Occasional eye twitching—those sudden, involuntary flutters of the eyelid—is something nearly everyone experiences at some point. While usually brief and harmless, persistent or worsening twitches can be unsettling. Understanding what triggers these spasms and recognizing when they might signal a more serious condition is key to managing them effectively.
Eye twitching, medically known as myokymia, typically affects the upper or lower eyelid of one eye. It may last seconds or recur over days, sometimes disappearing only to return later. Most cases resolve on their own without treatment. However, knowing the underlying factors—from lifestyle habits to neurological conditions—can help you take control before it escalates.
Common Causes of Eye Twitching
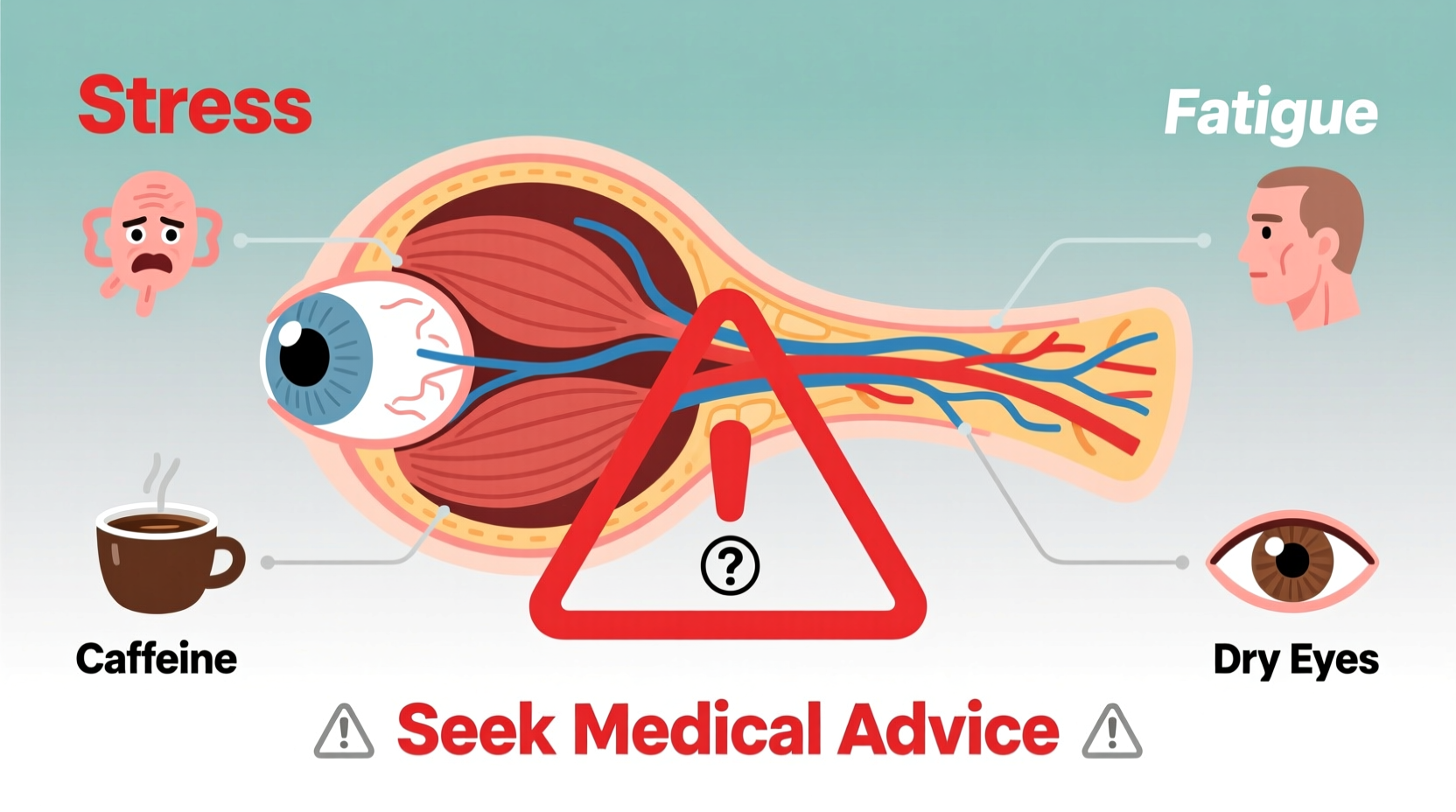
The majority of eyelid twitches are benign and linked to everyday stressors and behaviors. These temporary spasms occur when the nerves controlling the muscles around the eye fire erratically. The most frequent contributors include:
- Stress and anxiety: Elevated cortisol levels from emotional strain can increase muscle tension, including in the delicate facial muscles.
- Fatigue: Lack of quality sleep disrupts normal nerve function and lowers the threshold for muscle spasms.
- Caffeine intake: Excessive coffee, tea, energy drinks, or soda can overstimulate the nervous system.
- Dry eyes: Especially common with prolonged screen use, dryness irritates the eye surface and may trigger twitching.
- Nutritional imbalances: Deficiencies in magnesium, potassium, or calcium can affect nerve signaling.
- Eye strain: Extended focus on digital screens, reading, or uncorrected vision problems forces eye muscles to work harder.
When Eye Twitching May Signal a Medical Condition
While most twitching is temporary and self-limiting, certain patterns suggest an underlying neurological or muscular disorder. These conditions are rare but require medical evaluation if specific warning signs appear.
One such condition is benign essential blepharospasm, a progressive disorder causing increased frequency and intensity of spasms, often affecting both eyes. Over time, it may lead to functional blindness due to forced eyelid closure, though vision itself remains intact.
More serious causes include:
- Hemifacial spasm: Involuntary contractions on one side of the face, often starting near the eye and spreading downward. This may result from a blood vessel compressing a facial nerve.
- Multiple sclerosis (MS): A disease where the immune system attacks nerve coverings; eye twitching can be an early symptom alongside vision changes or numbness.
- Parkinson’s disease and other movement disorders: Though less commonly presenting with eyelid twitching, abnormal muscle movements may include facial tics.
- Bell’s palsy: Facial nerve inflammation that can cause weakness or spasms after recovery.
“Most eyelid twitches are nothing to worry about, but if the twitch spreads beyond the eye, causes the eye to close completely, or persists for weeks, it's time to consult a neurologist.” — Dr. Lena Patel, Neuro-Ophthalmologist, Massachusetts Eye and Ear
Do’s and Don’ts: Managing Eye Twitching
| Do | Don't |
|---|---|
| Get 7–8 hours of quality sleep per night | Consume excessive caffeine or stimulants |
| Use artificial tears for dry eyes | Rub your eyes vigorously during a spasm |
| Practice stress-reduction techniques like deep breathing or meditation | Ignore worsening symptoms lasting more than three weeks |
| Eat magnesium-rich foods like spinach, almonds, and avocado | Spend hours on screens without breaks |
| Take regular screen breaks using the 20-20-20 rule | Self-diagnose serious neurological conditions |
Real-Life Example: When Lifestyle Changes Made a Difference
Sarah, a 34-year-old software developer, began experiencing frequent left-eye twitching after transitioning to remote work. Initially dismissing it as fatigue, she noticed the twitch persisted for over two weeks, occasionally spreading to her cheek. Concerned, she tracked her habits and discovered she was drinking four energy drinks daily, sleeping fewer than six hours, and spending 10+ hours in front of screens.
After reducing caffeine, adopting a consistent sleep schedule, and implementing hourly screen breaks, her symptoms improved within ten days. A follow-up with her primary care provider ruled out neurological issues, confirming lifestyle factors were the root cause. Sarah now maintains a hydration and eye-care routine to prevent recurrence.
Step-by-Step Guide to Reducing Eye Twitching
- Track your symptoms: Note when the twitch occurs, how long it lasts, and any potential triggers (e.g., stress, screen time, caffeine).
- Reduce stimulants: Cut back on coffee, energy drinks, and nicotine over 5–7 days to minimize nervous system irritation.
- Improve sleep hygiene: Set a fixed bedtime, limit blue light exposure one hour before bed, and keep your bedroom cool and dark.
- Apply warm compresses: Use a clean, warm cloth on closed eyes for 5–10 minutes twice daily to relax muscles and improve circulation.
- Stay hydrated and eat balanced meals: Include leafy greens, nuts, and whole grains to support nerve health with essential minerals.
- Take visual breaks: Follow the 20-20-20 rule—every 20 minutes, look at something 20 feet away for 20 seconds.
- Seek medical advice: If twitching persists beyond three weeks, worsens, or spreads, consult a healthcare provider.
FAQ: Common Questions About Eye Twitching
Can eye twitching be a sign of a stroke?
No, isolated eyelid twitching is not a typical sign of stroke. Stroke symptoms usually involve sudden facial drooping (especially one side), arm weakness, speech difficulty, confusion, or severe headache. If twitching is accompanied by these signs, seek emergency care immediately—but twitching alone is rarely related to stroke.
Is eye twitching contagious?
No, eye twitching cannot spread from person to person. It results from internal physiological or neurological factors, not infection or pathogens.
Can children experience eye twitching?
Yes, children can have eye twitches, often due to fatigue, eye strain from devices, or mild nutritional deficiencies. However, persistent twitching in children should be evaluated by a pediatrician to rule out tic disorders or other conditions.
When to See a Doctor: Warning Signs
While most cases of eye twitching resolve independently, certain red flags warrant professional assessment:
- The twitch lasts longer than three weeks without improvement.
- It causes the eyelid to close completely or affects other facial muscles.
- You experience redness, swelling, discharge, or drooping eyelids.
- The twitch occurs in both eyes simultaneously and increases in severity.
- You notice other neurological symptoms like facial weakness, voice changes, or balance issues.
In such cases, your doctor may refer you to a neurologist or ophthalmologist. Diagnostic tools like MRI or electromyography (EMG) may be used to assess nerve function and rule out structural abnormalities.
Conclusion: Listen to Your Body
Random eye twitching is usually a minor annoyance rooted in lifestyle factors like stress, fatigue, or excessive screen time. Simple adjustments—better sleep, reduced caffeine, and mindful eye care—often bring quick relief. But when twitching becomes persistent, disruptive, or spreads beyond the eyelid, it’s a signal worth taking seriously.
Your body communicates through subtle cues. Responding early with informed action can prevent minor issues from escalating. If in doubt, always consult a healthcare professional. Prioritizing your well-being isn’t just about treating symptoms—it’s about understanding them.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?