A sudden appearance of red lines or spots beneath the fingernails or toenails can be alarming. While sometimes harmless, red discoloration under the nails may signal underlying health issues ranging from minor trauma to serious systemic diseases. Understanding the possible causes, recognizing warning signs, and knowing when to consult a healthcare provider is essential for timely diagnosis and treatment.
What Causes Red Discoloration Under the Nails?
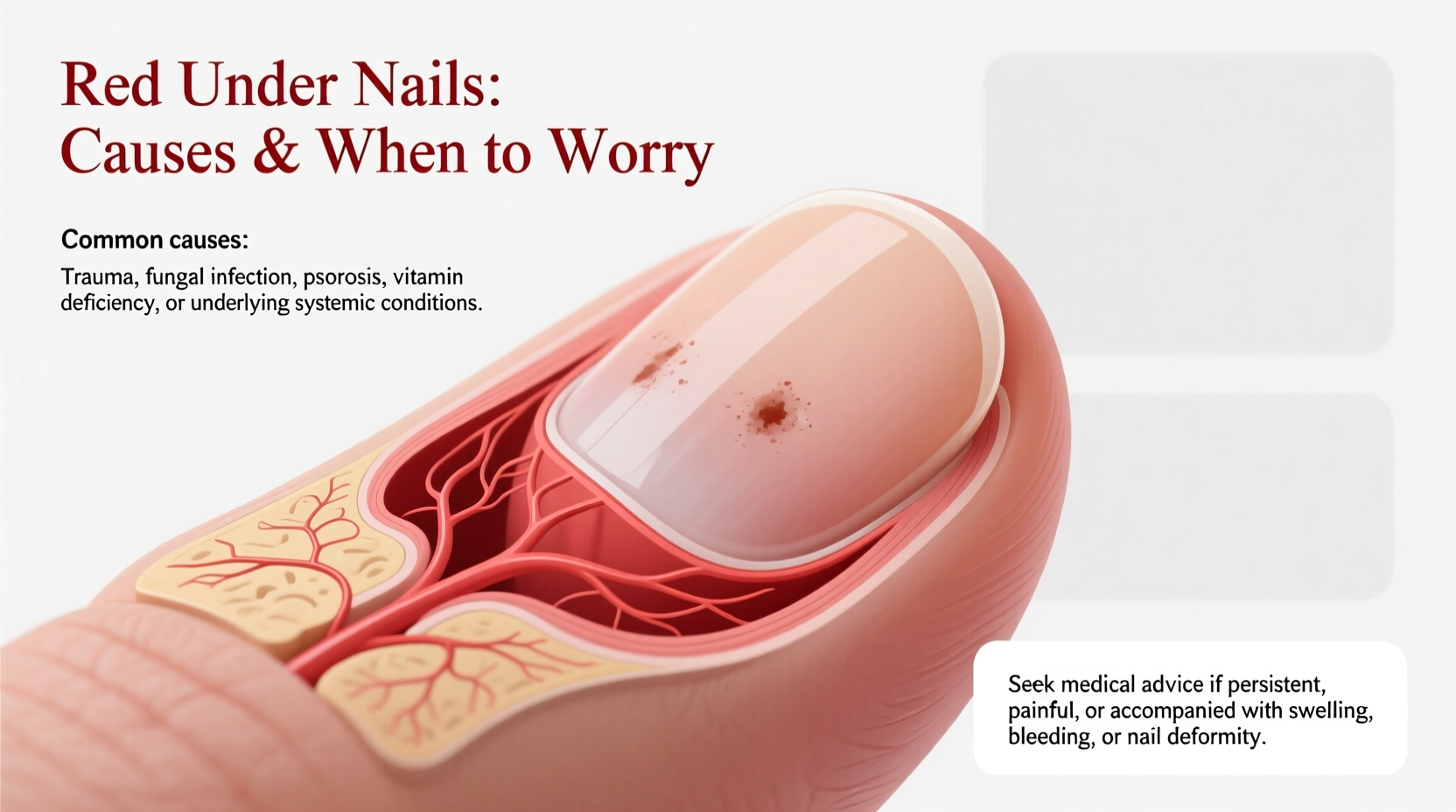
The area beneath the nail, known as the nail bed, is rich in blood vessels. Any disruption—whether from injury, infection, or disease—can lead to visible changes such as redness, streaks, or dots. The most common cause of red under the nails is splinter hemorrhage, but other conditions like fungal infections, psoriasis, and even cardiovascular issues may also manifest in this way.
Splinter hemorrhages appear as thin, dark red or brown lines running vertically from the base toward the tip of the nail. Despite their name, they are not caused by splinters but by tiny clots in the capillaries beneath the nail.
Trauma and Minor Injuries
One of the most frequent reasons for redness under the nails is physical trauma. Dropping something on your toe, slamming a finger in a door, or repetitive pressure (like from tight shoes or aggressive manicures) can rupture small blood vessels. This results in a localized pool of blood that appears red or dark purple.
In most cases, the discoloration will grow out with the nail over several weeks and requires no treatment. However, if pain, swelling, or pus develops, an infection could be present.
Medical Conditions Linked to Red Under Nails
While trauma accounts for many cases, persistent or unexplained red streaks warrant medical evaluation. Several systemic conditions are associated with nail bed changes.
1. Splinter Hemorrhages and Heart Health
Splinter hemorrhages are often benign, especially if only one or two nails are affected and there's a history of injury. However, when multiple nails show these lines without clear trauma, it may indicate a more serious condition such as infective endocarditis—an infection of the heart valves.
According to the American Heart Association, “Splinter hemorrhages, along with Janeway lesions and Osler’s nodes, are considered peripheral signs of infective endocarditis.” These occur due to microemboli (tiny clots) traveling through the bloodstream and lodging in small vessels under the nails.
“Recurrent or widespread splinter hemorrhages should prompt evaluation for cardiovascular or autoimmune disorders.” — Dr. Lena Torres, Dermatologist and Nail Specialist
2. Fungal Infections (Onychomycosis)
Fungal infections can cause yellowing, thickening, and crumbling of the nail, but they may also lead to reddish-brown discoloration underneath. As fungi break down keratin, debris accumulates, which can appear red or dark due to trapped blood or inflammatory response.
This type of discoloration usually affects toenails more than fingernails and is often accompanied by odor, separation of the nail from the bed (onycholysis), and discomfort.
3. Psoriasis and Nail Disease
Nail psoriasis affects nearly 90% of people with psoriatic arthritis. It can cause pitting, ridges, oil-drop spots (yellow-red patches under the nail), and splinter-like hemorrhages. The “oil drop” sign—a salmon-pink discoloration—is highly suggestive of psoriatic involvement.
Unlike traumatic hemorrhages, psoriasis-related changes tend to affect multiple nails and progress slowly over time.
4. Systemic Illnesses
Certain chronic diseases can manifest through nail changes:
- Lupus erythematosus: Can cause red lunulae (the half-moon at the nail base) and periungual telangiectasias (dilated capillaries around the cuticle).
- Rheumatoid arthritis: May present with brittle nails and subungual redness.
- HIV/AIDS: Associated with various nail pigmentation changes, including longitudinal red bands.
When to Worry: Warning Signs That Require Medical Attention
Not every instance of red under the nails demands urgent care, but certain symptoms should not be ignored. Early detection of serious conditions like endocarditis or vasculitis can be life-saving.
| Sign/Symptom | Benign Cause Likely? | Seek Medical Advice? |
|---|---|---|
| Single red line after stubbing toe | Yes | No, unless painful or enlarging |
| Multiple red streaks across several nails | No | Yes – rule out systemic illness |
| Pain, warmth, swelling around nail | No | Yes – possible infection |
| Fever with new nail changes | No | Yes – especially if IV drug use or heart condition |
| Nail lifting or crumbling | Depends | Yes – evaluate for fungus or psoriasis |
Mini Case Study: Unexplained Nail Changes Reveal Heart Infection
John, a 54-year-old man with a history of congenital heart defect, noticed several dark red lines appearing under his fingernails over two weeks. He had no recent injuries but felt fatigued and occasionally ran low-grade fevers. His primary care physician referred him to a cardiologist after observing additional signs—Osler’s nodes on fingers and a new heart murmur. Blood cultures confirmed Staphylococcus aureus bacteremia, leading to a diagnosis of infective endocarditis. Prompt antibiotic therapy prevented valve damage. His nail changes resolved within three months.
This case illustrates how seemingly minor nail findings can serve as early clues to severe internal disease.
Step-by-Step Guide: What to Do If You Notice Red Under Your Nails
- Assess for recent trauma: Recall any incidents involving impact or pressure on fingers or toes.
- Inspect all nails: Note whether one or multiple nails are involved.
- Check for other symptoms: Look for fever, joint pain, fatigue, shortness of breath, or skin rashes.
- Monitor progression: Take weekly photos to track changes in size, color, or number of streaks.
- Consult a healthcare provider: Especially if you have pre-existing heart conditions, autoimmune disease, or HIV.
- Prepare for possible tests: Your doctor may order blood work, echocardiogram, or nail biopsy depending on suspicion level.
Do’s and Don’ts When Dealing With Red Under Nails
| Do’s | Don’ts |
|---|---|
| Keep nails clean and trimmed | Ignore widespread or recurring red streaks |
| Protect hands and feet from injury | Use harsh chemicals or acetone-based removers excessively |
| See a dermatologist for persistent changes | Self-diagnose based on internet searches alone |
| Report nail changes to your doctor during routine visits | Share nail tools during manicures or pedicures |
Frequently Asked Questions
Can stress cause red lines under my nails?
No direct link exists between emotional stress and splinter hemorrhages. However, stress-related habits like nail biting or picking can lead to micro-injuries that result in bleeding under the nail. Chronic stress may also exacerbate autoimmune conditions like psoriasis, which can affect the nails.
How long does it take for a splinter hemorrhage to go away?
Since nails grow slowly—about 3 mm per month—it typically takes 3 to 6 months for a hemorrhage to grow out completely. If the red line moves upward and fades, it's likely resolving naturally. New or stationary lines require further evaluation.
Are red lines under nails always dangerous?
No. Isolated, asymptomatic splinter hemorrhages following minor trauma are usually harmless. But when combined with other symptoms—fever, weight loss, fatigue, or existing heart conditions—they may indicate a serious underlying issue.
Final Thoughts: Listen to Your Body’s Signals
Your nails are more than just cosmetic features—they’re windows into your overall health. A small red streak might seem trivial, but in some cases, it’s the first visible clue to a deeper problem. Pay attention to patterns, document changes, and don’t hesitate to ask questions during medical appointments.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?