If you've had three or more urinary tract infections (UTIs) in the past year—or two within six months—you're not alone. Recurrent UTIs affect nearly 25% of women who experience one initial infection. While often treatable with antibiotics, the frustration of repeated symptoms—burning during urination, urgency, pelvic pressure, and fatigue—can significantly impact quality of life. The real question isn't just how to treat them, but why they keep coming back.
Understanding the root causes behind recurring UTIs is essential for long-term relief. It’s not simply poor hygiene or drinking too little water, though those can contribute. Underlying anatomical, hormonal, behavioral, and microbial factors often play a role. This article breaks down the most common reasons for persistent UTIs and offers practical, evidence-based solutions to reduce recurrence.
What Defines a Recurring UTI?
A recurring UTI is typically defined as:
- Two confirmed infections in six months, or
- Three or more in a single year.
These infections usually involve the lower urinary tract (bladder and urethra), known as cystitis. While less common, some individuals may also experience recurrent kidney infections (pyelonephritis), which require prompt medical attention.
It's important to distinguish between true recurrence and reinfection. A recurrence happens when the same bacterial strain returns shortly after treatment, suggesting incomplete eradication or bacterial persistence. Reinfection occurs when a new strain causes another infection, often due to ongoing risk factors.
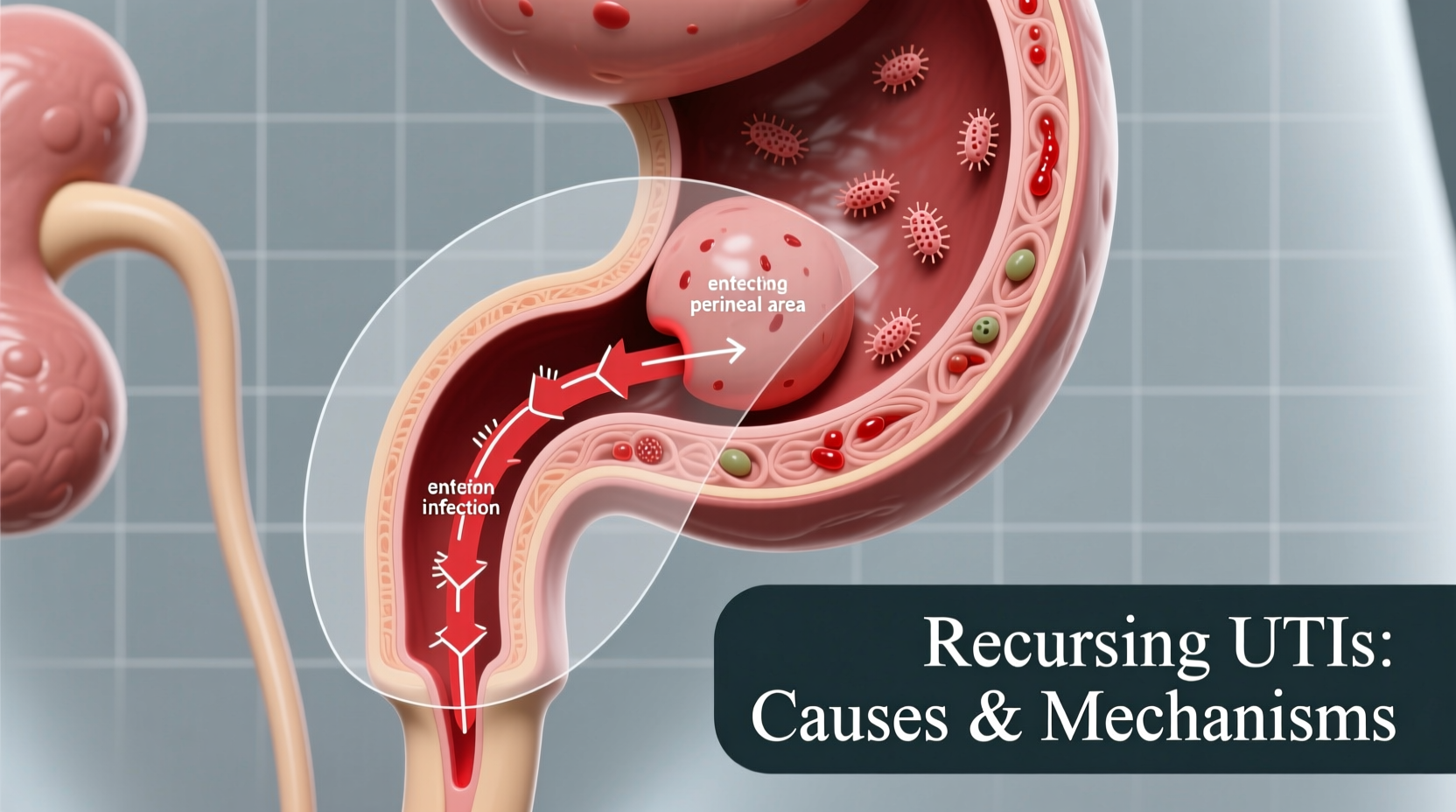
Common Causes of Frequent UTIs
Several interrelated factors increase susceptibility to repeated infections. Recognizing these can help tailor prevention strategies.
Anatomical and Physiological Factors
The female anatomy is a primary contributor. Women have shorter urethras than men, making it easier for bacteria—especially Escherichia coli from the gastrointestinal tract—to reach the bladder. Other anatomical issues include:
- Vaginal atrophy due to low estrogen levels (common post-menopause)
- Urinary retention or incomplete bladder emptying
- Bladder prolapse or pelvic floor dysfunction
- Structural abnormalities in the urinary tract
Hormonal Changes
Estrogen plays a protective role in urinary health. After menopause, declining estrogen leads to thinner vaginal and urethral tissues, reduced beneficial lactobacilli, and increased pH—creating an environment where harmful bacteria thrive. Even younger women on certain contraceptives (like spermicides or diaphragms) may experience similar shifts.
“Postmenopausal women are at higher risk not because they’re ‘dirty,’ but because their natural defenses weaken. Local estrogen therapy can restore that protection.” — Dr. Linda Chen, Urogynecologist
Sexual Activity
Sexual intercourse is a well-documented trigger. The mechanical action can introduce bacteria into the urethra. This is sometimes referred to as “honeymoon cystitis,” though it affects many women regardless of relationship status. Use of spermicides further increases risk by disrupting healthy vaginal flora.
Chronic Bacterial Reservoirs
Some bacteria can hide inside bladder cells, forming intracellular bacterial communities (IBCs). These reservoirs evade antibiotics and immune responses, then re-emerge later to cause new infections. This phenomenon helps explain why some UTIs return despite proper treatment.
Weakened Immune Response
Conditions like diabetes, chronic stress, or immunosuppressive medications can impair the body’s ability to fight off infections. Poorly controlled blood sugar also promotes bacterial growth in urine.
Do’s and Don’ts: What Actually Helps Prevent UTIs?
| Do | Don’t |
|---|---|
| Stay well-hydrated to flush bacteria regularly | Hold urine for long periods |
| Wipe front to back after using the toilet | Use scented soaps, douches, or sprays near the genital area |
| Consider cranberry products (with proanthocyanidins) | Rely solely on cranberry juice cocktails (high sugar content negates benefits) |
| Use vaginal estrogen if postmenopausal | Take antibiotics without confirmation (urine culture) |
| Wear cotton underwear and loose-fitting clothes | Wear tight synthetic underwear or wet workout clothes for hours |
Step-by-Step Prevention Plan
Managing recurring UTIs requires a proactive, multi-layered approach. Follow this timeline to build sustainable habits:
- Week 1–2: Assess Triggers
Keep a symptom diary noting timing of infections in relation to sex, menstruation, hydration, clothing, and bathroom habits. - Week 3: See a Specialist
Visit a urologist or urogynecologist. Request a urine culture during active infection and consider tests for residual urine volume or vaginal pH. - Month 2: Implement Lifestyle Adjustments
Increase daily water intake (aim for 1.5–2L), switch to non-spermicidal contraception if applicable, and begin pelvic floor exercises. - Month 3: Start Preventive Therapy (if recommended)
Options include low-dose nightly antibiotics, methenamine hippurate, or vaginal probiotics/estrogen. Never self-prescribe. - Ongoing: Monitor and Adapt
Re-evaluate every 6 months. Some patients only need seasonal prophylaxis (e.g., during summer or active travel).
Real-Life Example: Sarah’s Turnaround
Sarah, a 48-year-old teacher, had suffered six UTIs in 10 months. She drank cranberry juice, avoided caffeine, and wiped carefully—but infections kept returning. After seeing a specialist, she discovered her postmenopausal vaginal dryness was creating a hospitable environment for bacteria. Her doctor prescribed a low-dose vaginal estrogen cream. Within three months, her symptoms improved dramatically. Combined with timed voiding after sex and increased hydration, she remained UTI-free for over a year—her longest stretch in a decade.
Her case highlights that even diligent hygiene isn’t enough when underlying physiological changes go unaddressed.
Frequently Asked Questions
Can men get recurring UTIs?
Yes, though less commonly. In men, recurrent UTIs are often linked to prostate enlargement, catheter use, or urinary tract abnormalities. Any man with two or more UTIs should be evaluated for structural or functional issues.
Are probiotics effective for preventing UTIs?
Emerging evidence supports the use of specific strains—particularly Lactobacillus rhamnosus GR-1 and L. reuteri RC-14—for restoring healthy vaginal flora and reducing UTI risk. Oral and vaginal formulations exist, but consistency matters. Effects may take 2–3 months to become noticeable.
Should I take antibiotics every time I feel symptoms?
No. Self-treating without confirmation can lead to antibiotic resistance and mask other conditions like interstitial cystitis or sexually transmitted infections. Always get a urine test. Some providers offer “start-and-stop” prescriptions with clear instructions on when to use them.
Action Checklist: Reduce Your UTI Risk
- ✅ Drink at least six to eight glasses of water daily
- ✅ Urinate before and soon after sexual activity
- ✅ Avoid spermicides and diaphragms if possible
- ✅ Use gentle, fragrance-free soap for intimate hygiene
- ✅ Consider vaginal estrogen if postmenopausal (after consulting your doctor)
- ✅ Discuss preventive options with a healthcare provider if infections persist
- ✅ Get a urine culture with each symptomatic episode
Conclusion: Take Control of Your Urinary Health
Recurring UTIs are not something you just have to live with. While common, they are not normal—and they’re often preventable with the right strategy. Whether the cause is hormonal, behavioral, or anatomical, identifying your personal risk profile is the first step toward lasting relief. Work with a knowledgeable provider, avoid one-size-fits-all advice, and prioritize evidence-based interventions over myths.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?