Losing a pregnancy is a deeply personal and often isolating experience. When it happens more than once—defined as recurrent miscarriage, or two or more consecutive pregnancy losses—the emotional toll intensifies. Yet behind the pain lies a critical opportunity: understanding what may be contributing to these losses and taking informed steps toward a healthier future. Recurrent miscarriage affects approximately 1–2% of couples trying to conceive, and while not all cases have a clear cause, modern medicine offers tools to investigate, manage, and sometimes prevent further loss.
What Is Recurrent Miscarriage?
Medically, recurrent miscarriage (also known as recurrent pregnancy loss or RPL) is diagnosed after two or more consecutive clinical pregnancy losses before 20 weeks of gestation. A clinical pregnancy is confirmed by ultrasound or histological evidence, distinguishing it from chemical pregnancies, which are very early losses detected only by hormone tests.
It’s important to recognize that experiencing one miscarriage is relatively common—up to 15–20% of known pregnancies end this way—and does not necessarily indicate an underlying problem. However, when losses repeat, a thorough evaluation becomes essential.
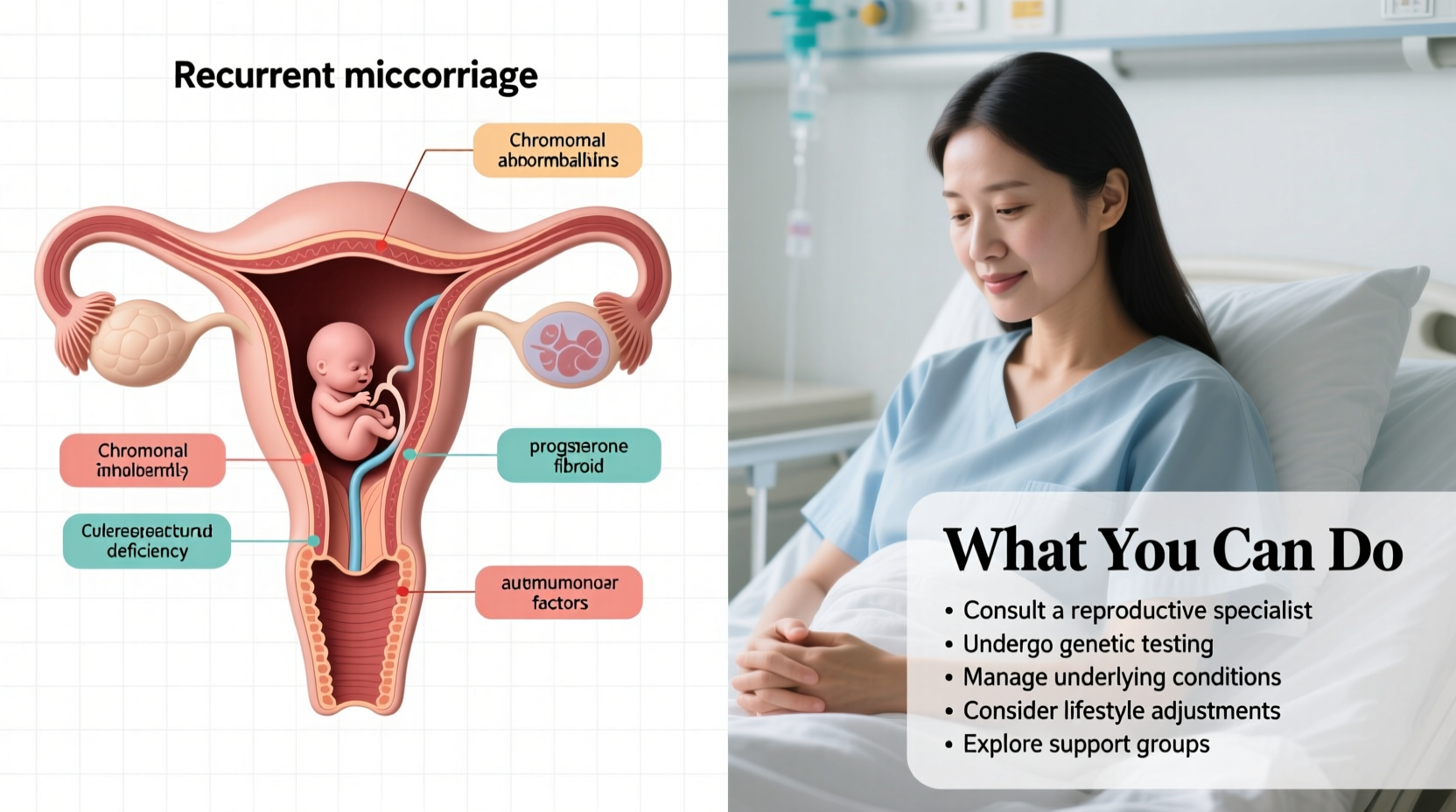
Common Causes of Recurrent Miscarriage
No single factor explains every case, but several well-documented causes can contribute to repeated pregnancy loss. Identifying them requires targeted testing and expert interpretation.
1. Chromosomal Abnormalities
The most frequent cause of early miscarriage is embryonic chromosomal anomalies, often due to random errors in cell division. In some cases, one partner may carry a balanced translocation—a rearrangement of chromosomes that doesn’t affect their health but can lead to unbalanced chromosomes in the embryo. This accounts for about 2–5% of recurrent miscarriage cases.
2. Uterine Structural Issues
Anatomical abnormalities in the uterus can interfere with implantation or fetal development. These include:
- Septate uterus (a wall dividing the uterine cavity)
- Intrauterine adhesions (Asherman’s syndrome)
- Fibroids or polyps distorting the cavity
A septate uterus is the most strongly associated structural issue with RPL and may be corrected surgically.
3. Endocrine and Metabolic Factors
Hormonal imbalances can disrupt early pregnancy maintenance. Key conditions include:
- Thyroid disorders: Both hypothyroidism and autoimmune thyroid disease increase risk.
- Uncontrolled diabetes: Poorly managed blood sugar raises miscarriage likelihood.
- Polycystic ovary syndrome (PCOS): Linked to higher loss rates, possibly due to insulin resistance or hormonal imbalance.
- Luteal phase defect: Insufficient progesterone production post-ovulation may impair uterine readiness.
4. Autoimmune and Thrombophilic Conditions
Antiphospholipid syndrome (APS) is the only widely accepted autoimmune cause of RPL. It involves antibodies that increase blood clotting, potentially disrupting placental blood flow. Testing includes lupus anticoagulant, anticardiolipin, and anti-β2-glycoprotein I antibodies.
Inherited thrombophilias (like Factor V Leiden) were once thought to play a major role, but current evidence suggests their impact on RPL is limited unless combined with other risk factors.
5. Immunological and Unexplained Factors
In up to 50% of cases, no definitive cause is found—a diagnosis labeled “unexplained recurrent miscarriage.” Research continues into immune system interactions between mother and embryo, though clinical applications remain limited. Age, lifestyle, and environmental factors may also contribute subtly.
“Even when tests come back normal, that doesn’t mean nothing can be done. Supportive care, close monitoring, and addressing modifiable risks still improve outcomes.” — Dr. Lena Patel, Reproductive Endocrinologist
What You Can Do: Evaluation and Next Steps
Taking action begins with a comprehensive medical workup. The goal isn’t just diagnosis—it’s empowerment through knowledge.
Recommended Testing After Recurrent Loss
| Test Category | Specific Tests | Purpose |
|---|---|---|
| Genetic | Karyotyping (for both partners) | Detect chromosomal translocations |
| Uterine Anatomy | Saline sonogram (SIS), hysterosalpingogram (HSG), or MRI | Assess shape and structure of uterine cavity |
| Hormonal | TSH, prolactin, HbA1c, AMH, day 3 FSH | Evaluate thyroid, ovarian reserve, metabolic health |
| Autoimmune | Antiphospholipid panel (lupus anticoagulant, etc.) | Diagnose antiphospholipid syndrome |
| Other | Vaginal culture, cervical length screening (later) | Rule out infection or cervical insufficiency |
Step-by-Step Guide: Navigating the Process
- Document your history: Gather dates, ultrasound reports, and pathology results from prior losses.
- See a specialist: A reproductive endocrinologist or RPL clinic offers expertise beyond general OB/GYN care.
- Complete recommended testing: Most evaluations occur during specific cycle phases—timing matters.
- Review results together: Ask for clear explanations and second opinions if needed.
- Develop a plan: Whether it's surgery, medication (like low-dose aspirin or heparin for APS), or IVF with PGT-A (preimplantation genetic testing), tailor treatment to your findings.
Real Example: Sarah’s Journey Through Recurrent Loss
Sarah, 34, experienced three miscarriages within two years. Each ended before 10 weeks, leaving her devastated and questioning whether she could ever carry a baby. After referral to a reproductive immunology clinic, karyotype testing revealed she carried a balanced translocation. Her husband’s results were normal. With this insight, they pursued IVF with PGT-SR (genetic testing for structural rearrangements). Of five embryos tested, two were chromosomally balanced. One was transferred in a carefully prepared cycle, resulting in a successful pregnancy and the birth of a healthy daughter.
Sarah’s story highlights how precise diagnosis—even in rare cases—can redirect a path toward parenthood.
Emotional Wellbeing and Support
Grief, anxiety, and relationship strain are common after repeated loss. Emotional resilience is not something to build alone. Consider:
- Counseling with a therapist specializing in fertility or perinatal loss
- Support groups (online or in-person) where shared experiences reduce isolation
- Mind-body practices like mindfulness, yoga, or acupuncture to manage stress
One study found that women who received psychological support during subsequent pregnancies reported lower anxiety and higher perceived control—even when no medical intervention changed.
Frequently Asked Questions
Can stress cause recurrent miscarriage?
While chronic stress isn't proven to directly cause miscarriage, it can affect hormonal balance and overall health. Managing stress supports general wellbeing, but it should not be blamed for pregnancy loss. Most miscarriages result from biological factors beyond emotional control.
Is IVF necessary after recurrent miscarriage?
Not always. Many women conceive naturally after diagnosis and treatment. IVF with PGT-A may be recommended for those with chromosomal issues, diminished ovarian reserve, or unexplained losses despite optimal conditions. It’s one tool among many, not a universal solution.
Will I ever have a successful pregnancy?
Yes—many do. Even in unexplained cases, the chance of a live birth in the next pregnancy ranges from 50% to 70%, depending on age and number of prior losses. Early monitoring and supportive care improve outcomes significantly.
Action Plan Checklist
- ✔ Gather medical records
- Collect ultrasound reports, pathology results, and dates of past losses.
- ✔ Schedule a specialist consultation
- Look for a reproductive endocrinologist or clinic with RPL experience.
- ✔ Complete core diagnostic tests
- Karyotypes, uterine imaging, hormone panel, and antiphospholipid screening.
- ✔ Address modifiable lifestyle factors
- Maintain healthy weight, avoid smoking/alcohol, take prenatal vitamins with folic acid.
- ✔ Prioritize mental health
- Seek therapy or join a support group to process grief and build resilience.
Conclusion: Moving Forward with Clarity and Hope
Recurrent miscarriage is not a life sentence of loss. It is a signal—one that invites deeper investigation, compassionate care, and proactive planning. While answers aren’t always immediate or complete, each step taken toward understanding brings greater clarity. Whether through medical intervention, emotional healing, or simply knowing you’re not alone, progress is possible.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?