A sore throat is a common complaint, often dismissed as a minor cold symptom. But when the pain is isolated to just one side, it can signal something more specific than a typical viral infection. While many cases resolve on their own, unilateral sore throat may point to infections, inflammation, or even structural issues requiring medical evaluation. Understanding the underlying causes, recognizing red flags, and knowing when to seek help are essential for effective recovery and avoiding complications.
Common Causes of a One-Sided Sore Throat
Pain localized to one side of the throat isn’t always due to a simple virus. Several conditions can lead to this asymmetry:
- Tonsillitis: Inflammation of one tonsil (unilateral tonsillitis) often results in sharp, one-sided pain, difficulty swallowing, and visible redness or white patches.
- Peritonsillar abscess: A pus-filled pocket near the tonsil, typically arising from untreated tonsillitis. This condition causes severe, worsening pain on one side, muffled voice (\"hot potato voice\"), and sometimes trismus (difficulty opening the mouth).
- Pharyngitis: Viral or bacterial infections like strep throat can occasionally present asymmetrically, especially in early stages.
- Dental or sinus infections: Referred pain from an infected tooth or maxillary sinusitis may radiate to the throat on one side.
- Tonsil stones (tonsilloliths): Calcified debris trapped in tonsil crypts can cause irritation, bad breath, and persistent discomfort on one side.
- Vocal strain or injury: Overuse, shouting, or accidental trauma (e.g., from eating hard food) can inflame one side of the throat.
- Tumors: Though rare, persistent unilateral sore throat lasting more than two weeks without clear cause should be evaluated for malignancy, especially in individuals with risk factors like smoking or heavy alcohol use.
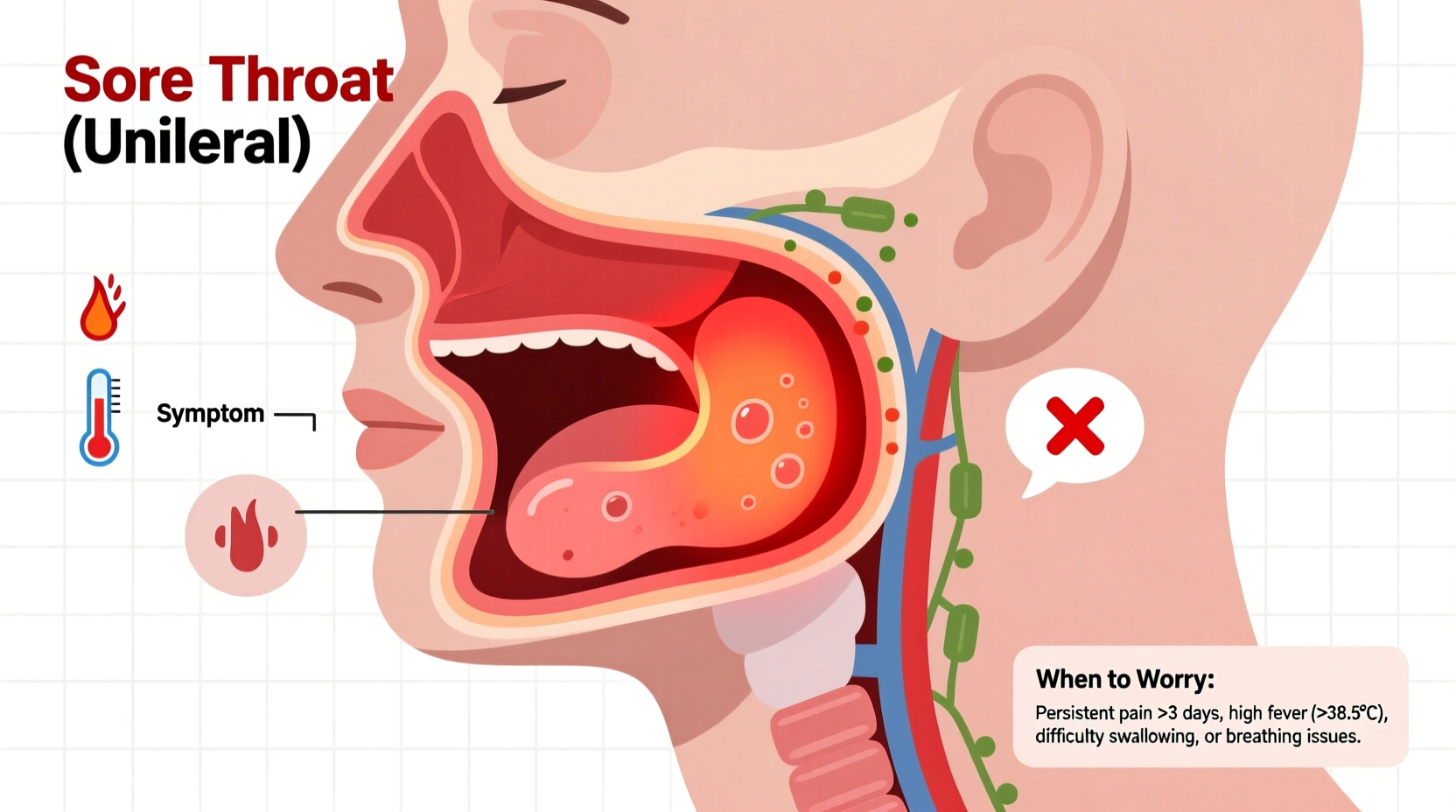
Symptoms That Accompany One-Sided Throat Pain
The nature and combination of symptoms help differentiate between mild and serious conditions. Common accompanying signs include:
- Difficulty or painful swallowing (odynophagia)
- Swollen lymph nodes on the same side of the neck
- Fever or chills
- White or yellow coating on one tonsil
- Hoarseness or voice changes
- Ear pain on the affected side (referred via shared nerves)
- Bad breath (halitosis), particularly with tonsil stones
- Headache or facial pressure (if sinus-related)
In more severe cases, such as peritonsillar abscess, patients may experience:
- Trismus — inability to open the mouth fully
- Drooling due to pain when swallowing saliva
- Visible swelling pushing the uvula toward the unaffected side
- Muffled or distorted speech
When to Worry: Red Flags Requiring Medical Attention
Most sore throats improve within a few days. However, certain symptoms suggest a need for prompt medical evaluation. Delaying care in these instances can lead to complications like airway obstruction or systemic infection.
“Unilateral throat pain that worsens over 2–3 days, especially with difficulty opening the mouth or breathing, should never be ignored. It could indicate a deep neck space infection.” — Dr. Lena Patel, Otolaryngologist
| Symptom | What It Might Indicate | Action Required |
|---|---|---|
| Severe pain worsening over 24–48 hours | Possible abscess or deep tissue infection | See a doctor within 24 hours |
| Inability to open mouth fully (trismus) | Peritonsillar abscess likely | Urgent ENT evaluation needed |
| Difficulty breathing or swallowing saliva | Impending airway compromise | Go to ER immediately |
| Fever above 102°F (39°C) | Systemic bacterial infection | Medical assessment recommended |
| Symptoms persisting beyond 7–10 days | Chronic infection or tumor possibility | Follow-up with primary care or ENT |
Step-by-Step Guide: What to Do If You Have a One-Sided Sore Throat
Not every sore throat requires emergency care, but taking structured steps helps manage symptoms and determine if professional help is needed.
- Monitor Onset and Progression: Note when the pain started, whether it’s constant or intermittent, and if any triggers (like eating or talking) make it worse.
- Check for Fever: Use a thermometer twice daily. A rising temperature suggests active infection.
- Inspect Your Throat: Use a flashlight and mirror. Look for redness, swelling, white patches, or deviation of the uvula.
- Try Symptomatic Relief: Gargle salt water, stay hydrated, use lozenges, and take OTC pain relievers like ibuprofen.
- Assess for Red Flags: Be vigilant for trismus, drooling, voice changes, or breathing issues.
- Contact a Healthcare Provider: If symptoms persist beyond 3 days or worsen, schedule an appointment. Rapid strep tests, throat cultures, or imaging may be necessary.
- Seek Emergency Care: If you experience trouble breathing, high fever with rigors, or inability to swallow liquids, go to the ER.
Real-Life Example: Recognizing a Peritonsillar Abscess
Jamal, a 24-year-old graduate student, noticed a sore throat on his right side after a week of fatigue and mild congestion. He assumed it was a cold. By day three, the pain intensified sharply, making it hard to eat or sleep. He began speaking oddly—his words sounded thick—and realized he couldn’t open his mouth fully. When he checked in the mirror, his uvula was visibly pushed to the left.
Concerned, he visited an urgent care clinic. The physician diagnosed a peritonsillar abscess and referred him immediately to an ENT specialist. Jamal received drainage of the abscess and a course of antibiotics. His recovery took about a week, but early intervention prevented life-threatening complications.
This case highlights how quickly a seemingly routine sore throat can escalate—and why recognizing asymmetry and functional limitations is crucial.
Prevention and Self-Care Checklist
While not all causes of one-sided sore throat are preventable, these habits reduce your risk and support faster healing:
- ✅ Practice good hand hygiene to avoid viral and bacterial infections
- ✅ Stay hydrated to keep mucous membranes moist and resilient
- ✅ Avoid smoking and excessive alcohol, which irritate the throat lining
- ✅ Treat dental issues promptly to prevent spread of infection
- ✅ Use a humidifier during dry seasons to prevent throat irritation
- ✅ Seek treatment early for recurrent tonsillitis; chronic cases may benefit from tonsillectomy
Frequently Asked Questions
Can allergies cause a sore throat on one side?
Allergies typically cause bilateral throat irritation due to postnasal drip. A truly one-sided sore throat is unlikely to be allergy-related unless accompanied by uneven sinus congestion or dental involvement.
Is a sore throat on one side always a sign of strep?
No. While strep throat can sometimes appear asymmetrically, it usually affects both sides. Strep is also commonly associated with fever, absence of cough, and swollen anterior neck nodes. A rapid test is needed for confirmation.
How long should a one-sided sore throat last before seeing a doctor?
If the pain persists beyond 5–7 days, worsens, or is accompanied by fever, difficulty swallowing, or lumps in the neck, consult a healthcare provider. Persistent unilateral symptoms warrant evaluation to rule out abscess or malignancy.
Final Thoughts: Don’t Ignore Asymmetry
The body often communicates severity through patterns. A sore throat affecting only one side breaks the usual symmetry of common infections and deserves closer attention. While many cases stem from treatable conditions like tonsillitis or tonsil stones, others—such as abscesses or tumors—require timely diagnosis and intervention.
Listening to your body, tracking symptoms accurately, and acting decisively when warning signs appear can prevent minor discomfort from becoming a major health issue. If in doubt, err on the side of caution and consult a medical professional.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?