In recent decades, a growing body of research has confirmed a quiet but significant trend: average testosterone levels in men are steadily declining. This isn't just a concern for aging athletes or those experiencing low libido—it affects metabolic health, mood stability, muscle maintenance, and long-term disease risk. Understanding why testosterone levels are dropping is essential not only for individual well-being but also for public health planning.
The decline isn’t solely due to aging. Studies show that even when controlling for age, modern men have lower testosterone than their counterparts from 30 or 40 years ago. The question is no longer whether levels are falling—but why, and what can be done about it.
Environmental and Lifestyle Factors Driving the Decline
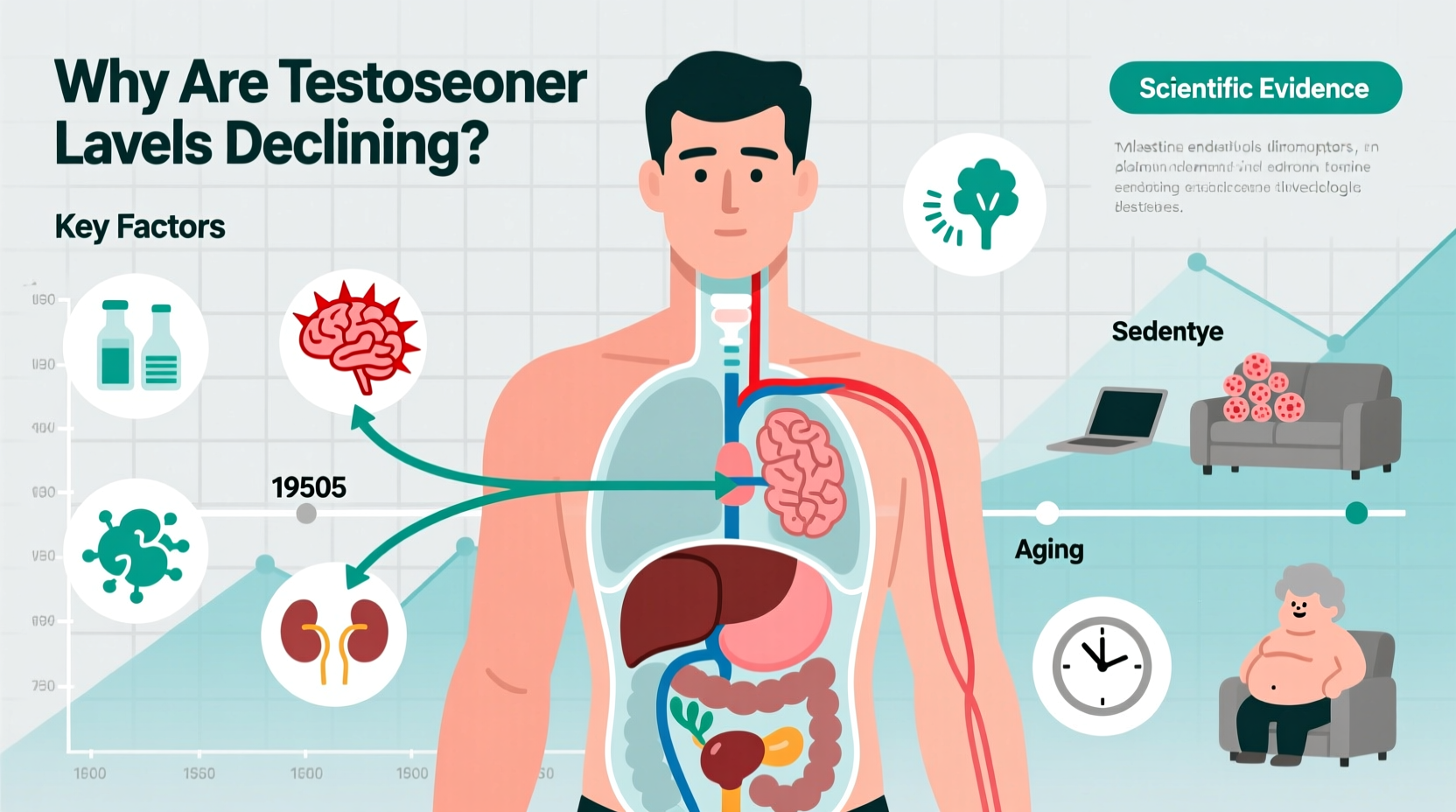
One of the most compelling explanations for falling testosterone lies in our changing environment and daily habits. Modern life exposes men to a combination of stressors that disrupt endocrine function—particularly the hypothalamic-pituitary-gonadal (HPG) axis, which regulates testosterone production.
- Endocrine-disrupting chemicals (EDCs): Found in plastics (like BPA and phthalates), pesticides, and personal care products, these compounds mimic or interfere with natural hormones. Phthalates, commonly used to soften plastics, are linked to reduced testosterone synthesis in both prenatal development and adult males.
- Sedentary behavior: Physical inactivity correlates strongly with lower testosterone. Exercise, especially resistance training, stimulates testosterone release. With desk jobs dominating the workforce, many men fail to engage in sufficient movement to maintain optimal hormone balance.
- Poor sleep quality: Testosterone is primarily produced during deep sleep stages. Chronic sleep deprivation or fragmented sleep—common in high-stress lifestyles—can suppress nightly testosterone surges by up to 15% after just one week.
- Dietary shifts: High intake of processed foods, refined sugars, and trans fats contributes to obesity and insulin resistance, both of which are associated with hypogonadism (low testosterone).
The Obesity Epidemic and Hormonal Feedback Loops
Obesity is one of the strongest predictors of low testosterone. Adipose (fat) tissue contains an enzyme called aromatase, which converts testosterone into estrogen. As body fat increases, particularly visceral fat around the abdomen, more testosterone is converted, leading to a double imbalance: lower testosterone and higher estrogen.
This creates a dangerous feedback loop. Low testosterone promotes further fat accumulation, especially in the abdominal region, which in turn drives more testosterone conversion to estrogen. Over time, this cycle accelerates metabolic dysfunction, increasing risks for type 2 diabetes, cardiovascular disease, and sexual dysfunction.
“Men with a waist circumference over 40 inches are three times more likely to have clinically low testosterone.” — Dr. Alan Hayes, Endocrinologist and Metabolic Researcher
Psychological Stress and Cortisol Interference
Chronic psychological stress plays a direct role in suppressing testosterone. When under constant pressure—whether from work, financial strain, or social instability—the body produces elevated levels of cortisol, the primary stress hormone.
Cortisol and testosterone have an inverse relationship. High cortisol inhibits luteinizing hormone (LH) secretion from the pituitary gland, which is necessary to signal the testes to produce testosterone. Long-term activation of the stress response essentially tells the body to prioritize survival over reproduction and anabolism.
A 2020 study published in Psychoneuroendocrinology found that men reporting high job strain had 12–18% lower total testosterone compared to those with low-stress occupations, independent of BMI and age.
Modern Exposure Timeline: How Daily Habits Affect Testosterone
Consider a typical day for an office worker in an urban setting:
- 6:30 AM: Wakes up after 5–6 hours of interrupted sleep due to screen use before bed.
- 7:00 AM: Eats a breakfast high in refined carbs (e.g., toast, jam, sugary coffee)—spiking insulin and promoting fat storage.
- 8:00 AM – 5:00 PM: Sits at a desk, drinks from a plastic water bottle containing BPA substitutes like BPS, and eats lunch from takeout containers lined with phthalates.
- 6:00 PM: Exercises rarely; instead scrolls through social media, increasing mental fatigue.
- 10:00 PM: Falls asleep late, exposed to blue light, restarting the cycle.
Each step contributes cumulatively to hormonal disruption. While none alone may cause immediate harm, repeated exposure over months and years leads to measurable declines in testosterone.
Actionable Checklist to Support Healthy Testosterone Levels
You don’t need drastic changes to make a difference. Implementing small, consistent habits can stabilize and even improve testosterone naturally. Here’s a practical checklist:
- ✅ Aim for 7–9 hours of quality sleep per night—maintain a cool, dark bedroom and avoid screens 60 minutes before bed.
- ✅ Perform strength training at least 3 times per week (focus on compound lifts: squats, deadlifts, bench press).
- ✅ Replace plastic food storage with glass or stainless steel to reduce EDC exposure.
- ✅ Eat whole foods rich in zinc (oysters, pumpkin seeds), vitamin D (fatty fish, egg yolks), and healthy fats (avocados, olive oil).
- ✅ Practice mindfulness or breathing exercises for 10 minutes daily to lower cortisol.
- ✅ Limit alcohol consumption—more than two drinks per day is linked to suppressed testosterone synthesis.
- ✅ Get sunlight exposure early in the day to regulate circadian rhythm and boost vitamin D.
Comparison Table: Lifestyle Factors and Their Impact on Testosterone
| Factor | Effect on Testosterone | Action Step |
|---|---|---|
| Sleep (less than 6 hours) | ↓ 10–15% reduction in one week | Maintain consistent sleep schedule |
| Resistance Training | ↑ Acute spikes + long-term elevation | Lift weights 3x/week |
| Body Fat >25% | ↓ Strongly correlated with low T | Focus on nutrition and activity |
| BPA/Phthalate Exposure | ↓ Disrupts hormone signaling | Avoid plastic containers and receipts |
| Vitamin D Deficiency | ↓ Linked to suboptimal T levels | Test levels; supplement if needed |
Real-Life Example: Reversing the Trend
Mark, a 42-year-old software developer, began noticing fatigue, weight gain around his midsection, and declining motivation. After a routine check-up, his doctor tested his hormones and found total testosterone at 280 ng/dL—below the normal range of 300–1000 ng/dL.
Instead of starting testosterone replacement therapy (TRT) immediately, Mark committed to lifestyle changes. He started sleeping 7.5 hours nightly, eliminated late-night screen use, began lifting weights twice a week, and replaced processed snacks with nuts, eggs, and vegetables. He also switched to a standing desk and spent 20 minutes outside each morning.
After six months, his follow-up test showed testosterone had risen to 460 ng/dL. His energy improved, he lost 18 pounds, and reported better focus and mood. His case illustrates that while environmental factors drive decline, targeted interventions can reverse the trend without medical intervention.
Frequently Asked Questions
Can low testosterone be reversed naturally?
Yes, in many cases—especially when linked to lifestyle factors such as poor sleep, inactivity, obesity, or stress. Addressing these root causes often restores testosterone to healthy levels without medication.
At what age do testosterone levels start to decline?
Testosterone begins to decline gradually around age 30, at a rate of about 1% per year. However, the pace and impact vary widely based on genetics, health behaviors, and environmental exposures.
Is testosterone replacement therapy (TRT) safe?
TRT can be effective for men with clinically diagnosed hypogonadism, but it carries risks including reduced sperm production, acne, fluid retention, and potential cardiovascular concerns. It should only be used under medical supervision after thorough testing.
Final Thoughts: Taking Control of Hormonal Health
The decline in testosterone levels is not inevitable. While modern life presents unique challenges—from chemical exposure to chronic stress—awareness and proactive choices can mitigate these effects. Hormonal health reflects overall health. By prioritizing sleep, movement, nutrition, and stress management, men can support robust testosterone levels well into later life.
It starts with recognizing that small daily decisions shape long-term outcomes. Whether you're in your 30s or 60s, the steps you take today influence your vitality, strength, and resilience tomorrow.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?