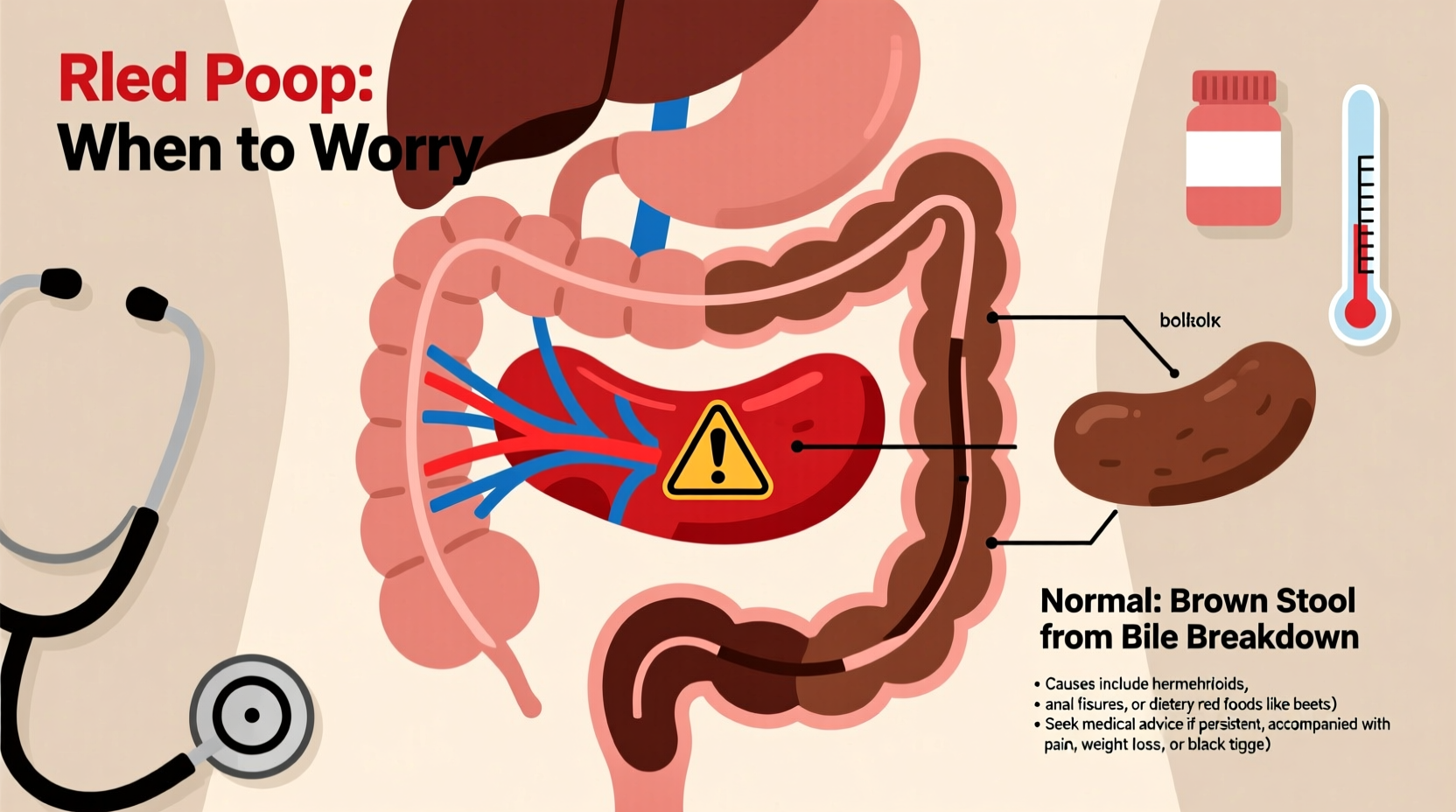
Seeing red in your stool can be alarming. It’s natural to wonder whether it’s something you ate—or a sign of a more serious health issue. While bright red poop isn’t always dangerous, it shouldn’t be ignored, especially if it happens repeatedly or comes with other symptoms. Understanding the difference between harmless causes and those requiring medical attention is key to making informed decisions about your digestive health.
This article breaks down the most common reasons for red-colored stool, highlights red flags that warrant a doctor’s visit, and offers practical guidance on when it’s safe to monitor at home—and when it’s time to seek help.
Common Causes of Red Poop
Not all red stools indicate bleeding. Many benign dietary and lifestyle factors can temporarily change stool color. These are usually one-time occurrences and resolve on their own.
- Foods with natural or artificial red coloring: Beets, tomato soup, cranberries, red gelatin, and popsicles can tint stool pink or red.
- Iron supplements or certain medications: Some multivitamins and iron-rich formulations may cause dark or reddish stools, though they’re more likely to turn stool black.
- Artificial food dyes: Found in candies, sports drinks, and processed snacks, these dyes pass through the digestive tract unchanged and may discolor stool.
In most cases, if you’ve recently eaten beets or had a red slushie, the culprit is obvious. The color typically fades within a day or two after stopping consumption.
When Red Poop Signals a Medical Concern
While diet is often to blame, red stool can also indicate gastrointestinal bleeding—especially if the color is maroon, dark red, or mixed with blood clots. Bleeding typically occurs in the lower digestive tract, such as the colon, rectum, or anus.
Common medical causes include:
- Hemorrhoids: Swollen veins in the rectum or anus that may bleed during bowel movements. Blood is usually bright red and seen on toilet paper or dripping into the bowl.
- Anal fissures: Small tears in the anal lining caused by passing hard stools. They often cause sharp pain and streaks of bright red blood.
- Colitis: Inflammation of the colon due to infections, inflammatory bowel disease (IBD), or reduced blood flow.
- Diverticulosis: Small pouches in the colon wall that can bleed, causing sudden, painless passage of bright red blood.
- Polyps or colorectal cancer: Growths in the colon that may bleed over time. Cancer-related bleeding is often subtle and chronic.
“Any persistent red discoloration without a clear dietary cause should be evaluated. Even small amounts of blood, if recurrent, can signal underlying pathology.” — Dr. Lena Torres, Gastroenterologist
Red Flags: When to See a Doctor Immediately
Most cases of red stool aren’t emergencies, but some symptoms require prompt medical evaluation. Don’t wait if you experience any of the following:
| Symptom | Potential Implication |
|---|---|
| Bright red blood in large amounts | Active lower GI bleeding |
| Dizziness, weakness, or fainting | Significant blood loss or anemia |
| Severe abdominal pain or cramping | Ischemic colitis, infection, or obstruction |
| Fever with bloody stool | Infection (e.g., bacterial colitis) |
| Unintentional weight loss | Chronic condition like IBD or cancer |
| Stool that looks like jelly with blood | Severe inflammation or infection |
If you're over 45 or have a family history of colon cancer, even mild rectal bleeding should be assessed. Early detection saves lives.
Mini Case Study: Recognizing a Hidden Issue
Jamal, a 52-year-old teacher, noticed occasional red streaks on his toilet paper. He assumed it was hemorrhoids, which ran in his family. He used over-the-counter creams and increased fiber intake. But after three months of intermittent bleeding—and a 7-pound unexplained weight loss—he scheduled a colonoscopy. The test revealed a precancerous polyp in the descending colon. Removed early, it prevented progression to cancer. His story underscores why persistent symptoms deserve investigation, even without pain.
Step-by-Step: What to Do If You Notice Red Stool
Follow this timeline to assess and respond appropriately:
- Day 1 – Evaluate recent diet: Did you eat beets, tomatoes, or red-dyed foods? If yes, monitor for one more bowel movement.
- Day 2 – Check consistency and frequency: Is the red color gone? If so, it was likely dietary. If not, note the amount and appearance of blood.
- Day 3 – Assess accompanying symptoms: Look for pain, changes in bowel habits, fatigue, or fever.
- Within 1 week – Contact your doctor if: Bleeding continues, you feel weak, or you’re over 40 with new-onset symptoms.
- Schedule diagnostic tests if advised: Options include fecal occult blood test, colonoscopy, or sigmoidoscopy.
Do’s and Don’ts: Managing Red Stool at Home
| Do’s | Don’ts |
|---|---|
| Track your diet and symptoms | Ignore repeated episodes |
| Stay hydrated and increase fiber gradually | Use harsh laxatives without advice |
| Use gentle wipes or moist cloths after bowel movements | Assume it’s just hemorrhoids without confirmation |
| See a doctor if over 40 or high-risk | Delay testing due to embarrassment |
FAQ
Is red poop always a sign of bleeding?
No. Red stool is often caused by food pigments like those in beets or artificial dyes. True bleeding usually presents with consistent red streaks, clots, or maroon-colored stool, especially if no dietary cause exists.
Can hemorrhoids cause significant bleeding?
Yes. Hemorrhoids can produce noticeable bright red blood, especially during straining. While usually not dangerous, heavy or prolonged bleeding can lead to iron deficiency and should be evaluated.
How soon should I get a colonoscopy if I have red stool?
If you’re over 45, have a family history of colon cancer, or experience persistent bleeding—even without pain—a colonoscopy should be scheduled within a few weeks. For younger adults with mild, infrequent bleeding and no risk factors, a primary care consultation may come first.
Conclusion: Stay Informed, Stay Proactive
Red poop doesn’t automatically mean something is wrong, but it’s a signal your body may need attention. Most causes are manageable, and many are entirely preventable with proper diet and bowel habits. However, dismissing symptoms because “it’s probably nothing” can delay diagnosis of serious conditions like colorectal cancer.
Your digestive health is a vital part of your overall well-being. Pay attention to changes, document patterns, and don’t hesitate to consult a healthcare provider when in doubt. Early action can prevent complications and provide peace of mind.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?