Sensory issues affect how the brain processes information from the senses—touch, sound, sight, smell, taste, and movement. While commonly associated with neurodevelopmental conditions like autism or ADHD, sensory sensitivities can also arise due to injury, illness, or environmental factors. For many individuals, these challenges remain stable over time. However, in some cases, sensory symptoms worsen unexpectedly, impacting concentration, emotional regulation, and quality of life. Understanding why this happens, how to manage it effectively, and when to involve professionals is essential for long-term well-being.
What Are Sensory Issues?
Sensory processing difficulties occur when the nervous system struggles to interpret and respond appropriately to sensory input. Some people are hypersensitive (over-responsive), meaning everyday stimuli feel overwhelming. Others are hyposensitive (under-responsive), often seeking intense sensory experiences. These patterns may manifest as discomfort from clothing tags, distress during loud events, aversion to certain food textures, or a constant need for movement.
While sensory differences are most frequently discussed in children, adults experience them too—sometimes developing new sensitivities later in life due to stress, trauma, or neurological changes. The key is not just recognizing these signs but understanding what might be making them worse over time.
Common Causes of Worsening Sensory Symptoms
Sudden or gradual intensification of sensory issues doesn't happen without reason. Several underlying factors can contribute:
- Increased stress or anxiety: Chronic stress alters brain chemistry, heightening sensory reactivity. During high-stress periods, even mild stimuli can trigger strong reactions.
- Sleep deprivation: Poor sleep disrupts neural regulation, lowering the threshold for sensory tolerance.
- Medical conditions: Migraines, fibromyalgia, post-concussion syndrome, and autoimmune disorders like lupus have been linked to heightened sensory sensitivity.
- Aging and neurological decline: Conditions such as dementia or Parkinson’s disease can impair sensory integration.
- Medication side effects: Certain drugs, including stimulants or antidepressants, may increase sensory awareness as an unintended consequence.
- Environmental overload: Prolonged exposure to noisy, cluttered, or chaotic environments can exhaust sensory coping mechanisms.
Effective Management Strategies
Managing sensory issues requires a personalized, multi-layered approach. What works for one person may not suit another, so experimentation and consistency are crucial.
Environmental Modifications
Adjusting your surroundings can significantly reduce sensory strain. Consider using noise-canceling headphones in busy areas, switching to soft, tagless clothing, or installing dimmer switches to control lighting intensity. Creating designated \"quiet zones\" at home or work provides a retreat when stimulation becomes overwhelming.
Regulation Techniques
Self-regulation tools help reset the nervous system. Deep pressure activities—such as weighted blankets or compression garments—can provide calming input. Mindfulness practices, slow breathing exercises, and grounding techniques (e.g., 5-4-3-2-1 method) are effective during acute sensory overload.
Diet and Lifestyle Adjustments
Nutrition plays a subtle yet important role. Diets high in processed foods, sugar, or artificial additives may exacerbate sensitivities in some individuals. Staying hydrated, maintaining regular mealtimes, and reducing caffeine intake support overall neurological stability.
“Sensory modulation isn’t about eliminating stimuli—it’s about building resilience through predictable routines and controlled exposure.” — Dr. Lena Patel, Occupational Therapist & Sensory Integration Specialist
When to Seek Professional Help
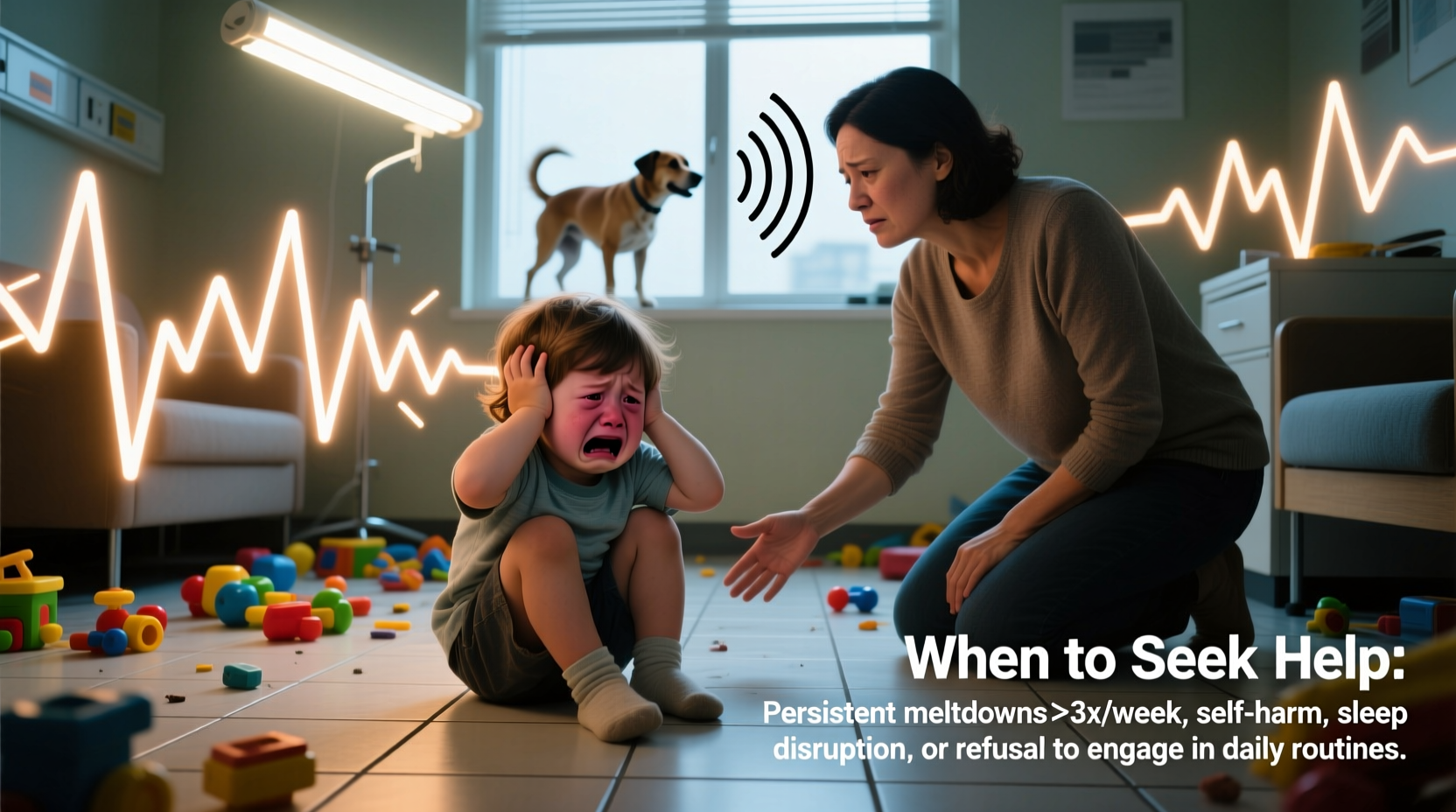
There comes a point when self-management is no longer enough. Recognizing warning signs early can prevent long-term complications such as chronic anxiety, social withdrawal, or functional impairment.
Consider seeking help if:
- Sensory reactions begin interfering with daily tasks like working, studying, or personal care.
- You experience panic attacks, meltdowns, or shutdowns triggered by routine sensory input.
- Symptoms appear suddenly after a head injury, infection, or major life change.
- Current coping strategies stop being effective despite consistent effort.
- There’s a noticeable decline in mental health, including increased irritability, depression, or insomnia.
Professionals who can assist include occupational therapists trained in sensory integration, neurologists, psychologists, and audiologists (for sound sensitivity). Early intervention often leads to better outcomes, especially when therapy is tailored to individual sensory profiles.
Step-by-Step Guide to Seeking Support
- Document symptoms: Record frequency, intensity, and triggers of sensory reactions over two weeks.
- Consult a primary care provider: Rule out medical causes such as thyroid dysfunction, migraines, or vitamin deficiencies.
- Request a referral: Ask for evaluation by an occupational therapist or specialist familiar with sensory processing disorders.
- Begin therapy: Engage in structured programs such as Ayres Sensory Integration® or cognitive-behavioral approaches adapted for sensory regulation.
- Reassess monthly: Track progress and adjust strategies based on feedback from both therapist and personal observation.
Do’s and Don’ts of Sensory Management
| Do | Don’t |
|---|---|
| Create a sensory toolkit (noise-canceling earbuds, fidget tools, sunglasses) | Force exposure to overwhelming stimuli “to get used to it” |
| Maintain consistent sleep and meal schedules | Ignore physical signs of overload (headaches, dizziness, fatigue) |
| Use timers or visual schedules to prepare for transitions | Dismiss reactions as “overreactions” or laziness |
| Practice calming techniques proactively, not just during crises | Rely solely on medication without addressing root causes |
Real-Life Example: Managing Adult-Onset Sensitivity
Mark, a 42-year-old software developer, began experiencing sudden discomfort from office fluorescent lights and keyboard sounds after recovering from a mild concussion. Initially dismissing it as temporary, he found his productivity dropping and anxiety rising within months. Simple tasks became exhausting. After tracking his symptoms, he consulted a neurologist who referred him to an occupational therapist specializing in post-injury sensory rehabilitation.
Through a customized plan involving light filters, scheduled sensory breaks, auditory desensitization exercises, and ergonomic adjustments, Mark regained control. His case highlights that adult-onset sensory issues are valid and treatable—but require timely recognition and expert guidance.
Frequently Asked Questions
Can sensory issues develop in adulthood?
Yes. While often present from childhood, sensory processing challenges can emerge later due to brain injuries, chronic illnesses, hormonal changes, or prolonged stress. Adults may not recognize these as sensory-related until symptoms interfere significantly with daily life.
Is there a test for sensory processing disorder?
There is no single diagnostic test. Evaluation typically involves clinical observation, standardized assessments (like the Sensory Profile 2), and interviews conducted by an occupational therapist. In adults, self-report tools combined with functional analysis are commonly used.
Are sensory issues always linked to autism?
No. Although highly prevalent in autistic individuals, sensory differences exist across various populations—including those with anxiety disorders, PTSD, ADHD, and even neurotypical people under extreme stress. Sensitivity alone does not indicate a broader condition.
Taking Action for Long-Term Relief
Sensory issues don’t have to dictate your quality of life. Whether you're supporting a child, navigating personal challenges, or caring for an aging loved one, understanding the causes of worsening symptoms empowers informed decisions. Effective management blends environmental adjustments, self-awareness, and timely professional input. Progress may be gradual, but small, consistent changes yield meaningful results.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?