Bacterial vaginosis (BV) is the most common vaginal condition among women aged 15 to 44, yet it remains widely misunderstood. While many experience occasional episodes, a significant number struggle with recurring BV—defined as three or more symptomatic episodes within a year. Despite treatment, symptoms like fishy odor, grayish discharge, and irritation often return within weeks. The frustration is real: you follow medical advice, complete antibiotics, and still find yourself back at square one. Understanding the root causes of recurrence is key to breaking the cycle.
What Is Bacterial Vaginosis?
BV occurs when the natural balance of bacteria in the vagina is disrupted. Normally, lactobacilli—beneficial bacteria—dominate the vaginal microbiome, maintaining an acidic environment that prevents harmful microbes from thriving. In BV, these protective bacteria decline, allowing anaerobic bacteria such as Gardnerella vaginalis, Prevotella, and Atopobium to overgrow.
Unlike yeast infections or sexually transmitted infections, BV isn’t classified as an STI, but sexual activity increases risk. It’s not caused by poor hygiene; in fact, excessive cleaning can worsen it. Symptoms vary—some women have no signs at all—while others face discomfort that affects daily life and intimacy.
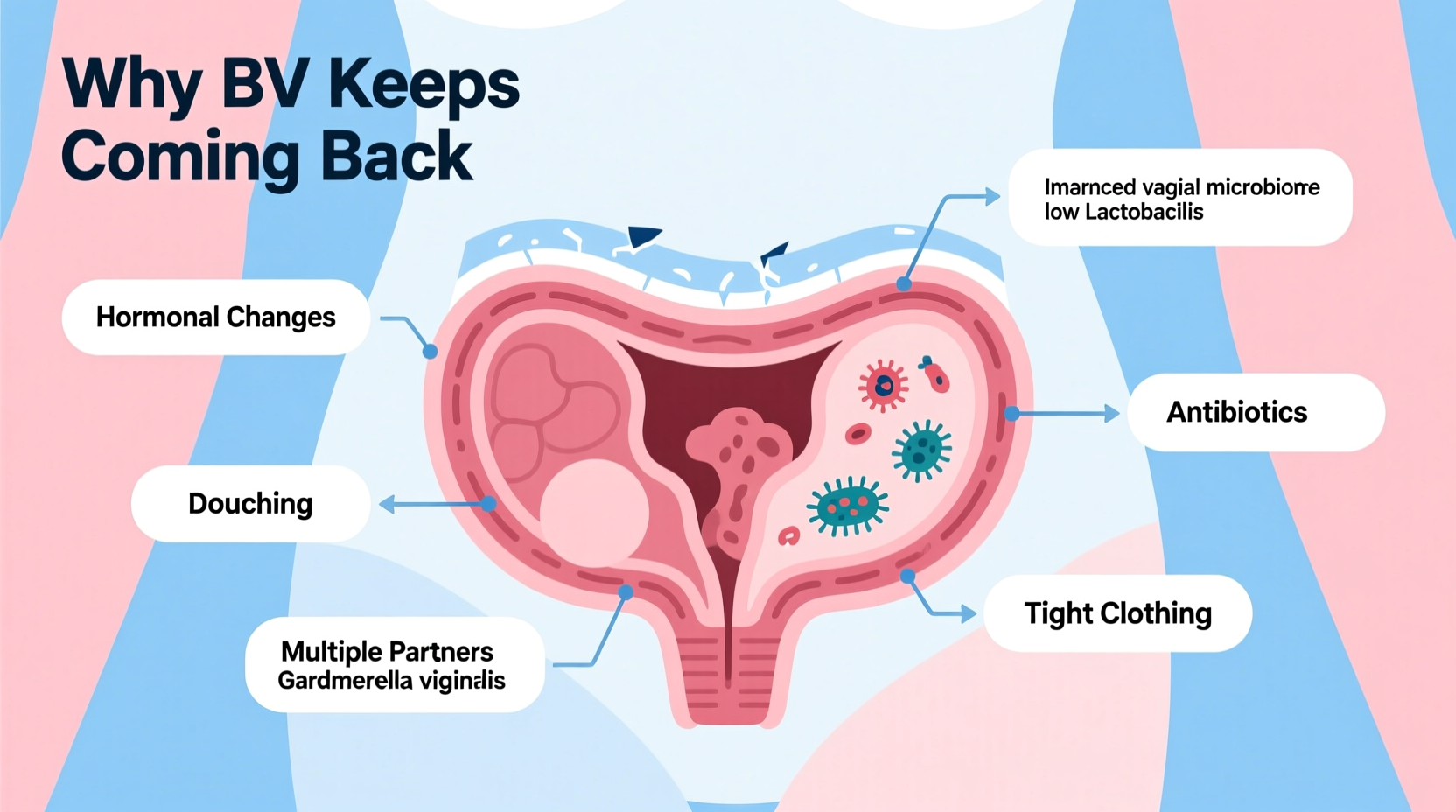
Why Does BV Keep Coming Back?
Recurrence rates are high: up to 60% of women experience a relapse within 6–12 months after antibiotic treatment. The reasons are multifactorial, involving biological, behavioral, and environmental influences.
1. Incomplete Restoration of Lactobacilli
Antibiotics like metronidazole or clindamycin effectively reduce harmful bacteria but don’t always help repopulate healthy lactobacilli. Without this crucial step, the vaginal ecosystem remains vulnerable to reinvasion.
2. Sexual Practices and Partners
While BV isn’t contagious, sexual activity—especially with new or multiple partners—alters vaginal pH and introduces competing bacteria. Women who have sex with women face higher recurrence due to shared microbial transfer during intercourse.
“Even if treated, reintroduction of biofilm-forming bacteria from a partner can reseed the infection.” — Dr. Lisa M. Valle, OB-GYN and Infectious Disease Researcher
3. Douching and Harsh Hygiene Products
The vagina is self-cleaning. Douching disrupts pH, washes away good bacteria, and pushes pathogens deeper into the reproductive tract. Scented soaps, wipes, and bubble baths have similar effects.
4. Hormonal Fluctuations
Menstruation, ovulation, and menopause affect vaginal acidity. Estrogen supports lactobacillus growth; lower levels during certain phases weaken microbial defenses.
5. Biofilm Formation
Some anaerobic bacteria form protective biofilms on vaginal cells—slime-like layers that resist antibiotics and immune responses. These “shields” allow bacteria to survive treatment and reactivate later.
Effective Prevention Strategies
Managing recurrent BV requires more than short-term medication. A long-term strategy focused on restoring and sustaining a healthy microbiome is essential.
Step-by-Step Guide to Reducing Recurrence
- Complete prescribed treatments: Finish full courses of antibiotics even if symptoms improve.
- Avoid douching and scented products: Use only warm water or mild, unscented soap on the vulva.
- Use probiotics: Oral or vaginal formulations containing L. rhamnosus GR-1 and L. reuteri RC-14 show promise in clinical studies.
- Practice safer sex: Use condoms consistently, even with long-term partners, to minimize bacterial exchange.
- Wipe front to back: Prevents gut bacteria like E. coli from entering the vaginal area.
- Change out of wet clothing promptly: Moist environments promote bacterial growth.
- Consider partner management: Though not standard, some specialists recommend male partner hygiene or female partner screening in recurrent cases.
Do’s and Don’ts: Managing Vaginal Health
| Do’s | Don’ts |
|---|---|
| Wear cotton underwear for breathability | Douch or use vaginal deodorants |
| Use condoms during sex | Use harsh soaps or body washes internally |
| Take probiotics regularly | Ignore symptoms hoping they’ll go away |
| See your provider at first sign of recurrence | Share towels or washcloths with sexual partners |
| Keep vulvar area dry and clean | Wear tight synthetic clothing for extended periods |
Real-Life Example: Breaking the Cycle
Maria, a 32-year-old teacher, had been battling BV for over two years. She visited her gynecologist four times annually, each time receiving metronidazole. Relief lasted about three weeks. Frustrated, she sought a second opinion. Her new doctor reviewed her habits: frequent use of scented wipes, regular hot tub use, and unprotected sex with her partner. She also took broad-spectrum antibiotics for sinus infections twice a year.
The doctor recommended stopping all scented products, using vaginal probiotics daily, wearing breathable underwear, and treating both Maria and her partner with sequential antibiotic-probiotic protocols. Within five months, Maria reported no recurrences. Lab tests confirmed a stable lactobacillus-dominant flora.
Her case illustrates how lifestyle adjustments, combined with targeted medical support, can make a lasting difference.
When to Seek Medical Help
Recurrent BV should never be ignored. Left unmanaged, it increases the risk of:
- Pelvic inflammatory disease (PID)
- Increased susceptibility to HIV and other STIs
- Pregnancy complications, including preterm birth and low birth weight
If you’ve had three or more episodes in a year, ask your provider about extended treatment regimens. Some options include:
- Suppressive therapy: Weekly metronidazole gel for 4–6 months
- Sequential treatment: Antibiotic followed by vaginal probiotics
- pH-stabilizing gels: Products like boric acid suppositories help restore acidity
“We now recognize that recurrent BV is not just a failure of antibiotics, but a failure to rebuild the microbiome.” — Dr. Amira Chen, Reproductive Immunologist
Frequently Asked Questions
Can my partner give me BV?
Not directly. BV isn’t transmitted like an STI, but sexual activity introduces bacteria that can alter your vaginal balance. Female partners may share BV-associated bacteria through genital contact.
Are home remedies effective for BV?
Yogurt, apple cider vinegar soaks, and garlic lack strong evidence and may irritate sensitive tissue. Stick to clinically proven methods unless advised otherwise by a healthcare provider.
Is boric acid safe for recurrent BV?
Yes, when used correctly. Boric acid suppositories (600 mg nightly for 7–14 days) are effective against resistant strains and biofilms. Avoid oral ingestion and use only under medical supervision.
Conclusion: Take Control of Your Vaginal Health
Recurring BV is not a personal failing—it’s a complex imbalance requiring informed, consistent care. By understanding the triggers, adopting protective habits, and working closely with a knowledgeable provider, you can break the cycle. Healing isn’t just about eliminating symptoms; it’s about rebuilding a resilient, self-sustaining vaginal environment.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?