessment |
| Progressive hearing loss with dizziness | Potential acoustic neuroma or Meniere’s disease | See ENT specialist |
If dizziness occurs more than once a week, interferes with daily activities, or lacks a clear trigger, schedule a visit with your doctor—even in the absence of red flags.
Step-by-Step Guide to Managing Episodic Dizziness
For mild or infrequent episodes, follow this timeline to assess and manage symptoms:
- Day 1–2: Document the Episode
- Note time, duration, triggers (e.g., standing, turning head), associated symptoms (nausea, hearing changes).
- Check medications and recent illnesses.
- Day 3–5: Implement Lifestyle Adjustments
- Stay hydrated; avoid alcohol and excess caffeine.
- Rise slowly from sitting or lying positions.
- Practice balance exercises (e.g., standing on one foot).
- Week 2: Try Targeted Maneuvers (if BPPV suspected)
- Perform the Epley maneuver under video guidance or physical therapist supervision.
- Reassess symptom frequency.
- After 2 Weeks: Consult a Healthcare Provider
- Request blood pressure monitoring, hearing test, or vestibular function assessment.
- Review medications for potential side effects.
Mini Case Study: Recognizing a Silent Stroke
Sarah, a 62-year-old teacher, began experiencing brief spells of dizziness when rolling over in bed. She dismissed them as fatigue-related. Over three weeks, episodes increased in frequency and were accompanied by mild slurring of speech and slight imbalance while walking. Her primary care physician referred her to neurology. An MRI revealed a small cerebellar infarct—likely a silent stroke. Prompt treatment with antiplatelet therapy and vascular risk management prevented further complications.
Sarah’s case illustrates how subtle dizziness, especially when progressive or combined with minor neurological signs, can signal a serious condition requiring urgent imaging and intervention.
Practical Checklist: What You Can Do Today
To better manage or prevent random dizziness, use this actionable checklist:
- ✅ Monitor blood pressure regularly, especially if on medication.
- ✅ Stay hydrated—aim for 6–8 glasses of water daily.
- ✅ Review all medications with your doctor for dizziness-inducing side effects.
- ✅ Practice slow transitions from lying to standing.
- ✅ Limit alcohol and avoid sedatives unless prescribed.
- ✅ Perform balance-strengthening exercises (e.g., tai chi or heel-to-toe walking).
- ✅ Keep a symptom diary tracking frequency, duration, and triggers.
- ✅ Schedule a hearing and vestibular evaluation if dizziness persists beyond two weeks.
Frequently Asked Questions
Can dehydration really cause dizziness?
Yes. Even mild dehydration reduces blood volume, lowering blood pressure and decreasing blood flow to the brain. This commonly results in lightheadedness, especially upon standing. Rehydrating with water or electrolyte solutions often resolves symptoms quickly.
Is it normal to feel dizzy during anxiety attacks?
Absolutely. During heightened anxiety, rapid breathing (hyperventilation) alters blood chemistry, reducing carbon dioxide levels and causing dizziness, tingling, and chest tightness. Grounding techniques and controlled breathing can help break the cycle.
Do I need an MRI for dizziness?
Not always. MRIs are typically reserved for cases with neurological deficits, progressive symptoms, or suspicion of structural brain abnormalities. Most patients are evaluated first with clinical exams, hearing tests, and possibly vestibular assessments.
Conclusion: Take Charge of Your Balance
Random dizziness is more than just a fleeting inconvenience—it can be a window into your overall health. While many causes are manageable with lifestyle adjustments or simple treatments, ignoring persistent or worsening symptoms risks missing serious underlying conditions. By understanding the triggers, recognizing danger signs, and taking proactive steps, you empower yourself to maintain stability and well-being.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?