Mucus in stool is more common than many people realize. While a small amount is normal, seeing noticeable, stringy, or colored mucus—especially if it looks like snot mixed with feces—can be alarming. Unlike stool discoloration or occasional bloating, visible mucus may signal irritation or inflammation in the digestive tract. Understanding what’s behind this symptom can help distinguish between harmless fluctuations and conditions requiring medical attention.
The digestive system naturally produces mucus to lubricate the intestines and protect the lining from digestive enzymes and bacteria. However, when excess mucus appears consistently or is accompanied by pain, diarrhea, or blood, it may point to an underlying issue such as infection, inflammatory bowel disease (IBD), or irritable bowel syndrome (IBS). This article explores the science behind mucus in stool, identifies potential causes, and provides practical guidance on when to seek care.
Why Does the Body Produce Mucus in the Gut?
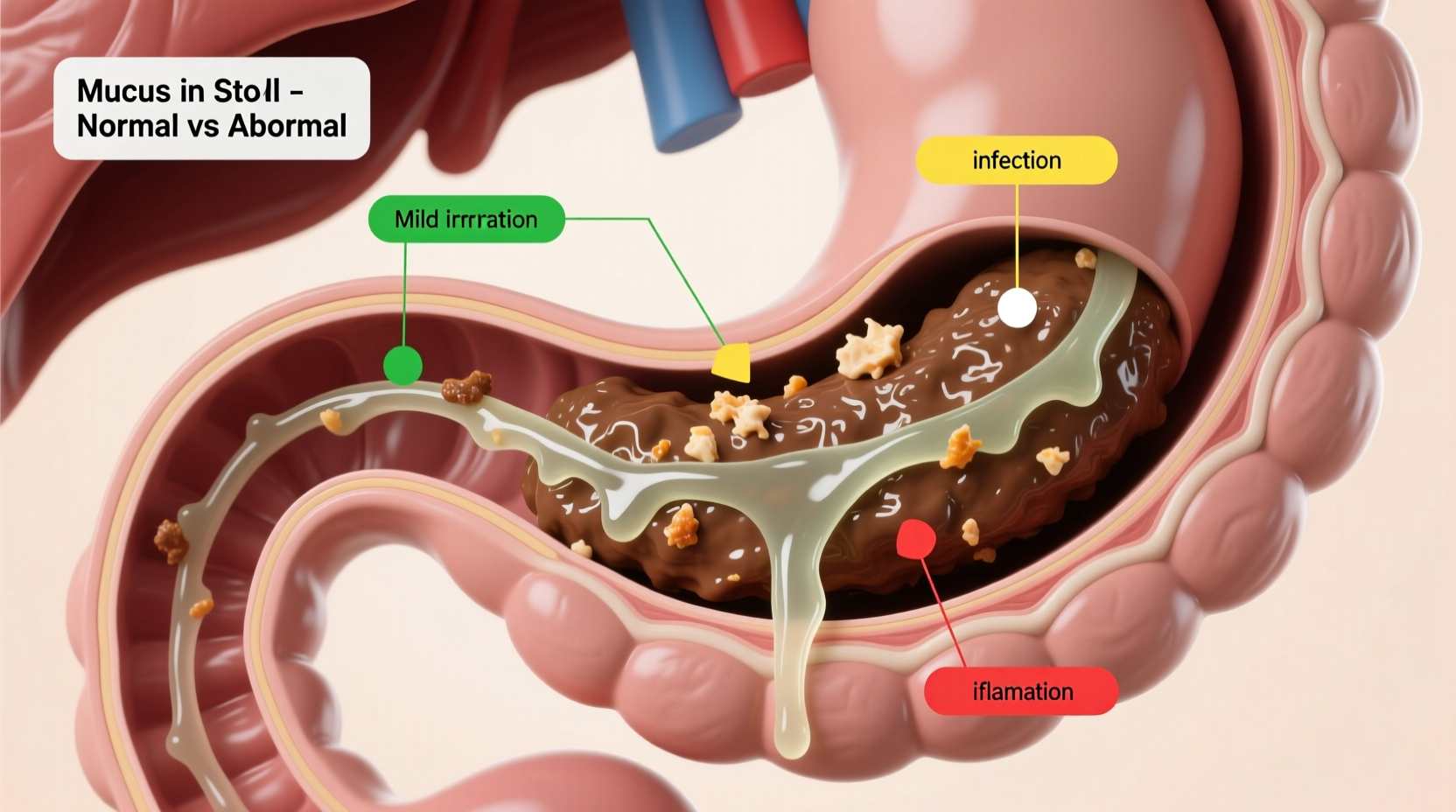
The gastrointestinal tract is lined with mucous membranes that secrete mucus to keep the colon moist and facilitate smooth passage of stool. Goblet cells, specialized cells in the intestinal lining, are responsible for this production. In healthy individuals, mucus is typically clear or white and not easily noticeable in bowel movements.
When the gut is irritated or inflamed, goblet cells may go into overdrive, producing larger amounts of mucus. This excess can appear as:
- Clear, jelly-like strands
- White or yellowish clumps
- Tan or pink-tinged mucus (if mixed with blood)
In some cases, mucus may coat the stool entirely or appear separately during wiping. The texture often resembles nasal mucus—hence the unsettling comparison to “snot”—but its presence in the digestive system has different implications.
“Mucus alone isn’t diagnostic, but it’s a signpost. It tells us the gut lining is reacting to something—whether it’s infection, food sensitivity, or chronic inflammation.” — Dr. Lena Patel, Gastroenterology Specialist, Cleveland Clinic
Common Causes of Mucus in Stool
Not all mucus in stool indicates serious illness. Several benign and treatable conditions can lead to increased mucus production. Below are the most frequent causes, ranging from mild to more complex.
Dietary Triggers and Minor Irritations
Sudden dietary changes, excessive spicy foods, or high-fat meals can irritate the intestinal lining. Artificial sweeteners like sorbitol and lactose in dairy products may also cause temporary mucus secretion, especially in sensitive individuals.
Bacterial or Parasitic Infections
Infections such as Salmonella, Shigella, or Campylobacter often cause inflammation in the colon, leading to mucus and diarrhea. These infections are usually acute, lasting several days, and may include fever, cramping, and nausea.
Parasites like Giardia lamblia can also trigger persistent mucus discharge, especially after travel or exposure to contaminated water.
Irritable Bowel Syndrome (IBS)
IBS is a functional disorder affecting up to 15% of the global population. One hallmark symptom is mucus in stool, particularly in the subtype known as IBS with diarrhea (IBS-D). Stress, certain carbohydrates (FODMAPs), and hormonal shifts can exacerbate symptoms.
Unlike inflammatory conditions, IBS does not cause tissue damage, but it can significantly impact quality of life.
Inflammatory Bowel Disease (IBD)
Chronic conditions like Crohn’s disease and ulcerative colitis involve immune-mediated inflammation of the digestive tract. Mucus is frequently present, often mixed with blood or pus. Other symptoms include:
- Abdominal pain
- Unintentional weight loss
- Frequent urgent bowel movements
Ulcerative colitis specifically affects the colon and rectum, where mucus production increases dramatically due to ulcerated tissue.
Anal Fissures or Hemorrhoids
Structural issues near the anus, such as fissures (small tears) or internal hemorrhoids, can stimulate mucus secretion as a protective response. This mucus may appear after bowel movements and is sometimes mistaken for stool contamination.
When to Be Concerned: Red Flags to Watch For
Occasional mucus without other symptoms is usually not dangerous. However, certain signs warrant prompt medical evaluation. The following table outlines key indicators and their possible implications.
| Symptom | Possible Cause | Action Recommended |
|---|---|---|
| Mucus with bright red blood | Hemorrhoids, IBD, colorectal polyps | See doctor within 1–2 weeks |
| Chronic mucus + diarrhea (>2 weeks) | IBS, infection, malabsorption | Consult gastroenterologist |
| Mucus with abdominal pain and weight loss | Possible IBD or malignancy | Seek immediate evaluation |
| Cloudy or foul-smelling mucus | Bacterial overgrowth or infection | Stool test recommended |
Diagnostic Steps and What to Expect
If mucus in stool persists beyond a few days or occurs with other symptoms, a healthcare provider may recommend diagnostic testing. The process typically follows a stepwise approach:
- Medical History Review: Your doctor will ask about diet, bowel habits, travel history, medications, and family history of gastrointestinal diseases.
- Physical Examination: Includes abdominal palpation and possibly a digital rectal exam to check for hemorrhoids or masses.
- Stool Tests: To detect infection, white blood cells, or occult (hidden) blood.
- Blood Work: Inflammatory markers like CRP or ESR can indicate systemic inflammation.
- Imaging or Endoscopy: A colonoscopy may be advised if IBD or cancer is suspected, especially in patients over 50 or with risk factors.
Early diagnosis is crucial. For example, untreated ulcerative colitis can increase the risk of colon cancer over time. Conversely, identifying IBS early allows for targeted dietary and lifestyle interventions that improve long-term outcomes.
Mini Case Study: Recognizing the Pattern
Sarah, a 34-year-old teacher, began noticing slimy, clear mucus in her stool after returning from a trip to Southeast Asia. Initially, she dismissed it as food-related. But after two weeks of ongoing mucus, bloating, and loose stools, she consulted her primary care physician.
A stool test revealed Giardia lamblia. With a course of metronidazole and rehydration support, her symptoms resolved within ten days. Follow-up testing confirmed eradication of the parasite. Sarah’s case highlights how travel-related infections can manifest subtly and why timely testing matters—even when symptoms seem minor at first.
Managing and Reducing Mucus Production
Depending on the cause, strategies to reduce mucus vary. Here’s a checklist of actionable steps based on common triggers:
Checklist: Responding to Mucus in Stool
- ✅ Monitor frequency and appearance for 3–5 days
- ✅ Eliminate potential irritants (spicy foods, alcohol, dairy)
- ✅ Stay hydrated, especially if diarrhea is present
- ✅ Avoid laxatives unless prescribed
- ✅ Schedule a doctor’s visit if symptoms persist beyond a week
- ✅ Request a stool culture if infection is suspected
For those with diagnosed IBS, a low-FODMAP diet under the guidance of a registered dietitian can significantly reduce mucus and other symptoms. Probiotics may also help restore gut balance, though evidence remains mixed.
Frequently Asked Questions
Is mucus in stool always a sign of something serious?
No. Small amounts of clear mucus are normal. However, consistent, visible, or bloody mucus should be evaluated, especially if paired with pain, weight loss, or changes in bowel habits.
Can stress cause mucus in stool?
Indirectly, yes. Stress doesn’t produce mucus directly but can worsen conditions like IBS, which increases mucus secretion. Managing stress through mindfulness or therapy may reduce flare-ups.
Should I collect a stool sample for the doctor?
If your provider requests one, use the sterile container provided. Do not store stool at room temperature for more than an hour. Refrigeration (not freezing) is acceptable for short delays.
Conclusion: Listen to Your Body
Seeing mucus in your stool—especially if it resembles snot—can be unsettling, but it’s not inherently dangerous. The body uses mucus as a defense mechanism, and its presence often reflects a temporary reaction to food, infection, or stress. However, ignoring persistent changes can delay diagnosis of conditions like IBD or infections that require treatment.
The key is awareness without alarm. Track your symptoms, adjust your diet mindfully, and consult a healthcare professional when red flags appear. Your digestive health is a vital component of overall well-being, and paying attention to subtle signals like mucus can lead to earlier intervention and better outcomes.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?