Experiencing stomach pain after eating is more common than many realize, but it shouldn't be ignored. While occasional discomfort may stem from simple overeating or spicy foods, recurring or severe pain can signal underlying digestive conditions. Understanding the potential causes and knowing when to seek medical attention are crucial steps in protecting your long-term health.
Common Causes of Post-Meal Stomach Pain
Stomach pain after eating can arise from a variety of sources, ranging from dietary choices to chronic gastrointestinal disorders. The location, timing, and nature of the pain often provide clues about its origin.
- Dyspepsia (Indigestion): A general term for upper abdominal discomfort, bloating, or burning that occurs during or shortly after meals. Often linked to eating too quickly, consuming fatty or spicy foods, or stress.
- Gastritis: Inflammation of the stomach lining, commonly caused by bacterial infection (H. pylori), excessive alcohol use, or prolonged use of NSAIDs like ibuprofen.
- Gastroesophageal Reflux Disease (GERD): Stomach acid flows back into the esophagus, causing heartburn, regurgitation, and sometimes upper abdominal pain after eating.
- Lactose Intolerance: Inability to digest lactose, the sugar found in milk and dairy products, leading to gas, bloating, cramps, and diarrhea within hours of consumption.
- Irritable Bowel Syndrome (IBS): A functional disorder affecting the large intestine, often triggered by certain foods and resulting in cramping, bloating, diarrhea, or constipation.
- Gallbladder Issues: Gallstones or inflammation can cause sharp pain in the upper right abdomen, typically occurring 30 minutes to an hour after a fatty meal.
- Pancreatitis: Inflammation of the pancreas, which may present as severe upper abdominal pain radiating to the back, worsened by eating—especially high-fat foods.
- Celiac Disease: An autoimmune reaction to gluten that damages the small intestine, causing bloating, diarrhea, fatigue, and malnutrition.
When to Seek Medical Help: Warning Signs
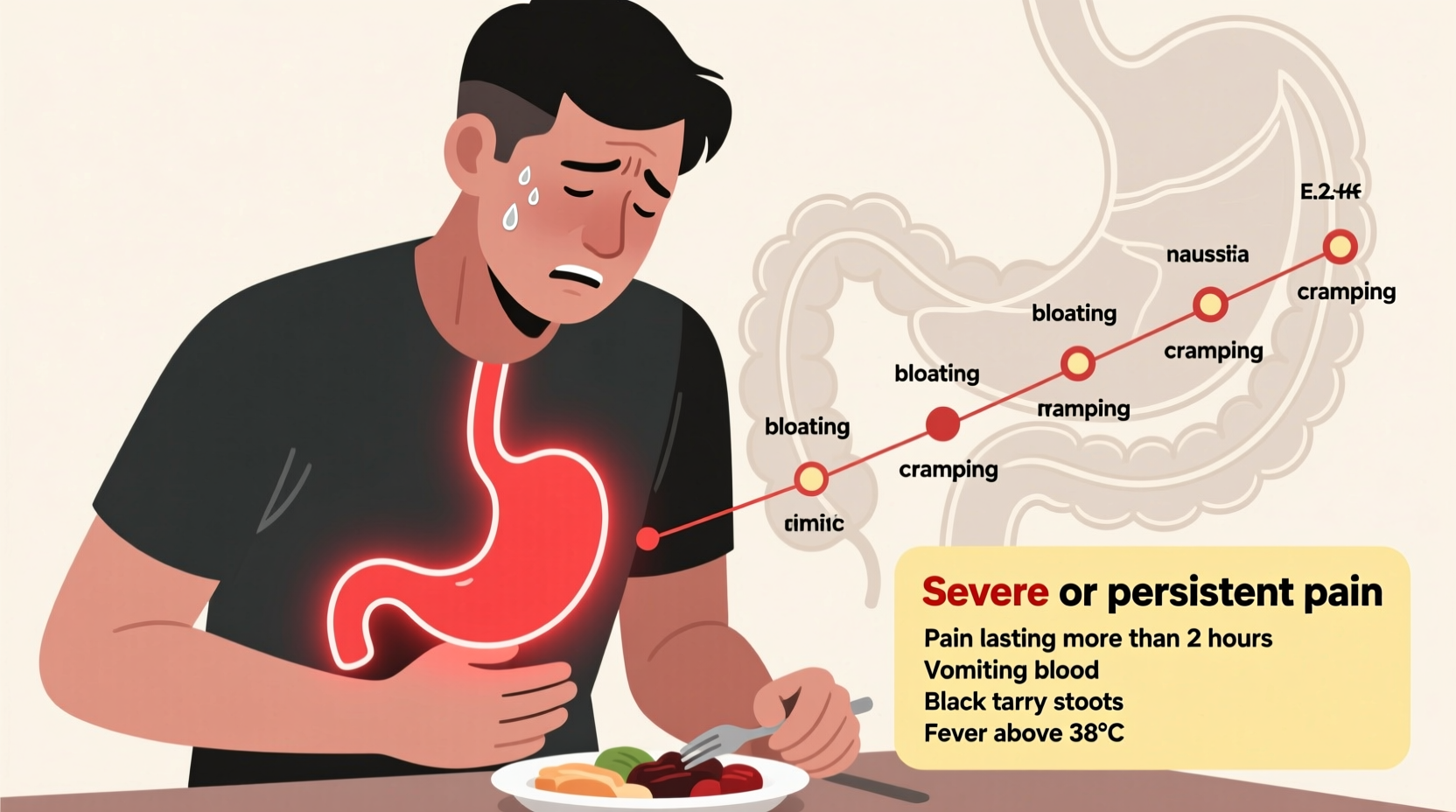
While mild post-meal discomfort may resolve on its own, certain symptoms indicate the need for prompt medical evaluation. Ignoring these red flags can lead to complications or delayed treatment of serious conditions.
“Persistent abdominal pain after eating isn’t something to brush off. If it interferes with daily life or is accompanied by weight loss or bleeding, it’s time to see a doctor.” — Dr. Lena Torres, Gastroenterologist
Symptoms That Require Immediate Attention
Seek emergency care if you experience any of the following:
- Severe, sudden abdominal pain that doesn’t improve
- Chest pain or pressure (could indicate heart issues)
- Vomiting blood or material that looks like coffee grounds
- Black, tarry stools (a sign of gastrointestinal bleeding)
- Fever with abdominal pain
- Pain that spreads to the shoulder, neck, or jaw
- Inability to pass gas or have a bowel movement (possible bowel obstruction)
Non-Emergency But Concerning Symptoms
Schedule a doctor’s visit if you notice:
- Pain that recurs frequently after meals
- Unintentional weight loss
- Persistent nausea or vomiting
- Difficulty swallowing
- Anemia or fatigue without clear cause
- Family history of gastrointestinal cancers
Diagnostic Process: What to Expect
If your symptoms persist, your healthcare provider will likely begin with a thorough medical history and physical exam. Based on initial findings, further testing may include:
| Test | Purpose | What It Detects |
|---|---|---|
| Blood Tests | Check for infection, inflammation, anemia, liver or pancreatic function | Anemia, H. pylori, elevated enzymes |
| Stool Tests | Look for hidden blood, infections, or malabsorption | Bleeding, parasites, C. difficile |
| Endoscopy | Visual examination of the esophagus, stomach, and duodenum | Ulcers, gastritis, Barrett’s esophagus, tumors |
| Abdominal Ultrasound | Imaging of gallbladder and liver | Gallstones, inflammation |
| CT Scan or MRI | Detailed imaging of abdominal organs | Pancreatitis, tumors, obstructions |
| Hydrogen Breath Test | Measures gas produced after ingesting specific sugars | Lactose intolerance, SIBO |
Step-by-Step Guide to Managing Mild Post-Meal Discomfort
For occasional, non-severe stomach pain, try this structured approach before assuming the worst:
- Pause and assess: Note when the pain started, its location, duration, and whether it’s related to a specific food.
- Modify eating habits: Eat smaller portions, chew thoroughly, and avoid lying down immediately after meals.
- Eliminate common triggers: Temporarily avoid alcohol, caffeine, spicy foods, dairy, or high-fat meals.
- Try over-the-counter remedies: Antacids for heartburn, simethicone for gas, or probiotics for bloating (if no fever or bleeding).
- Monitor response: Track symptoms for 3–5 days. If improvement occurs, reintroduce foods slowly to identify culprits.
- Consult a professional: If no improvement or symptoms worsen, schedule a visit with your primary care provider or gastroenterologist.
Real-Life Example: Recognizing a Hidden Condition
Sarah, a 42-year-old teacher, began experiencing dull upper abdominal pain about 20 minutes after eating dinner. At first, she assumed it was due to her new habit of eating late-night takeout. She tried antacids and cut back on spicy food, but the pain persisted for three weeks. She also noticed unexplained fatigue and slight yellowing of her eyes.
After reading about gallbladder symptoms online, she scheduled a visit with her doctor. An ultrasound revealed multiple gallstones blocking her bile duct. She underwent a laparoscopic cholecystectomy and recovered fully within two weeks. Her case highlights how seemingly minor digestive symptoms can mask serious conditions—and why timely evaluation matters.
Prevention and Long-Term Strategies
While not all causes of stomach pain can be prevented, adopting healthy eating and lifestyle habits reduces risk and improves digestive resilience.
Dietary Adjustments That Help
- Eat slowly and mindfully to aid digestion and prevent overeating.
- Limit processed foods, refined sugars, and trans fats.
- Incorporate fiber-rich fruits, vegetables, and whole grains gradually.
- Avoid carbonated beverages that contribute to bloating.
- Consider eliminating common irritants: gluten, dairy, or artificial sweeteners—under guidance if needed.
Lifestyle Factors
- Manage stress through mindfulness, yoga, or therapy—chronic stress disrupts gut function.
- Maintain a healthy weight; excess abdominal fat increases pressure on the stomach.
- Avoid smoking and limit alcohol, both of which irritate the digestive tract.
- Exercise regularly to support healthy bowel motility.
Frequently Asked Questions
Can stress really cause stomach pain after eating?
Yes. Stress activates the “fight-or-flight” response, which can slow digestion, increase stomach acid production, and heighten pain sensitivity. Many people with IBS report symptom flare-ups during stressful periods, even when diet remains unchanged.
Is it normal to feel bloated after every meal?
Occasional bloating is common, especially after large or gas-producing meals (like beans or cruciferous vegetables). However, consistent bloating after most meals—especially with pain, weight loss, or changes in bowel habits—should be evaluated by a doctor.
How soon after eating should pain be concerning?
Pain that starts within minutes may point to GERD, gastritis, or gallbladder issues. Delayed pain (1–3 hours post-meal) could suggest peptic ulcers or pancreatic problems. Timing alone isn’t diagnostic, but patterns help guide investigation.
Final Thoughts: Listen to Your Body
Your digestive system communicates through symptoms. Occasional discomfort after a rich meal is normal, but recurring pain is your body’s way of signaling imbalance or disease. Early intervention can prevent complications like ulcers, malnutrition, or chronic inflammation.
Whether adjusting your diet, managing stress, or seeking medical advice, taking proactive steps today can lead to lasting relief. Don’t normalize persistent pain—your long-term well-being depends on paying attention now.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?