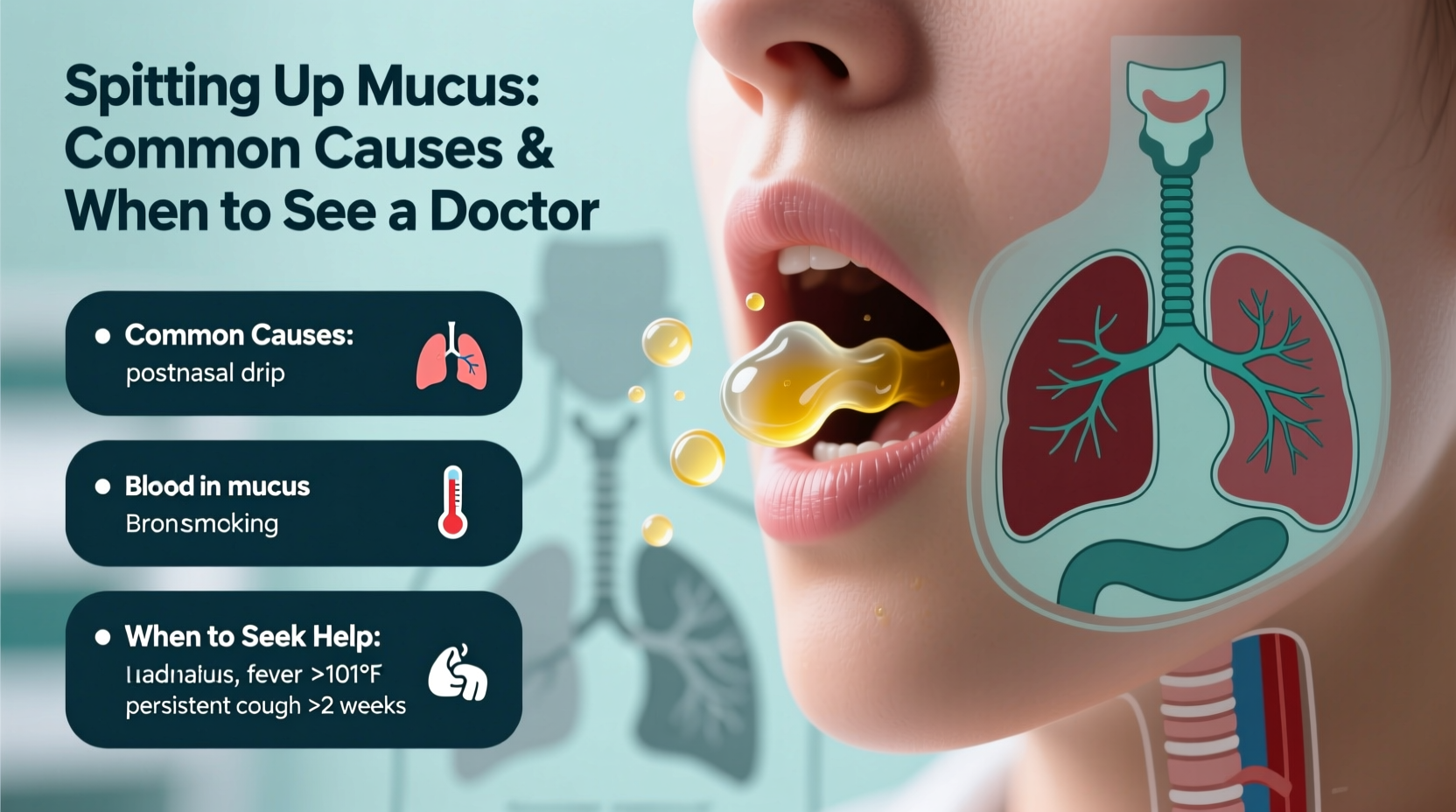
Spitting up mucus is a symptom many people experience at some point, often without serious concern. Mucus plays a vital role in protecting your respiratory system by trapping dust, bacteria, and allergens. However, when excess mucus accumulates and is expelled through coughing or spitting, it can signal an underlying condition. Understanding the root causes—and knowing when to seek medical advice—is essential for maintaining respiratory health and preventing complications.
What Is Mucus and Why Does the Body Produce It?
Mucus is a slippery, viscous substance produced by mucous membranes lining the nose, throat, lungs, and sinuses. Its primary function is to keep these tissues moist and act as a defensive barrier against pathogens. Under normal conditions, you swallow small amounts of mucus daily without noticing. But during illness or irritation, production increases, leading to noticeable buildup and the urge to spit or cough it up.
The color and consistency of mucus can offer clues about your health. Clear mucus is typically normal, while yellow or green may suggest infection. Brown or bloody mucus warrants closer attention and possibly medical evaluation.
Common Causes of Spitting Up Mucus
Several factors can trigger increased mucus production and lead to spitting it up. Most are benign and resolve on their own, but others may require treatment.
1. Viral Respiratory Infections
Colds and flu are among the most frequent causes. These infections inflame the nasal passages and bronchial tubes, prompting the body to produce more mucus to trap and expel viruses. Symptoms usually peak within a few days and improve over one to two weeks.
2. Allergic Rhinitis
Seasonal or environmental allergies (to pollen, dust, or pet dander) cause the immune system to overreact, leading to postnasal drip—mucus that drips down the back of the throat. This often results in a chronic need to clear the throat or spit.
3. Sinusitis
When sinuses become inflamed due to infection or blockage, mucus thickens and drains into the throat. Acute sinusitis typically lasts less than four weeks; chronic cases persist beyond 12 weeks and may require antibiotics or specialist care.
4. Bronchitis
Inflammation of the bronchial tubes, often following a cold, leads to excessive mucus production in the lungs. Coughing up phlegm—sometimes yellow or green—is common. Most cases are viral and resolve with rest and hydration.
5. Gastroesophageal Reflux Disease (GERD)
Acid reflux can irritate the throat and stimulate mucus production as a protective response. Some people mistake this for a respiratory issue, but heartburn, regurgitation, and a sour taste in the mouth are telltale signs of GERD.
6. Smoking and Environmental Irritants
Tobacco smoke, air pollution, strong fumes, and dry air can all irritate the respiratory tract, increasing mucus production. Smokers often experience a “smoker’s cough” with morning mucus due to cilia damage in the lungs.
“Persistent mucus production, especially if discolored or accompanied by breathing difficulties, should never be ignored. It’s the body’s way of signaling that something needs attention.” — Dr. Lena Patel, Pulmonologist
When to See a Doctor: Warning Signs
While occasional mucus expulsion is normal, certain symptoms indicate the need for professional evaluation. Seek medical advice if you experience any of the following:
- Coughing up blood or rust-colored sputum
- Fever lasting more than three days
- Shortness of breath or wheezing
- Unexplained weight loss or fatigue
- Symptoms lasting longer than three weeks without improvement
- Swelling in the face or neck
These could point to more serious conditions such as pneumonia, bronchiectasis, tuberculosis, or even lung cancer. Early diagnosis significantly improves outcomes.
Table: Common Mucus Colors and What They Might Mean
| Mucus Color | Likely Cause | Action Recommended |
|---|---|---|
| Clear | Allergies, early cold, or normal production | Monitor; increase fluids if symptomatic |
| White | Viral infection, congestion, or GERD | Rest, hydration; consider antacids if reflux suspected |
| Yellow or Green | Bacterial or viral infection (e.g., sinusitis, bronchitis) | See doctor if persistent beyond 10 days |
| Brown or Tan | Smoking, inhaled dirt, or old blood | Discontinue smoking; consult if recurrent |
| Pink or Red | Blood from nose/throat irritation or lung issues | Seek immediate medical attention if heavy or ongoing |
Step-by-Step Guide to Managing Mucus at Home
For mild cases, self-care strategies can reduce discomfort and speed recovery. Follow this timeline to manage symptoms effectively:
- Day 1–2: Increase fluid intake—warm herbal teas, broths, and water help thin mucus. Avoid caffeine and alcohol, which can dehydrate.
- Day 3–5: Use a humidifier to add moisture to the air, especially at night. Saline nasal sprays or neti pots can clear nasal passages and reduce postnasal drip.
- Day 6–7: If symptoms persist, try over-the-counter expectorants like guaifenesin to loosen mucus. Decongestants may help but should not be used long-term.
- After Day 7: Reassess. If mucus remains thick, discolored, or is worsening, schedule a visit with your healthcare provider.
Mini Case Study: Recognizing Chronic Bronchitis Early
Sarah, a 52-year-old office worker and former smoker, began noticing she was spitting up mucus every morning. At first, she dismissed it as seasonal allergies. Over several months, the mucus became thicker and yellowish, and she developed shortness of breath during light activity. After delaying a doctor’s visit for six months, she was diagnosed with chronic bronchitis—a form of COPD. With medication, pulmonary rehab, and lifestyle changes, her symptoms improved. Her case highlights the danger of ignoring persistent mucus production, especially in those with a smoking history.
Checklist: When to Take Action
Use this checklist to determine whether home care is sufficient or if medical evaluation is needed:
- ☐ Mucus has persisted for more than 3 weeks
- ☐ Cough produces blood or rust-colored phlegm
- ☐ Fever above 101°F (38.3°C) lasts over 3 days
- ☐ Breathing feels labored or tight
- ☐ Voice changes or throat pain worsens
- ☐ Unexplained fatigue or weight loss occurs
- ☐ You have a history of smoking or lung disease
If you check two or more items, consult a healthcare provider promptly.
Frequently Asked Questions
Is spitting up mucus always a sign of infection?
No. While infections are a common cause, mucus can also increase due to allergies, acid reflux, dry air, or irritants like smoke. Clear mucus without fever or fatigue is often non-infectious.
Can drinking milk increase mucus production?
Research shows milk does not increase mucus volume, though it may thicken existing mucus, creating a temporary sensation of congestion. People with lactose intolerance or dairy sensitivities might experience more noticeable symptoms.
Should I use a cough suppressant when spitting up mucus?
Generally, no. Suppressing a productive cough can trap mucus in the lungs. Expectorants are preferred because they help clear the airways. Reserve cough suppressants for dry, non-productive coughs, especially at night.
Conclusion: Listen to Your Body
Spitting up mucus is often a temporary response to minor illness or environmental triggers. With proper hydration, rest, and simple remedies, most cases resolve without intervention. However, dismissing persistent or severe symptoms can delay diagnosis of conditions like chronic bronchitis, asthma, or infections requiring antibiotics. Pay attention to changes in color, volume, and accompanying symptoms. Your body uses mucus as a messenger—learn to interpret its signals.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?