Experiencing a weak or sluggish stream during urination is more common than many realize. While occasional changes in urine flow may not be alarming, persistent slow urine flow can signal an underlying health issue that warrants attention. It affects people of all ages and genders, though it's particularly prevalent among older men. Understanding the root causes—and knowing what actions to take—can make a significant difference in both comfort and long-term urinary health.
Understanding Normal vs. Abnormal Urine Flow
Normal urine flow is typically strong, steady, and uninterrupted, lasting around 10 to 20 seconds depending on bladder fullness. A noticeable reduction in force, frequent stopping and starting, or a prolonged time to empty the bladder may indicate a problem. Slow urine flow doesn’t always come with pain, which can lead some individuals to dismiss it as a minor inconvenience. However, it’s often a symptom of obstruction, nerve dysfunction, or muscle weakness affecting the urinary tract.
Urinary flow rate can be objectively measured through a uroflowmetry test, where patients urinate into a special device that records flow speed and volume. A peak flow rate below 15 mL per second in men or 18 mL per second in women is generally considered abnormal and may prompt further investigation.
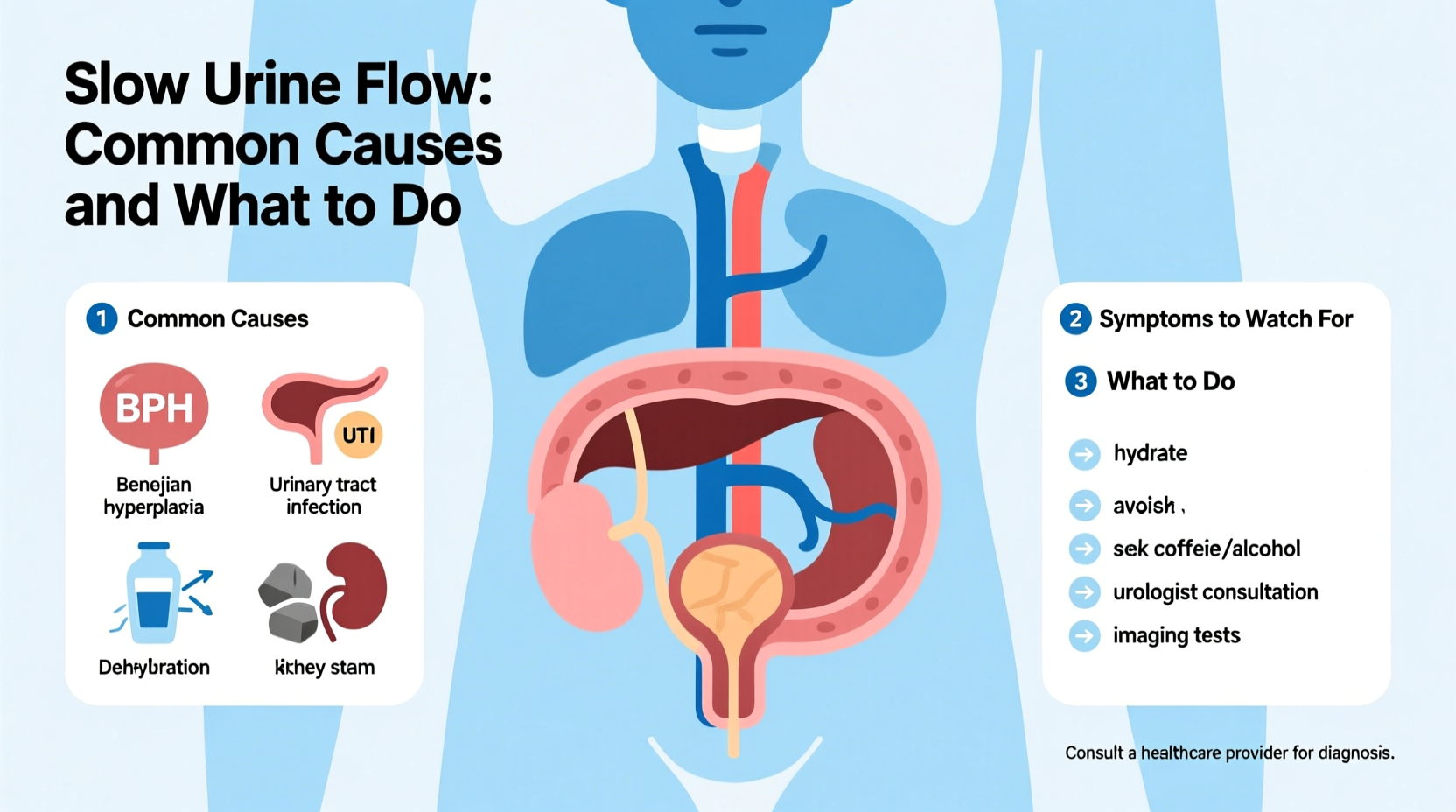
Common Causes of Slow Urine Flow
Several physiological and lifestyle factors can contribute to reduced urine flow. The most frequent causes vary by age, gender, and overall health.
1. Benign Prostatic Hyperplasia (BPH)
In men over 50, an enlarged prostate is the leading cause of slow urine flow. As the prostate gland grows, it compresses the urethra—the tube that carries urine from the bladder—restricting flow. Symptoms often include hesitancy, dribbling, incomplete emptying, and increased nighttime urination.
2. Urinary Tract Infections (UTIs)
Infections in the bladder or urethra can cause inflammation and swelling, narrowing the urinary passage. UTIs are more common in women but can affect men as well. Alongside slow flow, symptoms may include burning, urgency, cloudy urine, and pelvic discomfort.
3. Urethral Strictures
A urethral stricture occurs when scar tissue forms in the urethra, usually due to injury, infection, or prior procedures. This narrowing restricts urine passage and can progressively worsen if untreated.
4. Neurological Conditions
Diseases like multiple sclerosis, Parkinson’s, diabetes-related nerve damage, or spinal cord injuries can interfere with the brain’s ability to signal the bladder muscles properly. This neurogenic bladder dysfunction may result in weak contractions and poor urine expulsion.
5. Bladder Muscle Weakness
Over time, the detrusor muscle (which contracts to expel urine) can weaken, especially in older adults or those with chronic urinary retention. This leads to inefficient emptying and a slow, strained stream.
6. Medications and Lifestyle Factors
Certain drugs—including antihistamines, decongestants, antidepressants, and some blood pressure medications—can affect bladder function. Dehydration, excessive alcohol, and holding urine for long periods also contribute to temporary flow issues.
When to Seek Medical Attention
While mild or temporary changes may resolve on their own, certain red flags require prompt evaluation:
- Pain or burning during urination
- Frequent or urgent need to urinate without relief
- Inability to urinate at all (acute urinary retention)
- Blood in the urine
- Recurrent urinary tract infections
- Numbness or weakness in the legs alongside urinary changes
“Persistent slow urine flow isn’t something to normalize. It can lead to complications like bladder stones, kidney damage, or recurrent infections if left untreated.” — Dr. Alan Reyes, Urologist, Cleveland Clinic
Step-by-Step Guide to Addressing Slow Urine Flow
If you’re experiencing this issue, follow these evidence-based steps to identify and manage the cause:
- Track Your Symptoms: Keep a journal noting frequency, flow strength, pain, and any associated symptoms for at least a week.
- Hydrate Adequately: Drink enough water (about 6–8 glasses daily) to maintain healthy urine dilution and support bladder function.
- Review Medications: Consult your doctor about any drugs you're taking that might affect urination.
- Schedule a Medical Evaluation: See a primary care physician or urologist. They may perform a digital rectal exam (for men), urine analysis, ultrasound, or uroflowmetry.
- Follow Through with Testing: Depending on initial findings, further tests like cystoscopy or post-void residual measurement may be needed.
- Begin Treatment: Whether it’s medication for BPH, antibiotics for infection, or physical therapy for pelvic floor dysfunction, early intervention improves outcomes.
Do’s and Don’ts: Managing Urinary Flow Issues
| Do’s | Don’ts |
|---|---|
| Drink plenty of water throughout the day | Hold urine for extended periods |
| Practice double voiding (urinate, wait, try again) | Consume excessive caffeine or alcohol |
| Perform pelvic floor exercises (Kegels) | Ignore worsening symptoms |
| Follow prescribed treatment plans | Self-medicate with supplements without consulting a doctor |
Real-Life Example: John’s Experience with BPH
John, a 62-year-old teacher, began noticing he had to strain to start urinating and often felt his bladder wasn’t fully empty. At first, he dismissed it as aging. Over six months, the symptoms worsened—he was waking up three to four times nightly and occasionally leaking. After encouragement from his wife, he visited a urologist. Tests revealed moderate BPH with elevated post-void residual volume. He started on tamsulosin, a medication that relaxes prostate muscles, and within three weeks, his flow improved significantly. With regular follow-ups and lifestyle adjustments, John regained confidence and better sleep.
His story underscores the importance of not normalizing urinary changes and seeking timely care.
Natural and Preventive Strategies
While medical treatment is essential for diagnosed conditions, several lifestyle habits support healthy urinary function:
- Pelvic Floor Exercises: Kegel exercises strengthen the muscles involved in bladder control and can improve flow, especially in cases of mild weakness.
- Dietary Adjustments: Reduce intake of bladder irritants like spicy foods, citrus, and artificial sweeteners. Include fiber-rich foods to prevent constipation, which can press on the bladder.
- Maintain a Healthy Weight: Obesity increases abdominal pressure and is linked to urinary symptoms, especially in men with prostate issues.
- Avoid Smoking: Chronic coughing from smoking can weaken pelvic muscles and worsen urinary control.
FAQ
Can slow urine flow go away on its own?
Sometimes, if caused by temporary factors like dehydration or a mild UTI, flow may return to normal after addressing the trigger. However, structural or progressive issues like BPH or strictures typically require treatment and won’t resolve independently.
Is slow urine flow a sign of prostate cancer?
Not necessarily. While prostate enlargement is common in older men, slow flow is more often due to benign prostatic hyperplasia (BPH). However, your doctor may check PSA levels or perform imaging to rule out cancer if risk factors are present.
Are there home remedies that help?
Staying hydrated, avoiding bladder irritants, and doing pelvic floor exercises can support improvement. However, they should complement—not replace—professional diagnosis and treatment, especially if symptoms persist beyond a few days.
Conclusion: Take Control of Your Urinary Health
Slow urine flow is not just a nuisance—it’s a signal from your body that something may need attention. Whether it’s a treatable infection, a manageable prostate condition, or a neurological concern, early action prevents complications and improves quality of life. Don’t downplay changes in how you urinate. By understanding the causes, tracking your symptoms, and working with a healthcare provider, you can restore normal function and maintain long-term urinary wellness.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?