Many people assume that pushing hard during a bowel movement is normal or even necessary. In reality, excessive straining can lead to serious health complications over time. From hemorrhoids to pelvic floor dysfunction, the consequences are more common—and preventable—than most realize. Understanding why straining happens and how to promote natural, effortless elimination is essential for long-term digestive and overall health.
The Hidden Dangers of Straining During Bowel Movements
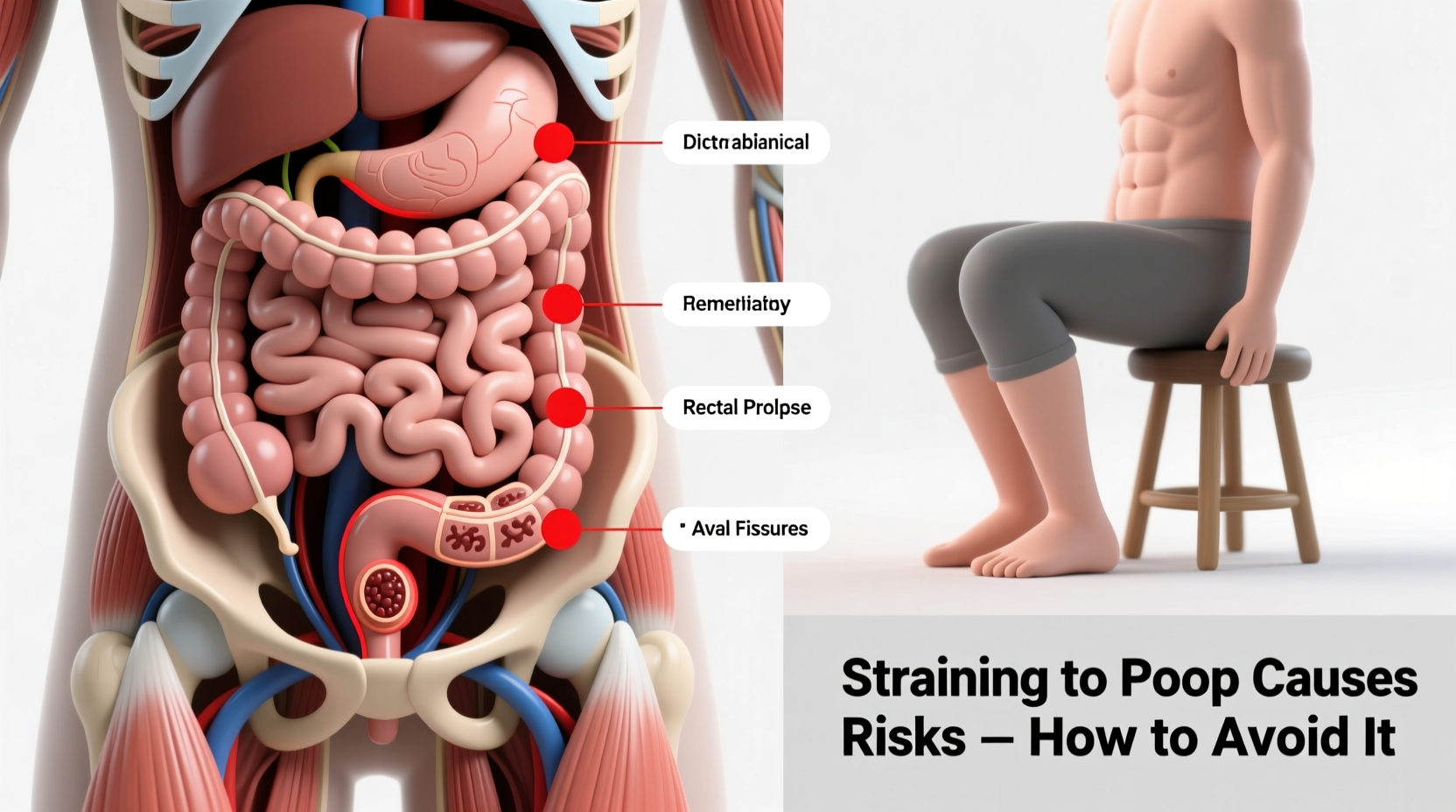
When you push too hard to pass stool, pressure builds in the rectal and abdominal areas. This increased intra-abdominal pressure affects blood vessels, muscles, and nerves involved in digestion and continence. Over time, chronic straining can contribute to several medical conditions:
- Hemorrhoids: Swollen veins in the lower rectum or anus caused by prolonged pressure.
- Anal fissures: Small tears in the anal lining, often resulting in pain and bleeding.
- Pelvic floor dysfunction: Weakening or improper coordination of pelvic muscles, leading to constipation, incontinence, or prolapse.
- Rectal prolapse: A condition where part of the rectum protrudes from the anus due to weakened supporting tissues.
- Increased risk of varicose veins and hernias: Elevated pressure can affect other vascular and muscular systems throughout the abdomen and legs.
These issues may start subtly but can escalate into chronic discomfort requiring medical intervention. The good news is that most cases of straining are avoidable with proper habits.
Why Do People Strain? Common Causes of Difficult Bowel Movements
Straining isn’t just about willpower—it’s usually a symptom of underlying factors affecting gut motility and stool consistency. Key contributors include:
- Inadequate fiber intake: Low-fiber diets produce small, hard stools that are difficult to pass.
- Dehydration: Without enough water, the colon absorbs excess moisture from waste, making stool dry and compacted.
- Sedentary lifestyle: Physical inactivity slows intestinal transit time.
- Ignoring the urge: Delaying bowel movements disrupts natural reflexes and allows stool to become harder.
- Poor toileting posture: Sitting upright on a standard toilet doesn't align the anorectal angle optimally for easy passage.
- Medications: Opioids, certain antidepressants, antacids containing aluminum, and iron supplements can cause constipation.
Addressing these root causes is far more effective than relying on laxatives or forceful evacuation.
How to Avoid Straining: A Step-by-Step Guide to Easier Elimination
Preventing straining requires consistent daily practices that support healthy digestion and efficient bowel function. Follow this timeline-based approach to make lasting improvements:
Step 1: Optimize Your Diet (Days 1–7)
Increase dietary fiber gradually to 25–35 grams per day using whole grains, legumes, fruits, and vegetables. Sudden spikes can cause bloating. Pair every gram of fiber with at least 8 ounces of water to keep stool soft.
Step 2: Hydrate Strategically (Ongoing)
Drink at least 6–8 glasses of water daily. Start your morning with a glass of warm water, which may stimulate colonic activity. Limit dehydrating beverages like coffee and alcohol.
Step 3: Adopt the Ideal Toileting Position (Immediate)
Use a small footstool to elevate your knees above your hips while seated. This mimics a squatting position, straightening the rectoanal canal and reducing strain by up to 70%, according to research published in *Digestive Diseases and Sciences*.
Step 4: Establish a Routine (Weeks 1–4)
Visit the bathroom at the same time each day—ideally 15–45 minutes after breakfast. The gastrocolic reflex triggered by eating helps initiate bowel movements naturally.
Step 5: Incorporate Movement (Daily)
Engage in at least 30 minutes of moderate exercise such as walking, cycling, or yoga. Physical activity stimulates peristalsis—the wave-like contractions that move stool through the intestines.
“Chronic straining is one of the most overlooked contributors to pelvic floor disorders. Patients often don’t realize they’re doing harm until symptoms become severe.” — Dr. Lena Patel, Gastroenterologist and Pelvic Floor Specialist
Do’s and Don’ts: Table of Best Practices
| Do’s | Don’ts |
|---|---|
| Eat high-fiber foods like oats, apples, beans, and leafy greens | Consume large amounts of low-fiber processed foods |
| Drink plenty of water throughout the day | Wait until you're thirsty to drink fluids |
| Use a footstool to improve toilet posture | Sit on the toilet for extended periods trying to force a bowel movement |
| Respond promptly when you feel the urge to go | Ignore or delay bowel urges regularly |
| Exercise daily to support gut motility | Lead a completely sedentary lifestyle |
Real-Life Example: Recovering from Chronic Straining
James, a 42-year-old office worker, began experiencing rectal pain and occasional bleeding after years of habitual straining. He often spent 15 minutes on the toilet each morning, sometimes feeling dizzy afterward from the effort. After seeing a gastroenterologist, he was diagnosed with internal hemorrhoids and early signs of pelvic floor dysfunction.
His treatment plan included adopting a squat-assist position using a footstool, increasing his fiber intake with psyllium husk, drinking two liters of water daily, and taking short walks after meals. Within three weeks, James reported significantly easier bowel movements without pain. By week six, his symptoms had nearly resolved, and follow-up evaluation showed reduced hemorrhoidal swelling.
This case illustrates how simple, non-invasive changes can reverse damage caused by chronic straining.
Checklist: Prevent Straining in 7 Daily Actions
- ✅ Consume at least 25g of fiber from whole foods
- ✅ Drink 6–8 glasses of water throughout the day
- ✅ Use a footstool to elevate legs while on the toilet
- ✅ Respond immediately to bowel urges
- ✅ Exercise for at least 30 minutes (e.g., brisk walk)
- ✅ Avoid holding your breath or clenching during defecation
- ✅ Limit time on the toilet to under 10 minutes
Frequently Asked Questions
Is it ever okay to push a little when pooping?
A gentle increase in abdominal pressure is normal and sometimes needed, especially after larger meals. However, forceful, prolonged straining—especially if accompanied by grunting, facial redness, or dizziness—is not safe and should be avoided.
Can children develop problems from straining?
Yes. Children who repeatedly strain may develop painful anal fissures or begin withholding stool out of fear, creating a cycle of worsening constipation. Encourage kids to use a stepstool and maintain a fiber-rich diet to prevent issues early.
What if I still can’t pass stool despite trying everything?
If lifestyle adjustments don’t improve bowel movements within 4–6 weeks, consult a healthcare provider. Underlying conditions such as irritable bowel syndrome (IBS), slow-transit constipation, or neurological disorders may require targeted treatment.
Take Control of Your Digestive Health Today
Straining to poop might seem like a minor inconvenience, but its long-term risks are significant. Hemorrhoids, pelvic floor damage, and chronic constipation don’t have to be inevitable. By adjusting your diet, hydration, posture, and daily routines, you can achieve comfortable, strain-free bowel movements.
Your body is designed to eliminate waste efficiently—when supported properly. Start applying these evidence-based strategies today. Your digestive system, pelvic health, and overall well-being will thank you.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?